A newborn boy is evaluated on arrival in the nursery. He was born 3 hours ago by spontaneous vaginal delivery at 40 weeks gestation after an uncomplicated pregnancy. Apgar scores were 9 at 1 minute and 10 at 5 minutes after birth. His mother has no significant medical history and does not take any medications. Temperature is 36.7 C (98 F) , pulse is 124/min, and respirations are 26/min. He is awake, alert, and active with a strong cry. His head is normocephalic and atraumatic with an open flat anterior fontanelle. Pupils are equal and reactive to light and accommodation, and red reflexes are present bilaterally. The nares are patent, there is no cleft lip or palate, and the pharynx is not erythematous. Clavicles are intact without crepitus. S1 and S2 are normal without murmurs, and lungs are clear to auscultation bilaterally. The abdomen is soft, nontender, and nondistended with normal bowel sounds and no organomegaly. Femoral pulses are normal and symmetrical. All extremities move spontaneously and there is no edema. There are no rashes, skin lesions, or jaundice, but the complexion appears ruddy with generalized erythema. Blood samples obtained from the heel through simple prick method reveal a hematocrit of 70%. Repeat testing revealed a hematocrit of 65%. The patient is re-evaluated in the nursery and appears comfortable, with no tachycardia or respiratory distress. He feeds slowly but has no emesis, and voids spontaneously after his first feed. A decision is made to observe the child without intervention. Approximately 12 hours later, he appears irritable and lethargic. The infant has refused all subsequent feeds and has had decreased urine output. Nursery staff observed an episode of apnea. Temperature is 37.4 C (99.3 F) , pulse is 170/min, and respirations are 60/min. Physical examination shows a drowsy, hypotonic, poorly responsive newborn. The fontanelle is open and flat. Pupils are equal and reactive with normal red reflexes. There is no rhinorrhea. Oral mucosa is moist. S1 and S2 are present without murmurs. On pulmonary examination there are no wheezes or rales, but there are intercostal retractions. The skin is erythematous and ruddy, and there is cyanosis of the fingertips. There are no focal neurologic deficits. Laboratory results from peripheral blood draw are as follows: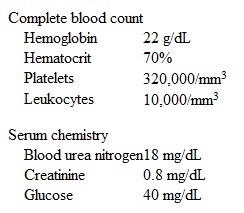 The patient is transferred to the neonatal intensive care unit, and treatment with intravenous fluids and glucose is initiated. His symptoms fail to improve, and his hematocrit after several hours is 71%. What is the most appropriate next step in management of this patient?
The patient is transferred to the neonatal intensive care unit, and treatment with intravenous fluids and glucose is initiated. His symptoms fail to improve, and his hematocrit after several hours is 71%. What is the most appropriate next step in management of this patient?
A) Chest x-ray
B) CT scan of the head
C) Echocardiography
D) Intravenous antibiotics
E) Partial exchange transfusion
Correct Answer:
Verified
Q478: A 52-year-old Caucasian woman comes to the
Q479: A 55-year-old Caucasian male is receiving doxorubicin-based
Q480: A 62-year-old hospitalized man is evaluated for
Q481: A 32-year-old female is seen for a
Q482: A 5-year-old boy is brought to the
Q484: A 30-year-old Caucasian man with no significant
Q485: A 4-year-old girl with sickle cell disease
Q486: A 45-year-old Caucasian female presents to your
Q487: A 45-year-old Caucasian female presents to your
Q488: A 50-year-old African American man comes to
Unlock this Answer For Free Now!
View this answer and more for free by performing one of the following actions

Scan the QR code to install the App and get 2 free unlocks

Unlock quizzes for free by uploading documents