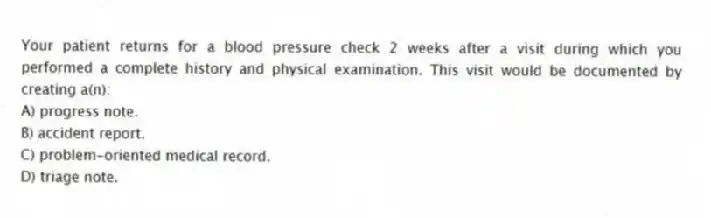
Your patient returns for a blood pressure check 2 weeks after a visit during which you performed a complete history and physical examination. This visit would be documented by creating a(n) :
A) progress note.
B) accident report.
C) problem-oriented medical record.
D) triage note.
Correct Answer:
Verified
Q13: A SOAP note is used in which
Q14: Differential diagnoses belong in the:
A) history.
B) physical
Q15: Drawing of stick figures is most useful
Q16: A detailed description of the symptoms related
Q17: The effect of the chief complaint on
Q19: A problem may be defined as anything
Q20: Which is an example of a problem
Q21: Which format would be used for visits
Q22: George Michaels, a 22-year-old patient, tells the
Q23: The examiner's evaluation of a patient's mental
Unlock this Answer For Free Now!
View this answer and more for free by performing one of the following actions

Scan the QR code to install the App and get 2 free unlocks

Unlock quizzes for free by uploading documents