
Clinical Laboratory Hematology 3rd Edition by Shirlyn McKenzie, Lynne Williams
النسخة 3الرقم المعياري الدولي: 978-0133076011
Clinical Laboratory Hematology 3rd Edition by Shirlyn McKenzie, Lynne Williams
النسخة 3الرقم المعياري الدولي: 978-0133076011 تمرين 11
Heidi, a 54-day-old female, was admitted to the hospital because of recurrent respiratory distress and failure to gain weight. She was born prematurely at 35 weeks gestation by urgent Cesarean section. Her mother was immune to rubella and had negative serologic tests for syphilis.
Consider why the lymphatic system should be evaluated in this child and the possible etiology of repeated respiratory problems.
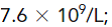
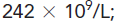
Admission CBC on Heidi was WBC: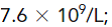
Hct: 0.55 L/L; Plt: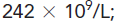
and differential: 84% segs, 2% bands, 4% lymphocytes, 8% monocytes, and 2% eosinophils.
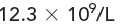
Heidi weighed 2 pounds 1 ounce at birth. Tests for CMV and toxoplasma infections were negative. At 4 days of age, she was transferred to a special facility for feeding and growth monitoring. She developed a diaper rash that failed to respond to many measures. No thrush was found. At 44 days, she developed pneumonia from coagulase-negative staphylococci that responded to antibiotics. Her WBC count was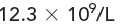
with a differential of segs 42%, bands 5%, lymphocytes 1%, monocytes 28%, eosinophils 23%, and basophils 1%.
All of Heidi's immunoglobulin levels were decreased. T and B lymphocyte counts were severely decreased. The peripheral blood smear showed anisocytosis, poikilocytosis (schistocytes), polychromatophilia, and two nucleated RBCs/100 WBCs. Her thymus was not detectable on chest films.
If she has a congenital immune deficiency, is it more likely that she has X-linked or autosomal SCIDS?
Consider why the lymphatic system should be evaluated in this child and the possible etiology of repeated respiratory problems.
Admission CBC on Heidi was WBC:
Hct: 0.55 L/L; Plt:
and differential: 84% segs, 2% bands, 4% lymphocytes, 8% monocytes, and 2% eosinophils.
Heidi weighed 2 pounds 1 ounce at birth. Tests for CMV and toxoplasma infections were negative. At 4 days of age, she was transferred to a special facility for feeding and growth monitoring. She developed a diaper rash that failed to respond to many measures. No thrush was found. At 44 days, she developed pneumonia from coagulase-negative staphylococci that responded to antibiotics. Her WBC count was
with a differential of segs 42%, bands 5%, lymphocytes 1%, monocytes 28%, eosinophils 23%, and basophils 1%.
All of Heidi's immunoglobulin levels were decreased. T and B lymphocyte counts were severely decreased. The peripheral blood smear showed anisocytosis, poikilocytosis (schistocytes), polychromatophilia, and two nucleated RBCs/100 WBCs. Her thymus was not detectable on chest films.
If she has a congenital immune deficiency, is it more likely that she has X-linked or autosomal SCIDS?
التوضيح
The patient's T and B lymphocyte count g...
Clinical Laboratory Hematology 3rd Edition by Shirlyn McKenzie, Lynne Williams
لماذا لم يعجبك هذا التمرين؟
أخرى 8 أحرف كحد أدنى و 255 حرفاً كحد أقصى
حرف 255








