Deck 24: Congenital Cardiac Defects
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question

Unlock Deck
Sign up to unlock the cards in this deck!
Unlock Deck
Unlock Deck
1/24
Play
Full screen (f)
Deck 24: Congenital Cardiac Defects
1
Which of the following blood flow patterns occurs in complete transposition of the great arteries?
A) The systemic venous blood passes through the right heart chambers.
B) The pulmonary venous blood traverses the left side of the heart and then returns to the systemic circulation.
C) When PVR increases relative to SVR, blood flow increases through the ductus arteriosus.
D) Systemic venous blood flows to the lungs after leaving the right ventricle.
A) The systemic venous blood passes through the right heart chambers.
B) The pulmonary venous blood traverses the left side of the heart and then returns to the systemic circulation.
C) When PVR increases relative to SVR, blood flow increases through the ductus arteriosus.
D) Systemic venous blood flows to the lungs after leaving the right ventricle.
A
Transposition of the great arteries (TGA) is a lesion in which the normal relationship between the ventricles and great arteries is inverted; the aorta arises from the RV, and the pulmonary artery arises from the LV (see Figure 24-17 in the textbook). The physiologic result of this is that the two circulations are in parallel rather than in series with each other. Deoxygenated systemic venous blood passes through the right side of the heart and to the body without flowing through the lungs. Oxygenated pulmonary venous blood passes through the left side of the heart and back to the lungs without flowing to the body. Survival depends on adequate mixing between the two circulations, most commonly occurring at the atrial level.
Transposition of the great arteries (TGA) is a lesion in which the normal relationship between the ventricles and great arteries is inverted; the aorta arises from the RV, and the pulmonary artery arises from the LV (see Figure 24-17 in the textbook). The physiologic result of this is that the two circulations are in parallel rather than in series with each other. Deoxygenated systemic venous blood passes through the right side of the heart and to the body without flowing through the lungs. Oxygenated pulmonary venous blood passes through the left side of the heart and back to the lungs without flowing to the body. Survival depends on adequate mixing between the two circulations, most commonly occurring at the atrial level.
2
Which of the following clinical features characterizes a critical aortic stenosis in a neonate?
A) Chest radiography reveals pleural effusion and pulmonary engorgement.
B) The neonate often has metabolic alkalosis.
C) The neonate presents in cardiogenic shock with hypotension.
D) These infants are rarely symptomatic during the first month of life.
A) Chest radiography reveals pleural effusion and pulmonary engorgement.
B) The neonate often has metabolic alkalosis.
C) The neonate presents in cardiogenic shock with hypotension.
D) These infants are rarely symptomatic during the first month of life.
C
The clinical presentation and natural history of aortic stenosis are determined primarily by the degree of stenosis. If not diagnosed prenatally, neonates with critical (i.e., dependent on PDA flow for survival) aortic stenosis may present in cardiogenic shock with hypotension, poor perfusion, and metabolic acidosis.
The clinical presentation and natural history of aortic stenosis are determined primarily by the degree of stenosis. If not diagnosed prenatally, neonates with critical (i.e., dependent on PDA flow for survival) aortic stenosis may present in cardiogenic shock with hypotension, poor perfusion, and metabolic acidosis.
3
How should the therapist interpret a preductal-to-postductal PaO2 difference of 8 mm Hg in a neonate?
A) Unreliable data
B) Absence of ductal shunting
C) Presence of ductal shunting
D) Inconclusive data
A) Unreliable data
B) Absence of ductal shunting
C) Presence of ductal shunting
D) Inconclusive data
B
Clinical signs of a PDA depend on the degree of left-to-right shunting but may include tachypnea and a continuous murmur. In addition to signs on examination, one can detect the presence of shunting by looking for a difference in oxygenation of preductal and postductal blood. A preductal blood gas should be obtained from the right radial or temporal artery, while a postductal gas may be obtained from the umbilical artery or from a peripheral artery in the lower extremity. A difference in PaO2 >15 mm Hg indicates significant shunting across the PDA.
Clinical signs of a PDA depend on the degree of left-to-right shunting but may include tachypnea and a continuous murmur. In addition to signs on examination, one can detect the presence of shunting by looking for a difference in oxygenation of preductal and postductal blood. A preductal blood gas should be obtained from the right radial or temporal artery, while a postductal gas may be obtained from the umbilical artery or from a peripheral artery in the lower extremity. A difference in PaO2 >15 mm Hg indicates significant shunting across the PDA.
4
Identify the following congenital cardiac anomaly: 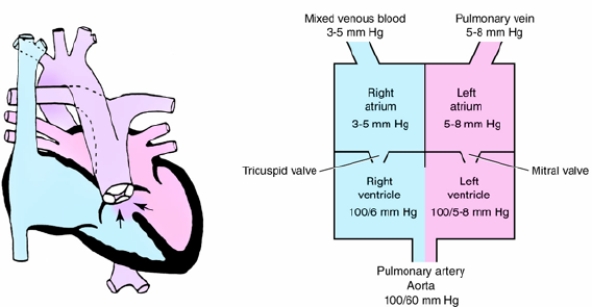
A) Truncus arteriosus
B) Hypoplastic left ventricle
C) Transposition of the great vessels
D) Ventricular septal defect
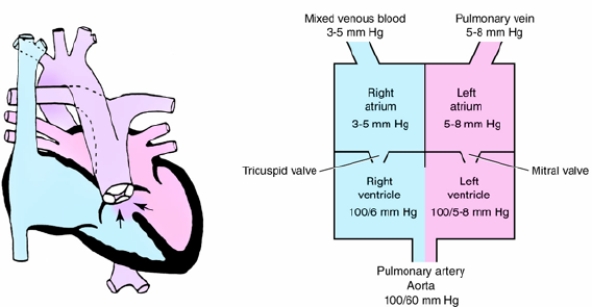
A) Truncus arteriosus
B) Hypoplastic left ventricle
C) Transposition of the great vessels
D) Ventricular septal defect

Unlock Deck
Unlock for access to all 24 flashcards in this deck.
Unlock Deck
k this deck
5
Which of the following vessels return blood to the right ventricle?
I). Pulmonary vein
II) Inferior vena cava
III) Superior vena cava
IV) Coronary sinus
A) I and IV only
B) II and III only
C) I, II, and III only
D) II, III, and IV only
I). Pulmonary vein
II) Inferior vena cava
III) Superior vena cava
IV) Coronary sinus
A) I and IV only
B) II and III only
C) I, II, and III only
D) II, III, and IV only

Unlock Deck
Unlock for access to all 24 flashcards in this deck.
Unlock Deck
k this deck
6
For which of the following congenital cardiac defects are considered ductal dependent, and closure of the ductus arteriosus could have catastrophic consequences for the patient?
I). Tetralogy of Fallot with pulmonary atresia
II) Atrial septal defect
III) Severe coarctation of the aorta
IV) Hypoplastic left heart syndrome
A) I and III only
B) III and IV only
C) I, II, and IV only
D) I, III, and IV only
I). Tetralogy of Fallot with pulmonary atresia
II) Atrial septal defect
III) Severe coarctation of the aorta
IV) Hypoplastic left heart syndrome
A) I and III only
B) III and IV only
C) I, II, and IV only
D) I, III, and IV only

Unlock Deck
Unlock for access to all 24 flashcards in this deck.
Unlock Deck
k this deck
7
Which of the following medications is the most common preoperative treatment to minimize preductal constriction until surgical correction of coarctation of the aorta can be achieved?
A) Indomethacin
B) Prostaglandin E1
C) Negative inotropes
D) Diuretics
A) Indomethacin
B) Prostaglandin E1
C) Negative inotropes
D) Diuretics

Unlock Deck
Unlock for access to all 24 flashcards in this deck.
Unlock Deck
k this deck
8
In patients with HLHS, which of the following are consequences if premature closure of the PDA occurs?
A) Metabolic alkalosis
B) Respiratory alkalosis
C) Hypertension
D) Hypoperfusion
A) Metabolic alkalosis
B) Respiratory alkalosis
C) Hypertension
D) Hypoperfusion

Unlock Deck
Unlock for access to all 24 flashcards in this deck.
Unlock Deck
k this deck
9
Identify the congenital cardiac defect depicted in the following illustration: 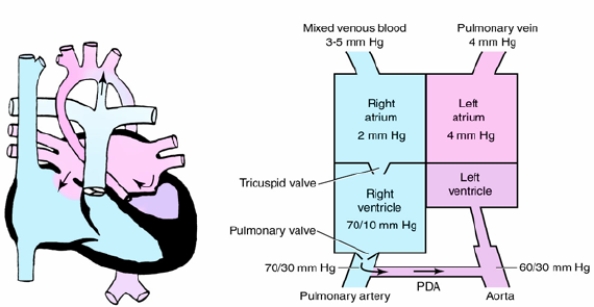
A) Atrial septal defect
B) Hypoplastic left ventricular syndrome
C) Hypoplastic right ventricular syndrome
D) Atrioventricular canal defect
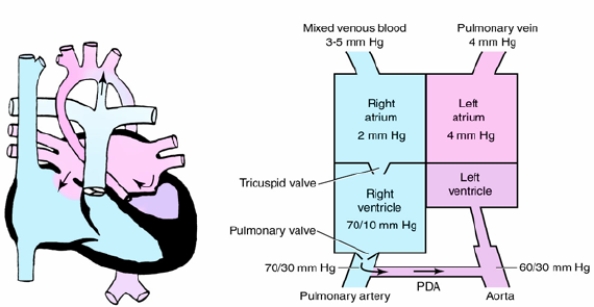
A) Atrial septal defect
B) Hypoplastic left ventricular syndrome
C) Hypoplastic right ventricular syndrome
D) Atrioventricular canal defect

Unlock Deck
Unlock for access to all 24 flashcards in this deck.
Unlock Deck
k this deck
10
Which of the following clinical manifestations is consistent with an atrial septal defect (ASD)?
A) An ASD often causes congestive heart failure.
B) The right ventricle may become hypertrophic.
C) Most patients with an ASD are symptomatic in the NICU, presenting with right atrial enlargement.
D) Chest radiographs are usually abnormal.
A) An ASD often causes congestive heart failure.
B) The right ventricle may become hypertrophic.
C) Most patients with an ASD are symptomatic in the NICU, presenting with right atrial enlargement.
D) Chest radiographs are usually abnormal.

Unlock Deck
Unlock for access to all 24 flashcards in this deck.
Unlock Deck
k this deck
11
What factor is responsible for closure of the foramen ovale?
A) Increased PaO2
B) Increased pressure on the left side of the heart
C) Blood flowing through the lungs
D) High pulmonary vascular resistance
A) Increased PaO2
B) Increased pressure on the left side of the heart
C) Blood flowing through the lungs
D) High pulmonary vascular resistance

Unlock Deck
Unlock for access to all 24 flashcards in this deck.
Unlock Deck
k this deck
12
A condition in which blood flow out of the right ventricle is obstructed because of atresia of the pulmonary valve is more consistent with which of the following defects?
A) Pulmonary atresia with intact ventricular septum
B) Coarctation of the aorta
C) Truncus arteriosus
D) Transposition of the great arteries
A) Pulmonary atresia with intact ventricular septum
B) Coarctation of the aorta
C) Truncus arteriosus
D) Transposition of the great arteries

Unlock Deck
Unlock for access to all 24 flashcards in this deck.
Unlock Deck
k this deck
13
Which of the following statements describe truncus arteriosus?
I) It is a rare defect in which a single great artery arises from the ventricles of the heart.
II) If PVR increases relative to systemic vascular resistance (SVR), more blood flows to the lungs through the truncus, decreasing systemic cardiac output.
III) Oxygen should be avoided in almost all circumstances in the preoperative setting.
IV) Patients may undergo complete biventricular repair in the newborn period.
A) I and III only
B) II and IV only
C) I, II, and IV only
D) I, III, and IV only
I) It is a rare defect in which a single great artery arises from the ventricles of the heart.
II) If PVR increases relative to systemic vascular resistance (SVR), more blood flows to the lungs through the truncus, decreasing systemic cardiac output.
III) Oxygen should be avoided in almost all circumstances in the preoperative setting.
IV) Patients may undergo complete biventricular repair in the newborn period.
A) I and III only
B) II and IV only
C) I, II, and IV only
D) I, III, and IV only

Unlock Deck
Unlock for access to all 24 flashcards in this deck.
Unlock Deck
k this deck
14
Which of the following is a risk if PVR decreases in the first days of life in infants with HLHS?
A) Pulmonary edema
B) Induce hypocapnia
C) Development of a VSD
D) Development of an ASD
A) Pulmonary edema
B) Induce hypocapnia
C) Development of a VSD
D) Development of an ASD

Unlock Deck
Unlock for access to all 24 flashcards in this deck.
Unlock Deck
k this deck
15
Which of the following clinical pathophysiologic manifestations are consistent with a large ventricular septal defect (VSD)?
I) The majority of the blood flow are shunted from left right to right left.
II) Shunting typically occurs during ventricular diastole, which causes left atrial enlargement.
III) Chest radiography reveals an enlarged cardiac silhouette and increased pulmonary vascular markings, increasing pulmonary blood flow.
IV) Thickening and fibrosing of the pulmonary veins develop, decreasing pulmonary artery pressure.
A) II and III only
B) I and IV only
C) I, II, and III only
D) II, III, and IV only
I) The majority of the blood flow are shunted from left right to right left.
II) Shunting typically occurs during ventricular diastole, which causes left atrial enlargement.
III) Chest radiography reveals an enlarged cardiac silhouette and increased pulmonary vascular markings, increasing pulmonary blood flow.
IV) Thickening and fibrosing of the pulmonary veins develop, decreasing pulmonary artery pressure.
A) II and III only
B) I and IV only
C) I, II, and III only
D) II, III, and IV only

Unlock Deck
Unlock for access to all 24 flashcards in this deck.
Unlock Deck
k this deck
16
Which of the following physiologic mechanisms needs to be in place to ensure adequate systemic perfusion in infants with HLHS?
A) Presence of an ASD
B) Presence of a mitral regurgitation
C) Adequate left atrial function
D) Presence of an PDA
A) Presence of an ASD
B) Presence of a mitral regurgitation
C) Adequate left atrial function
D) Presence of an PDA

Unlock Deck
Unlock for access to all 24 flashcards in this deck.
Unlock Deck
k this deck
17
Why must supplemental oxygen be judiciously administered to patients with an atrioventricular canal defect?
A) To prevent the development of retinopathy of prematurity
B) To avoid oxygen-induced hypoventilation
C) To minimize pulmonary vascular dilation
D) To reduce oxidative stress
A) To prevent the development of retinopathy of prematurity
B) To avoid oxygen-induced hypoventilation
C) To minimize pulmonary vascular dilation
D) To reduce oxidative stress

Unlock Deck
Unlock for access to all 24 flashcards in this deck.
Unlock Deck
k this deck
18
At birth, what factor causes dilation of the pulmonary vascular bed and a decrease in the pulmonary vascular resistance?
A) Increased PaO2
B) Decreased PaCO2
C) Lung inflation
D) Circulating indomethacin
A) Increased PaO2
B) Decreased PaCO2
C) Lung inflation
D) Circulating indomethacin

Unlock Deck
Unlock for access to all 24 flashcards in this deck.
Unlock Deck
k this deck
19
Which of the following methods is involved in the management of a PDA?
A) Increasing the circulating volume
B) Maintaining/optimizing the hematocrit at the low end of normal hemoglobin level
C) Administering indomethacin
D) Administering digoxin
A) Increasing the circulating volume
B) Maintaining/optimizing the hematocrit at the low end of normal hemoglobin level
C) Administering indomethacin
D) Administering digoxin

Unlock Deck
Unlock for access to all 24 flashcards in this deck.
Unlock Deck
k this deck
20
The therapist is treating a child with TOF who appears to be having a "spell." What should the therapist suggest to treat this event?
I) Prone positioning
II) Knee-chest position to increase SVR
III) Morphine sulfate
IV) Oxygen
A) II and IV only
B) I and III only
C) I and IV only
D) II, III, and IV only
I) Prone positioning
II) Knee-chest position to increase SVR
III) Morphine sulfate
IV) Oxygen
A) II and IV only
B) I and III only
C) I and IV only
D) II, III, and IV only

Unlock Deck
Unlock for access to all 24 flashcards in this deck.
Unlock Deck
k this deck
21
Low signal strength on a plethysmogram may indicate which of the following?
A) Hyperperfusion
B) Increased stroke volume
C) Probe malposition
D) Decreased SVR
A) Hyperperfusion
B) Increased stroke volume
C) Probe malposition
D) Decreased SVR

Unlock Deck
Unlock for access to all 24 flashcards in this deck.
Unlock Deck
k this deck
22
A therapist monitoring an infant after a Blalock-Tausig shunt placement notices a significant drop in the end-tidal carbon dioxide (ETCO2) despite no changes in the infant's respiratory rate. How should the therapist interpret this change?
A) The infant has dramatically improved ventilation by breathing deeply.
B) The ETCO2 monitor is not accurate.
C) Loss of pulmonary blood flow through the shunt.
D) Tricuspid regurgitation.
A) The infant has dramatically improved ventilation by breathing deeply.
B) The ETCO2 monitor is not accurate.
C) Loss of pulmonary blood flow through the shunt.
D) Tricuspid regurgitation.

Unlock Deck
Unlock for access to all 24 flashcards in this deck.
Unlock Deck
k this deck
23
The therapist is monitoring a patient in the CICU with a cardiac abnormality. They notice a narrowing pulse pressure. Which of the following could result?
I) A low stroke volume
II) Increased cardiac output
III) Poor ventricular function
IV) Impaired venous return
A) I and III only
B) II and IV only
C) I, II, and IV only
D) I, III, and IV only
I) A low stroke volume
II) Increased cardiac output
III) Poor ventricular function
IV) Impaired venous return
A) I and III only
B) II and IV only
C) I, II, and IV only
D) I, III, and IV only

Unlock Deck
Unlock for access to all 24 flashcards in this deck.
Unlock Deck
k this deck
24
Which of the following is the correct statement regarding the path of blood as it travels through the heart?
A) During ventricular diastole, blood passes through the tricuspid valve and into the left ventricle (LV).
B) During ventricular diastole, blood is ejected from the RV into the pulmonary arteries through the pulmonary valve.
C) During ventricular systole, blood is pumped from the RA into the right ventricle (RV) via the mitral valve (TV).
D) The coronary sinus drains venous blood supplying the heart muscle itself.
A) During ventricular diastole, blood passes through the tricuspid valve and into the left ventricle (LV).
B) During ventricular diastole, blood is ejected from the RV into the pulmonary arteries through the pulmonary valve.
C) During ventricular systole, blood is pumped from the RA into the right ventricle (RV) via the mitral valve (TV).
D) The coronary sinus drains venous blood supplying the heart muscle itself.

Unlock Deck
Unlock for access to all 24 flashcards in this deck.
Unlock Deck
k this deck



