Deck 65: Nursing Management: Arthritis and Connective Tissue Diseases
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question

Unlock Deck
Sign up to unlock the cards in this deck!
Unlock Deck
Unlock Deck
1/22
Play
Full screen (f)
Deck 65: Nursing Management: Arthritis and Connective Tissue Diseases
1
In assessing the joints of a patient with osteoarthritis, the nurse understands that Heberden's nodes
A) are often red, swollen, and tender.
B) indicate osteophyte formation at the DIP joints.
C) are the result of pannus formation at the PIP joints.
D) occur from deterioration of cartilage by proteolytic enzymes.
A) are often red, swollen, and tender.
B) indicate osteophyte formation at the DIP joints.
C) are the result of pannus formation at the PIP joints.
D) occur from deterioration of cartilage by proteolytic enzymes.
Osteoarthritis is a condition that occurs as a result of damage of cartilage that tends to initiate formation of new joint tissues. Heberden's nodes are not normally found in the body and are not formed due to pannus formation or deterioration of the cartilage.
Hence, the options (a), (c) and (d) are incorrect.
Heberden's nodes are bony deformities found in the distal interphalangeal (DIP) joints indicating formation of osteophyte and loss of joint space in osteoarthritis.
Hence, the option (b) is correct.
Hence, the options (a), (c) and (d) are incorrect.
Heberden's nodes are bony deformities found in the distal interphalangeal (DIP) joints indicating formation of osteophyte and loss of joint space in osteoarthritis.
Hence, the option (b) is correct.
2
Patient Profile
K.R., a 42-yr-old married white woman, is seen at the rheumatology clinic with complaints of tenderness and pain in the small joints of her hands.
Subjective Data
• Complains of tenderness, joint pain, and stiffness in her hands for the last 3 mo
• Experiencing fatigue, anorexia, and morning stiffness
• Mother diagnosed with ankylosing spondylitis 8 yr ago
• Expresses doubt about her ability to manage disease
Objective Data
Physical Examination
• Swelling, warmth, and tenderness of third and fourth metacarpophalangeal joints of both hands
• Mild pain with neck motion
• Tenosynovitis
Diagnostic Studies
• Positive ESR, RF, and ACPA
• Moderate bone demineralization evident bilaterally in hand x-rays
Collaborative Care
• Diagnosed with RA
• Started on methotrexate (Rheumatrex) 7.5 mg PO once per week, etanercept (Enbrel) 50 mg subcutaneously once per week, prednisone 10 mg/day
1. How will you explain the pathophysiology of RA to K.R.
2. K.R. asks you if genetic factors are related to a diagnosis of RA. How will you respond
3. What are some home and work modifications that you can suggest to K.R. to reduce her symptoms
4. What suggestions can you make to K.R. about coping with fatigue
5. Priority Decision: Based on the assessment data presented, what are the priority nursing diagnoses Are there any collaborative problems
6. Evidence-Based Practice: Why is an exercise program important in the treatment plan for K.R.
K.R., a 42-yr-old married white woman, is seen at the rheumatology clinic with complaints of tenderness and pain in the small joints of her hands.
Subjective Data
• Complains of tenderness, joint pain, and stiffness in her hands for the last 3 mo
• Experiencing fatigue, anorexia, and morning stiffness
• Mother diagnosed with ankylosing spondylitis 8 yr ago
• Expresses doubt about her ability to manage disease
Objective Data
Physical Examination
• Swelling, warmth, and tenderness of third and fourth metacarpophalangeal joints of both hands
• Mild pain with neck motion
• Tenosynovitis
Diagnostic Studies
• Positive ESR, RF, and ACPA
• Moderate bone demineralization evident bilaterally in hand x-rays
Collaborative Care
• Diagnosed with RA
• Started on methotrexate (Rheumatrex) 7.5 mg PO once per week, etanercept (Enbrel) 50 mg subcutaneously once per week, prednisone 10 mg/day
1. How will you explain the pathophysiology of RA to K.R.
2. K.R. asks you if genetic factors are related to a diagnosis of RA. How will you respond
3. What are some home and work modifications that you can suggest to K.R. to reduce her symptoms
4. What suggestions can you make to K.R. about coping with fatigue
5. Priority Decision: Based on the assessment data presented, what are the priority nursing diagnoses Are there any collaborative problems
6. Evidence-Based Practice: Why is an exercise program important in the treatment plan for K.R.
1.
The pathophysiology of rheumatoid arthritis can be explained to K.R. rheumatoid arthritis is an autoimmune disease caused by the abnormal growth of the immunoglobulin G (IgG) due to entry of some antigen (virus/bacteria); thereby, causing production of autoantibodies (RF) against the production of IgG. There is formation of immune complexes by combination of RF and IgG which gets deposited over the superficial articular cartilage or synovial membrane in joints; thereby activating inflammatory response.
2.
The genetic factors associated with rheumatoid arthritis including more occurrence of condition in identical twins than fraternal twins. There is a possible genetic link of rheumatoid arthritis in R.A. due to the diagnosis of ankylosing spondylitis of her mother as the genetic basis of the two condition shares the involvement of human leukocyte antigen.
3.
The suggested modifications at home and work for K.R. include relieving from morning stiffness by soaking the hands in warm water or by taking warm shower. At work, the patient can take breaks in between to avoid any fatigue and pain. Material and supplies that are used more often should be placed in carts present in easily reached place. The patient should wear shoes with Velcro fasteners and clothes with zippers or buttons in front side to prevent stress on joints.
4.
The patient should be advised to incorporate short rest periods during their activities all throughout the day for relieving pain and fatigue. The nurse should assist K.R. in modification of activities of daily living to reduce fatigue. Teaching about proper alignment of body while resting can also help the patient.
5.
The priority nursing diagnosis includes chronic pain, disturbed image of body, impaired physical mobility and fatigue. The collaborative problems of rheumatoid arthritis include deformities of hands, contractures of flexion and side effects of corticosteroids.
6.
It is important to include an individualized exercise plan for treating the patients with rheumatoid arthritis because exercises can help in improving the strength of the patient. Several studies have shown the quality of life and functioning of body can be improved significantly by following a home-based exercise program.
The pathophysiology of rheumatoid arthritis can be explained to K.R. rheumatoid arthritis is an autoimmune disease caused by the abnormal growth of the immunoglobulin G (IgG) due to entry of some antigen (virus/bacteria); thereby, causing production of autoantibodies (RF) against the production of IgG. There is formation of immune complexes by combination of RF and IgG which gets deposited over the superficial articular cartilage or synovial membrane in joints; thereby activating inflammatory response.
2.
The genetic factors associated with rheumatoid arthritis including more occurrence of condition in identical twins than fraternal twins. There is a possible genetic link of rheumatoid arthritis in R.A. due to the diagnosis of ankylosing spondylitis of her mother as the genetic basis of the two condition shares the involvement of human leukocyte antigen.
3.
The suggested modifications at home and work for K.R. include relieving from morning stiffness by soaking the hands in warm water or by taking warm shower. At work, the patient can take breaks in between to avoid any fatigue and pain. Material and supplies that are used more often should be placed in carts present in easily reached place. The patient should wear shoes with Velcro fasteners and clothes with zippers or buttons in front side to prevent stress on joints.
4.
The patient should be advised to incorporate short rest periods during their activities all throughout the day for relieving pain and fatigue. The nurse should assist K.R. in modification of activities of daily living to reduce fatigue. Teaching about proper alignment of body while resting can also help the patient.
5.
The priority nursing diagnosis includes chronic pain, disturbed image of body, impaired physical mobility and fatigue. The collaborative problems of rheumatoid arthritis include deformities of hands, contractures of flexion and side effects of corticosteroids.
6.
It is important to include an individualized exercise plan for treating the patients with rheumatoid arthritis because exercises can help in improving the strength of the patient. Several studies have shown the quality of life and functioning of body can be improved significantly by following a home-based exercise program.
3
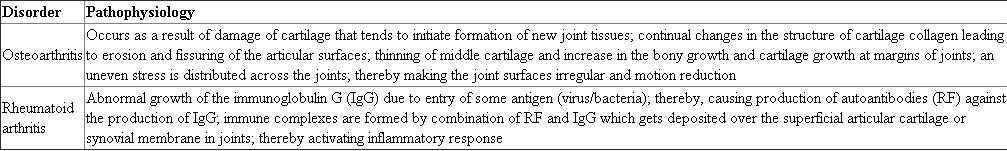
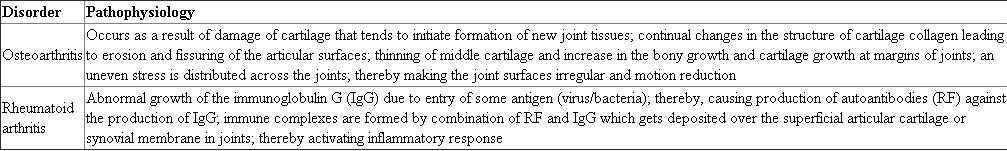
Compare and contrast the sequence of events leading to joint destruction in osteoarthritis and rheumatoid arthritis.
The difference between the events leading to the destruction of joints in osteoarthritis and rheumatoid arthritis are listed below:
4
You are working on the medical-surgical unit and have been assigned to care for the following five patients. You have one LPN and one UAP on your team to help you.
Patients
A.J. is a 66-yr-old white woman who had an ischemic stroke 2 days ago. She has a history of migraines, hypertension, and atrial fibrillation. She is alert, oriented, and able to answer questions appropriately but has mild slowness in responding. She has left-sided arm weakness (3/5) and left leg weakness (4/5). Her vital signs are BP 160/84, HR 88, RR 20, T 37° C. She is receiving ASA 325 mg po daily, Lovenox 80 mg subcutaneously q12hr, lisinopril 10 mg po daily, Cardizem CD 180 mg po daily, and Coumadin 5 mg po daily. Her most recent INR was 1.7. She is scheduled to receive physical therapy today.
J.P. is a 24-yr-old woman who fell and hit her head after experiencing a tonic-clonic seizure. Her boyfriend found her lying semiconscious on the floor in her apartment. She had an emergency evacuation of a subdural hematoma and was initially admitted to the ICU. She was transferred to the medical-surgical unit yesterday and is scheduled for rehabilitation evaluation. She is oriented to person only and is somewhat restless. A safety sitter is with her at all times.
M.Y., an 80-yr-old Asian American man, had an ORIF 2 days ago for a fractured left hip. He has a 3-yr history of Alzheimer's disease and is confused to place and time. Although he has a history of agitation, he has been pleasant and cooperative. He has a personal alarm and bed alarm on for safety. His hip dressing is dry and intact and the drainage in the hemovac is minimal.
B.V., a 24-yr-old white man, was admitted to the ICU 3 weeks ago after suffering a C5-6 cervical spinal cord injury. B.V. dove into the shallow end of a neighbor's backyard pool and struck his head on the bottom. He was initially placed in cervical traction, intubated, and mechanically ventilated. He has since undergone surgical stabilization and the traction was removed. He was weaned from the ventilator 2 days ago. He was transferred to the medical-surgical unit yesterday. He is currently requesting medication for a "severe headache."
M.L. is a 58-yr-old white retired nurse who suffered an L4 compression fracture after falling 1 week ago. She underwent vertebroplasty yesterday and was kept in the hospital overnight for observation after experiencing some postoperative hypotension. She has a 6-yr history of Addison's disease. She is planning to be discharged home today.
Priority Decision: After receiving report, which patient should you see first Provide a rationale.
Patients
A.J. is a 66-yr-old white woman who had an ischemic stroke 2 days ago. She has a history of migraines, hypertension, and atrial fibrillation. She is alert, oriented, and able to answer questions appropriately but has mild slowness in responding. She has left-sided arm weakness (3/5) and left leg weakness (4/5). Her vital signs are BP 160/84, HR 88, RR 20, T 37° C. She is receiving ASA 325 mg po daily, Lovenox 80 mg subcutaneously q12hr, lisinopril 10 mg po daily, Cardizem CD 180 mg po daily, and Coumadin 5 mg po daily. Her most recent INR was 1.7. She is scheduled to receive physical therapy today.
J.P. is a 24-yr-old woman who fell and hit her head after experiencing a tonic-clonic seizure. Her boyfriend found her lying semiconscious on the floor in her apartment. She had an emergency evacuation of a subdural hematoma and was initially admitted to the ICU. She was transferred to the medical-surgical unit yesterday and is scheduled for rehabilitation evaluation. She is oriented to person only and is somewhat restless. A safety sitter is with her at all times.
M.Y., an 80-yr-old Asian American man, had an ORIF 2 days ago for a fractured left hip. He has a 3-yr history of Alzheimer's disease and is confused to place and time. Although he has a history of agitation, he has been pleasant and cooperative. He has a personal alarm and bed alarm on for safety. His hip dressing is dry and intact and the drainage in the hemovac is minimal.
B.V., a 24-yr-old white man, was admitted to the ICU 3 weeks ago after suffering a C5-6 cervical spinal cord injury. B.V. dove into the shallow end of a neighbor's backyard pool and struck his head on the bottom. He was initially placed in cervical traction, intubated, and mechanically ventilated. He has since undergone surgical stabilization and the traction was removed. He was weaned from the ventilator 2 days ago. He was transferred to the medical-surgical unit yesterday. He is currently requesting medication for a "severe headache."
M.L. is a 58-yr-old white retired nurse who suffered an L4 compression fracture after falling 1 week ago. She underwent vertebroplasty yesterday and was kept in the hospital overnight for observation after experiencing some postoperative hypotension. She has a 6-yr history of Addison's disease. She is planning to be discharged home today.
Priority Decision: After receiving report, which patient should you see first Provide a rationale.

Unlock Deck
Unlock for access to all 22 flashcards in this deck.
Unlock Deck
k this deck
5
A patient with rheumatoid arthritis is experiencing articular involvement of the joints. The nurse recognizes that these characteristic changes include (select all that apply)
A) bamboo-shaped fingers.
B) metatarsal head dislocation in feet.
C) noninflammatory pain in large joints.
D) asymmetric involvement of small joints.
E) morning stiffness lasting 60 minutes or more.
A) bamboo-shaped fingers.
B) metatarsal head dislocation in feet.
C) noninflammatory pain in large joints.
D) asymmetric involvement of small joints.
E) morning stiffness lasting 60 minutes or more.

Unlock Deck
Unlock for access to all 22 flashcards in this deck.
Unlock Deck
k this deck
6
Detail the clinical manifestations, collaborative care, and nursing management of osteoarthritis and rheumatoid arthritis.

Unlock Deck
Unlock for access to all 22 flashcards in this deck.
Unlock Deck
k this deck
7
You are working on the medical-surgical unit and have been assigned to care for the following five patients. You have one LPN and one UAP on your team to help you.
Patients
A)J. is a 66-yr-old white woman who had an ischemic stroke 2 days ago. She has a history of migraines, hypertension, and atrial fibrillation. She is alert, oriented, and able to answer questions appropriately but has mild slowness in responding. She has left-sided arm weakness (3/5) and left leg weakness (4/5). Her vital signs are BP 160/84, HR 88, RR 20, T 37° C. She is receiving ASA 325 mg po daily, Lovenox 80 mg subcutaneously q12hr, lisinopril 10 mg po daily, Cardizem CD 180 mg po daily, and Coumadin 5 mg po daily. Her most recent INR was 1.7. She is scheduled to receive physical therapy today.
J)P. is a 24-yr-old woman who fell and hit her head after experiencing a tonic-clonic seizure. Her boyfriend found her lying semiconscious on the floor in her apartment. She had an emergency evacuation of a subdural hematoma and was initially admitted to the ICU. She was transferred to the medical-surgical unit yesterday and is scheduled for rehabilitation evaluation. She is oriented to person only and is somewhat restless. A safety sitter is with her at all times.
M)Y., an 80-yr-old Asian American man, had an ORIF 2 days ago for a fractured left hip. He has a 3-yr history of Alzheimer's disease and is confused to place and time. Although he has a history of agitation, he has been pleasant and cooperative. He has a personal alarm and bed alarm on for safety. His hip dressing is dry and intact and the drainage in the hemovac is minimal.
B)V., a 24-yr-old white man, was admitted to the ICU 3 weeks ago after suffering a C5-6 cervical spinal cord injury. B.V. dove into the shallow end of a neighbor's backyard pool and struck his head on the bottom. He was initially placed in cervical traction, intubated, and mechanically ventilated. He has since undergone surgical stabilization and the traction was removed. He was weaned from the ventilator 2 days ago. He was transferred to the medical-surgical unit yesterday. He is currently requesting medication for a "severe headache."
M)L. is a 58-yr-old white retired nurse who suffered an L4 compression fracture after falling 1 week ago. She underwent vertebroplasty yesterday and was kept in the hospital overnight for observation after experiencing some postoperative hypotension. She has a 6-yr history of Addison's disease. She is planning to be discharged home today.
Delegation Decision: Which tasks could you delegate to UAP (select all that apply)
A) Explain discharge instructions to M.L.
B) Change the dressing on M.Y.'s left hip.
C) Obtain vital signs on M.L. before discharge.
D) Sit with J.P. while the safety sitter takes a break.
E) Assess A.J.'s ability to swallow before feeding her breakfast.
Patients
A)J. is a 66-yr-old white woman who had an ischemic stroke 2 days ago. She has a history of migraines, hypertension, and atrial fibrillation. She is alert, oriented, and able to answer questions appropriately but has mild slowness in responding. She has left-sided arm weakness (3/5) and left leg weakness (4/5). Her vital signs are BP 160/84, HR 88, RR 20, T 37° C. She is receiving ASA 325 mg po daily, Lovenox 80 mg subcutaneously q12hr, lisinopril 10 mg po daily, Cardizem CD 180 mg po daily, and Coumadin 5 mg po daily. Her most recent INR was 1.7. She is scheduled to receive physical therapy today.
J)P. is a 24-yr-old woman who fell and hit her head after experiencing a tonic-clonic seizure. Her boyfriend found her lying semiconscious on the floor in her apartment. She had an emergency evacuation of a subdural hematoma and was initially admitted to the ICU. She was transferred to the medical-surgical unit yesterday and is scheduled for rehabilitation evaluation. She is oriented to person only and is somewhat restless. A safety sitter is with her at all times.
M)Y., an 80-yr-old Asian American man, had an ORIF 2 days ago for a fractured left hip. He has a 3-yr history of Alzheimer's disease and is confused to place and time. Although he has a history of agitation, he has been pleasant and cooperative. He has a personal alarm and bed alarm on for safety. His hip dressing is dry and intact and the drainage in the hemovac is minimal.
B)V., a 24-yr-old white man, was admitted to the ICU 3 weeks ago after suffering a C5-6 cervical spinal cord injury. B.V. dove into the shallow end of a neighbor's backyard pool and struck his head on the bottom. He was initially placed in cervical traction, intubated, and mechanically ventilated. He has since undergone surgical stabilization and the traction was removed. He was weaned from the ventilator 2 days ago. He was transferred to the medical-surgical unit yesterday. He is currently requesting medication for a "severe headache."
M)L. is a 58-yr-old white retired nurse who suffered an L4 compression fracture after falling 1 week ago. She underwent vertebroplasty yesterday and was kept in the hospital overnight for observation after experiencing some postoperative hypotension. She has a 6-yr history of Addison's disease. She is planning to be discharged home today.
Delegation Decision: Which tasks could you delegate to UAP (select all that apply)
A) Explain discharge instructions to M.L.
B) Change the dressing on M.Y.'s left hip.
C) Obtain vital signs on M.L. before discharge.
D) Sit with J.P. while the safety sitter takes a break.
E) Assess A.J.'s ability to swallow before feeding her breakfast.

Unlock Deck
Unlock for access to all 22 flashcards in this deck.
Unlock Deck
k this deck
8
When administering medications to the patient with gout, the nurse would recognize that which drug is used as a treatment for this disease
A) Colchicine
B) Febuxostat
C) Sulfasalazine
D) Cyclosporine
A) Colchicine
B) Febuxostat
C) Sulfasalazine
D) Cyclosporine

Unlock Deck
Unlock for access to all 22 flashcards in this deck.
Unlock Deck
k this deck
9
Describe the pathophysiology, clinical manifestations, and collaborative care of gout, Lyme disease, and septic arthritis.

Unlock Deck
Unlock for access to all 22 flashcards in this deck.
Unlock Deck
k this deck
10
You are working on the medical-surgical unit and have been assigned to care for the following five patients. You have one LPN and one UAP on your team to help you.
Patients
A)J. is a 66-yr-old white woman who had an ischemic stroke 2 days ago. She has a history of migraines, hypertension, and atrial fibrillation. She is alert, oriented, and able to answer questions appropriately but has mild slowness in responding. She has left-sided arm weakness (3/5) and left leg weakness (4/5). Her vital signs are BP 160/84, HR 88, RR 20, T 37° C. She is receiving ASA 325 mg po daily, Lovenox 80 mg subcutaneously q12hr, lisinopril 10 mg po daily, Cardizem CD 180 mg po daily, and Coumadin 5 mg po daily. Her most recent INR was 1.7. She is scheduled to receive physical therapy today.
J)P. is a 24-yr-old woman who fell and hit her head after experiencing a tonic-clonic seizure. Her boyfriend found her lying semiconscious on the floor in her apartment. She had an emergency evacuation of a subdural hematoma and was initially admitted to the ICU. She was transferred to the medical-surgical unit yesterday and is scheduled for rehabilitation evaluation. She is oriented to person only and is somewhat restless. A safety sitter is with her at all times.
M)Y., an 80-yr-old Asian American man, had an ORIF 2 days ago for a fractured left hip. He has a 3-yr history of Alzheimer's disease and is confused to place and time. Although he has a history of agitation, he has been pleasant and cooperative. He has a personal alarm and bed alarm on for safety. His hip dressing is dry and intact and the drainage in the hemovac is minimal.
B)V., a 24-yr-old white man, was admitted to the ICU 3 weeks ago after suffering a C5-6 cervical spinal cord injury. B.V. dove into the shallow end of a neighbor's backyard pool and struck his head on the bottom. He was initially placed in cervical traction, intubated, and mechanically ventilated. He has since undergone surgical stabilization and the traction was removed. He was weaned from the ventilator 2 days ago. He was transferred to the medical-surgical unit yesterday. He is currently requesting medication for a "severe headache."
M)L. is a 58-yr-old white retired nurse who suffered an L4 compression fracture after falling 1 week ago. She underwent vertebroplasty yesterday and was kept in the hospital overnight for observation after experiencing some postoperative hypotension. She has a 6-yr history of Addison's disease. She is planning to be discharged home today.
Priority and Delegation Decision: When you enter the room to assess B.V., you find him diaphoretic with a flushed face and pale extremities. His BP is 200/102 mm Hg. Which two initial actions would be most appropriate
A) Ask the UAP to obtain a stat bladder scan.
B) Have the LPN administer his oral antihypertensive meds stat.
C) Elevate the head of the bed while assessing for any noxious stimuli.
D) Ask the LPN to stay with B.V. while you call B.V.'s health care provider.
E) Insert rectal suppository after applying lidocaine to the area around the rectum.
Patients
A)J. is a 66-yr-old white woman who had an ischemic stroke 2 days ago. She has a history of migraines, hypertension, and atrial fibrillation. She is alert, oriented, and able to answer questions appropriately but has mild slowness in responding. She has left-sided arm weakness (3/5) and left leg weakness (4/5). Her vital signs are BP 160/84, HR 88, RR 20, T 37° C. She is receiving ASA 325 mg po daily, Lovenox 80 mg subcutaneously q12hr, lisinopril 10 mg po daily, Cardizem CD 180 mg po daily, and Coumadin 5 mg po daily. Her most recent INR was 1.7. She is scheduled to receive physical therapy today.
J)P. is a 24-yr-old woman who fell and hit her head after experiencing a tonic-clonic seizure. Her boyfriend found her lying semiconscious on the floor in her apartment. She had an emergency evacuation of a subdural hematoma and was initially admitted to the ICU. She was transferred to the medical-surgical unit yesterday and is scheduled for rehabilitation evaluation. She is oriented to person only and is somewhat restless. A safety sitter is with her at all times.
M)Y., an 80-yr-old Asian American man, had an ORIF 2 days ago for a fractured left hip. He has a 3-yr history of Alzheimer's disease and is confused to place and time. Although he has a history of agitation, he has been pleasant and cooperative. He has a personal alarm and bed alarm on for safety. His hip dressing is dry and intact and the drainage in the hemovac is minimal.
B)V., a 24-yr-old white man, was admitted to the ICU 3 weeks ago after suffering a C5-6 cervical spinal cord injury. B.V. dove into the shallow end of a neighbor's backyard pool and struck his head on the bottom. He was initially placed in cervical traction, intubated, and mechanically ventilated. He has since undergone surgical stabilization and the traction was removed. He was weaned from the ventilator 2 days ago. He was transferred to the medical-surgical unit yesterday. He is currently requesting medication for a "severe headache."
M)L. is a 58-yr-old white retired nurse who suffered an L4 compression fracture after falling 1 week ago. She underwent vertebroplasty yesterday and was kept in the hospital overnight for observation after experiencing some postoperative hypotension. She has a 6-yr history of Addison's disease. She is planning to be discharged home today.
Priority and Delegation Decision: When you enter the room to assess B.V., you find him diaphoretic with a flushed face and pale extremities. His BP is 200/102 mm Hg. Which two initial actions would be most appropriate
A) Ask the UAP to obtain a stat bladder scan.
B) Have the LPN administer his oral antihypertensive meds stat.
C) Elevate the head of the bed while assessing for any noxious stimuli.
D) Ask the LPN to stay with B.V. while you call B.V.'s health care provider.
E) Insert rectal suppository after applying lidocaine to the area around the rectum.

Unlock Deck
Unlock for access to all 22 flashcards in this deck.
Unlock Deck
k this deck
11
The nurse should teach the patient with ankylosing spondylitis the importance of
A) regularly exercising and maintaining proper posture.
B) avoiding extremes in environmental temperatures.
C) maintaining usual physical activity during flare-ups.
D) applying hot and cool compresses for relief of local symptoms.
A) regularly exercising and maintaining proper posture.
B) avoiding extremes in environmental temperatures.
C) maintaining usual physical activity during flare-ups.
D) applying hot and cool compresses for relief of local symptoms.

Unlock Deck
Unlock for access to all 22 flashcards in this deck.
Unlock Deck
k this deck
12
Summarize the pathophysiology, clinical manifestations, collaborative care, and nursing management of ankylosing spondylitis, psoriatic arthritis, and reactive arthritis.

Unlock Deck
Unlock for access to all 22 flashcards in this deck.
Unlock Deck
k this deck
13
You are working on the medical-surgical unit and have been assigned to care for the following five patients. You have one LPN and one UAP on your team to help you.
Patients
A)J. is a 66-yr-old white woman who had an ischemic stroke 2 days ago. She has a history of migraines, hypertension, and atrial fibrillation. She is alert, oriented, and able to answer questions appropriately but has mild slowness in responding. She has left-sided arm weakness (3/5) and left leg weakness (4/5). Her vital signs are BP 160/84, HR 88, RR 20, T 37° C. She is receiving ASA 325 mg po daily, Lovenox 80 mg subcutaneously q12hr, lisinopril 10 mg po daily, Cardizem CD 180 mg po daily, and Coumadin 5 mg po daily. Her most recent INR was 1.7. She is scheduled to receive physical therapy today.
J)P. is a 24-yr-old woman who fell and hit her head after experiencing a tonic-clonic seizure. Her boyfriend found her lying semiconscious on the floor in her apartment. She had an emergency evacuation of a subdural hematoma and was initially admitted to the ICU. She was transferred to the medical-surgical unit yesterday and is scheduled for rehabilitation evaluation. She is oriented to person only and is somewhat restless. A safety sitter is with her at all times.
M)Y., an 80-yr-old Asian American man, had an ORIF 2 days ago for a fractured left hip. He has a 3-yr history of Alzheimer's disease and is confused to place and time. Although he has a history of agitation, he has been pleasant and cooperative. He has a personal alarm and bed alarm on for safety. His hip dressing is dry and intact and the drainage in the hemovac is minimal.
B)V., a 24-yr-old white man, was admitted to the ICU 3 weeks ago after suffering a C5-6 cervical spinal cord injury. B.V. dove into the shallow end of a neighbor's backyard pool and struck his head on the bottom. He was initially placed in cervical traction, intubated, and mechanically ventilated. He has since undergone surgical stabilization and the traction was removed. He was weaned from the ventilator 2 days ago. He was transferred to the medical-surgical unit yesterday. He is currently requesting medication for a "severe headache."
M)L. is a 58-yr-old white retired nurse who suffered an L4 compression fracture after falling 1 week ago. She underwent vertebroplasty yesterday and was kept in the hospital overnight for observation after experiencing some postoperative hypotension. She has a 6-yr history of Addison's disease. She is planning to be discharged home today.
B)V.'s bladder scan revealed 700 mL of urine. After you have the LPN catheterize him using a local anesthetic gel, his symptoms subside. You take this time to further teach B.V. about the clinical manifestations of autonomic dysreflexia and the need to report any symptom as soon as it appears. You also take the time to discuss bladder training strategies and how to avoid bladder distention in the future. B.V. is grateful for the information and your caring attitude. Just as you are finishing, the UAP informs you that M.Y. has pulled out his hemovac drain.
What should be your initial intervention for M.Y.
A) Reinsert the hemovac drain.
B) Assess the incision site for a hematoma.
C) Notify M.Y.'s surgeon that the drain was removed.
D) Apply pressure to the incisional site where the drain had been placed.
Patients
A)J. is a 66-yr-old white woman who had an ischemic stroke 2 days ago. She has a history of migraines, hypertension, and atrial fibrillation. She is alert, oriented, and able to answer questions appropriately but has mild slowness in responding. She has left-sided arm weakness (3/5) and left leg weakness (4/5). Her vital signs are BP 160/84, HR 88, RR 20, T 37° C. She is receiving ASA 325 mg po daily, Lovenox 80 mg subcutaneously q12hr, lisinopril 10 mg po daily, Cardizem CD 180 mg po daily, and Coumadin 5 mg po daily. Her most recent INR was 1.7. She is scheduled to receive physical therapy today.
J)P. is a 24-yr-old woman who fell and hit her head after experiencing a tonic-clonic seizure. Her boyfriend found her lying semiconscious on the floor in her apartment. She had an emergency evacuation of a subdural hematoma and was initially admitted to the ICU. She was transferred to the medical-surgical unit yesterday and is scheduled for rehabilitation evaluation. She is oriented to person only and is somewhat restless. A safety sitter is with her at all times.
M)Y., an 80-yr-old Asian American man, had an ORIF 2 days ago for a fractured left hip. He has a 3-yr history of Alzheimer's disease and is confused to place and time. Although he has a history of agitation, he has been pleasant and cooperative. He has a personal alarm and bed alarm on for safety. His hip dressing is dry and intact and the drainage in the hemovac is minimal.
B)V., a 24-yr-old white man, was admitted to the ICU 3 weeks ago after suffering a C5-6 cervical spinal cord injury. B.V. dove into the shallow end of a neighbor's backyard pool and struck his head on the bottom. He was initially placed in cervical traction, intubated, and mechanically ventilated. He has since undergone surgical stabilization and the traction was removed. He was weaned from the ventilator 2 days ago. He was transferred to the medical-surgical unit yesterday. He is currently requesting medication for a "severe headache."
M)L. is a 58-yr-old white retired nurse who suffered an L4 compression fracture after falling 1 week ago. She underwent vertebroplasty yesterday and was kept in the hospital overnight for observation after experiencing some postoperative hypotension. She has a 6-yr history of Addison's disease. She is planning to be discharged home today.
B)V.'s bladder scan revealed 700 mL of urine. After you have the LPN catheterize him using a local anesthetic gel, his symptoms subside. You take this time to further teach B.V. about the clinical manifestations of autonomic dysreflexia and the need to report any symptom as soon as it appears. You also take the time to discuss bladder training strategies and how to avoid bladder distention in the future. B.V. is grateful for the information and your caring attitude. Just as you are finishing, the UAP informs you that M.Y. has pulled out his hemovac drain.
What should be your initial intervention for M.Y.
A) Reinsert the hemovac drain.
B) Assess the incision site for a hematoma.
C) Notify M.Y.'s surgeon that the drain was removed.
D) Apply pressure to the incisional site where the drain had been placed.

Unlock Deck
Unlock for access to all 22 flashcards in this deck.
Unlock Deck
k this deck
14
In teaching a patient with SLE about the disorder, the nurse knows that the pathophysiology of SLE includes
A) circulating immune complexes formed from IgG autoantibodies reacting with IgG.
B) an autoimmune T-cell reaction that results in destruction of the deep dermal skin layer.
C) immunologic dysfunction leading to chronic inflammation in the cartilage and muscles.
D) the production of a variety of autoantibodies directed against components of the cell nucleus.
A) circulating immune complexes formed from IgG autoantibodies reacting with IgG.
B) an autoimmune T-cell reaction that results in destruction of the deep dermal skin layer.
C) immunologic dysfunction leading to chronic inflammation in the cartilage and muscles.
D) the production of a variety of autoantibodies directed against components of the cell nucleus.

Unlock Deck
Unlock for access to all 22 flashcards in this deck.
Unlock Deck
k this deck
15
Differentiate the pathophysiology, clinical manifestations, collaborative care, and nursing management of systemic lupus erythematosus, scleroderma, polymyositis, dermatomyositis, and Sjögren's syndrome.

Unlock Deck
Unlock for access to all 22 flashcards in this deck.
Unlock Deck
k this deck
16
You are working on the medical-surgical unit and have been assigned to care for the following five patients. You have one LPN and one UAP on your team to help you.
Patients
A)J. is a 66-yr-old white woman who had an ischemic stroke 2 days ago. She has a history of migraines, hypertension, and atrial fibrillation. She is alert, oriented, and able to answer questions appropriately but has mild slowness in responding. She has left-sided arm weakness (3/5) and left leg weakness (4/5). Her vital signs are BP 160/84, HR 88, RR 20, T 37° C. She is receiving ASA 325 mg po daily, Lovenox 80 mg subcutaneously q12hr, lisinopril 10 mg po daily, Cardizem CD 180 mg po daily, and Coumadin 5 mg po daily. Her most recent INR was 1.7. She is scheduled to receive physical therapy today.
J)P. is a 24-yr-old woman who fell and hit her head after experiencing a tonic-clonic seizure. Her boyfriend found her lying semiconscious on the floor in her apartment. She had an emergency evacuation of a subdural hematoma and was initially admitted to the ICU. She was transferred to the medical-surgical unit yesterday and is scheduled for rehabilitation evaluation. She is oriented to person only and is somewhat restless. A safety sitter is with her at all times.
M)Y., an 80-yr-old Asian American man, had an ORIF 2 days ago for a fractured left hip. He has a 3-yr history of Alzheimer's disease and is confused to place and time. Although he has a history of agitation, he has been pleasant and cooperative. He has a personal alarm and bed alarm on for safety. His hip dressing is dry and intact and the drainage in the hemovac is minimal.
B)V., a 24-yr-old white man, was admitted to the ICU 3 weeks ago after suffering a C5-6 cervical spinal cord injury. B.V. dove into the shallow end of a neighbor's backyard pool and struck his head on the bottom. He was initially placed in cervical traction, intubated, and mechanically ventilated. He has since undergone surgical stabilization and the traction was removed. He was weaned from the ventilator 2 days ago. He was transferred to the medical-surgical unit yesterday. He is currently requesting medication for a "severe headache."
M)L. is a 58-yr-old white retired nurse who suffered an L4 compression fracture after falling 1 week ago. She underwent vertebroplasty yesterday and was kept in the hospital overnight for observation after experiencing some postoperative hypotension. She has a 6-yr history of Addison's disease. She is planning to be discharged home today.
B)V.'s bladder scan revealed 700 mL of urine. After you have the LPN catheterize him using a local anesthetic gel, his symptoms subside. You take this time to further teach B.V. about the clinical manifestations of autonomic dysreflexia and the need to report any symptom as soon as it appears. You also take the time to discuss bladder training strategies and how to avoid bladder distention in the future. B.V. is grateful for the information and your caring attitude. Just as you are finishing, the UAP informs you that M.Y. has pulled out his hemovac drain.
Which intervention would be most appropriate in caring for A.J.
A) Place her left arm in a sling for support.
B) Arrange the food tray so that all foods are on the right side.
C) Call the health care provider to decrease her Coumadin dosage.
D) Position her left leg so that the ankle is lower than the knee to prevent contractures.
Patients
A)J. is a 66-yr-old white woman who had an ischemic stroke 2 days ago. She has a history of migraines, hypertension, and atrial fibrillation. She is alert, oriented, and able to answer questions appropriately but has mild slowness in responding. She has left-sided arm weakness (3/5) and left leg weakness (4/5). Her vital signs are BP 160/84, HR 88, RR 20, T 37° C. She is receiving ASA 325 mg po daily, Lovenox 80 mg subcutaneously q12hr, lisinopril 10 mg po daily, Cardizem CD 180 mg po daily, and Coumadin 5 mg po daily. Her most recent INR was 1.7. She is scheduled to receive physical therapy today.
J)P. is a 24-yr-old woman who fell and hit her head after experiencing a tonic-clonic seizure. Her boyfriend found her lying semiconscious on the floor in her apartment. She had an emergency evacuation of a subdural hematoma and was initially admitted to the ICU. She was transferred to the medical-surgical unit yesterday and is scheduled for rehabilitation evaluation. She is oriented to person only and is somewhat restless. A safety sitter is with her at all times.
M)Y., an 80-yr-old Asian American man, had an ORIF 2 days ago for a fractured left hip. He has a 3-yr history of Alzheimer's disease and is confused to place and time. Although he has a history of agitation, he has been pleasant and cooperative. He has a personal alarm and bed alarm on for safety. His hip dressing is dry and intact and the drainage in the hemovac is minimal.
B)V., a 24-yr-old white man, was admitted to the ICU 3 weeks ago after suffering a C5-6 cervical spinal cord injury. B.V. dove into the shallow end of a neighbor's backyard pool and struck his head on the bottom. He was initially placed in cervical traction, intubated, and mechanically ventilated. He has since undergone surgical stabilization and the traction was removed. He was weaned from the ventilator 2 days ago. He was transferred to the medical-surgical unit yesterday. He is currently requesting medication for a "severe headache."
M)L. is a 58-yr-old white retired nurse who suffered an L4 compression fracture after falling 1 week ago. She underwent vertebroplasty yesterday and was kept in the hospital overnight for observation after experiencing some postoperative hypotension. She has a 6-yr history of Addison's disease. She is planning to be discharged home today.
B)V.'s bladder scan revealed 700 mL of urine. After you have the LPN catheterize him using a local anesthetic gel, his symptoms subside. You take this time to further teach B.V. about the clinical manifestations of autonomic dysreflexia and the need to report any symptom as soon as it appears. You also take the time to discuss bladder training strategies and how to avoid bladder distention in the future. B.V. is grateful for the information and your caring attitude. Just as you are finishing, the UAP informs you that M.Y. has pulled out his hemovac drain.
Which intervention would be most appropriate in caring for A.J.
A) Place her left arm in a sling for support.
B) Arrange the food tray so that all foods are on the right side.
C) Call the health care provider to decrease her Coumadin dosage.
D) Position her left leg so that the ankle is lower than the knee to prevent contractures.

Unlock Deck
Unlock for access to all 22 flashcards in this deck.
Unlock Deck
k this deck
17
In teaching a patient with Sjögren's syndrome about drug therapy for this disorder, the nurse includes instruction on use of which drug
A) Pregabalin (Lyrica)
B) Etanercept (Enbrel)
C) Cyclosporine (Restasis)
D) Cyclobenzaprine (Flexeril)
A) Pregabalin (Lyrica)
B) Etanercept (Enbrel)
C) Cyclosporine (Restasis)
D) Cyclobenzaprine (Flexeril)

Unlock Deck
Unlock for access to all 22 flashcards in this deck.
Unlock Deck
k this deck
18
Explain the drug therapy and related nursing management associated with arthritis and connective tissue diseases.

Unlock Deck
Unlock for access to all 22 flashcards in this deck.
Unlock Deck
k this deck
19
You are working on the medical-surgical unit and have been assigned to care for the following five patients. You have one LPN and one UAP on your team to help you.
Patients
A)J. is a 66-yr-old white woman who had an ischemic stroke 2 days ago. She has a history of migraines, hypertension, and atrial fibrillation. She is alert, oriented, and able to answer questions appropriately but has mild slowness in responding. She has left-sided arm weakness (3/5) and left leg weakness (4/5). Her vital signs are BP 160/84, HR 88, RR 20, T 37° C. She is receiving ASA 325 mg po daily, Lovenox 80 mg subcutaneously q12hr, lisinopril 10 mg po daily, Cardizem CD 180 mg po daily, and Coumadin 5 mg po daily. Her most recent INR was 1.7. She is scheduled to receive physical therapy today.
J)P. is a 24-yr-old woman who fell and hit her head after experiencing a tonic-clonic seizure. Her boyfriend found her lying semiconscious on the floor in her apartment. She had an emergency evacuation of a subdural hematoma and was initially admitted to the ICU. She was transferred to the medical-surgical unit yesterday and is scheduled for rehabilitation evaluation. She is oriented to person only and is somewhat restless. A safety sitter is with her at all times.
M)Y., an 80-yr-old Asian American man, had an ORIF 2 days ago for a fractured left hip. He has a 3-yr history of Alzheimer's disease and is confused to place and time. Although he has a history of agitation, he has been pleasant and cooperative. He has a personal alarm and bed alarm on for safety. His hip dressing is dry and intact and the drainage in the hemovac is minimal.
B)V., a 24-yr-old white man, was admitted to the ICU 3 weeks ago after suffering a C5-6 cervical spinal cord injury. B.V. dove into the shallow end of a neighbor's backyard pool and struck his head on the bottom. He was initially placed in cervical traction, intubated, and mechanically ventilated. He has since undergone surgical stabilization and the traction was removed. He was weaned from the ventilator 2 days ago. He was transferred to the medical-surgical unit yesterday. He is currently requesting medication for a "severe headache."
M)L. is a 58-yr-old white retired nurse who suffered an L4 compression fracture after falling 1 week ago. She underwent vertebroplasty yesterday and was kept in the hospital overnight for observation after experiencing some postoperative hypotension. She has a 6-yr history of Addison's disease. She is planning to be discharged home today.
B)V.'s bladder scan revealed 700 mL of urine. After you have the LPN catheterize him using a local anesthetic gel, his symptoms subside. You take this time to further teach B.V. about the clinical manifestations of autonomic dysreflexia and the need to report any symptom as soon as it appears. You also take the time to discuss bladder training strategies and how to avoid bladder distention in the future. B.V. is grateful for the information and your caring attitude. Just as you are finishing, the UAP informs you that M.Y. has pulled out his hemovac drain.
When teaching J.P.'s boyfriend about what to expect during recovery from a head injury, which statement is most accurate
A) "You can tell by how great she looks physically that she will ultimately function well at the home."
B) "One good thing that will come out of this injury is that her seizures should occur less frequently."
C) "Most patients are usually transferred for acute rehabilitation management to prepare them for going home."
D) "She can expect a full recovery without any chronic problems, but it may take a few months to achieve that goal."
Patients
A)J. is a 66-yr-old white woman who had an ischemic stroke 2 days ago. She has a history of migraines, hypertension, and atrial fibrillation. She is alert, oriented, and able to answer questions appropriately but has mild slowness in responding. She has left-sided arm weakness (3/5) and left leg weakness (4/5). Her vital signs are BP 160/84, HR 88, RR 20, T 37° C. She is receiving ASA 325 mg po daily, Lovenox 80 mg subcutaneously q12hr, lisinopril 10 mg po daily, Cardizem CD 180 mg po daily, and Coumadin 5 mg po daily. Her most recent INR was 1.7. She is scheduled to receive physical therapy today.
J)P. is a 24-yr-old woman who fell and hit her head after experiencing a tonic-clonic seizure. Her boyfriend found her lying semiconscious on the floor in her apartment. She had an emergency evacuation of a subdural hematoma and was initially admitted to the ICU. She was transferred to the medical-surgical unit yesterday and is scheduled for rehabilitation evaluation. She is oriented to person only and is somewhat restless. A safety sitter is with her at all times.
M)Y., an 80-yr-old Asian American man, had an ORIF 2 days ago for a fractured left hip. He has a 3-yr history of Alzheimer's disease and is confused to place and time. Although he has a history of agitation, he has been pleasant and cooperative. He has a personal alarm and bed alarm on for safety. His hip dressing is dry and intact and the drainage in the hemovac is minimal.
B)V., a 24-yr-old white man, was admitted to the ICU 3 weeks ago after suffering a C5-6 cervical spinal cord injury. B.V. dove into the shallow end of a neighbor's backyard pool and struck his head on the bottom. He was initially placed in cervical traction, intubated, and mechanically ventilated. He has since undergone surgical stabilization and the traction was removed. He was weaned from the ventilator 2 days ago. He was transferred to the medical-surgical unit yesterday. He is currently requesting medication for a "severe headache."
M)L. is a 58-yr-old white retired nurse who suffered an L4 compression fracture after falling 1 week ago. She underwent vertebroplasty yesterday and was kept in the hospital overnight for observation after experiencing some postoperative hypotension. She has a 6-yr history of Addison's disease. She is planning to be discharged home today.
B)V.'s bladder scan revealed 700 mL of urine. After you have the LPN catheterize him using a local anesthetic gel, his symptoms subside. You take this time to further teach B.V. about the clinical manifestations of autonomic dysreflexia and the need to report any symptom as soon as it appears. You also take the time to discuss bladder training strategies and how to avoid bladder distention in the future. B.V. is grateful for the information and your caring attitude. Just as you are finishing, the UAP informs you that M.Y. has pulled out his hemovac drain.
When teaching J.P.'s boyfriend about what to expect during recovery from a head injury, which statement is most accurate
A) "You can tell by how great she looks physically that she will ultimately function well at the home."
B) "One good thing that will come out of this injury is that her seizures should occur less frequently."
C) "Most patients are usually transferred for acute rehabilitation management to prepare them for going home."
D) "She can expect a full recovery without any chronic problems, but it may take a few months to achieve that goal."

Unlock Deck
Unlock for access to all 22 flashcards in this deck.
Unlock Deck
k this deck
20
Teach the patient with fibromyalgia the importance of limiting intake of which foods (select all that apply)
A) Sugar
B) Alcohol
C) Caffeine
D) Red meat
E) Root vegetables
A) Sugar
B) Alcohol
C) Caffeine
D) Red meat
E) Root vegetables

Unlock Deck
Unlock for access to all 22 flashcards in this deck.
Unlock Deck
k this deck
21
Compare and contrast the possible etiologies, clinical manifestations, and collaborative and nursing management of fibromyalgia and chronic fatigue syndrome.

Unlock Deck
Unlock for access to all 22 flashcards in this deck.
Unlock Deck
k this deck
22
You are working on the medical-surgical unit and have been assigned to care for the following five patients. You have one LPN and one UAP on your team to help you.
Patients
A)J. is a 66-yr-old white woman who had an ischemic stroke 2 days ago. She has a history of migraines, hypertension, and atrial fibrillation. She is alert, oriented, and able to answer questions appropriately but has mild slowness in responding. She has left-sided arm weakness (3/5) and left leg weakness (4/5). Her vital signs are BP 160/84, HR 88, RR 20, T 37° C. She is receiving ASA 325 mg po daily, Lovenox 80 mg subcutaneously q12hr, lisinopril 10 mg po daily, Cardizem CD 180 mg po daily, and Coumadin 5 mg po daily. Her most recent INR was 1.7. She is scheduled to receive physical therapy today.
J)P. is a 24-yr-old woman who fell and hit her head after experiencing a tonic-clonic seizure. Her boyfriend found her lying semiconscious on the floor in her apartment. She had an emergency evacuation of a subdural hematoma and was initially admitted to the ICU. She was transferred to the medical-surgical unit yesterday and is scheduled for rehabilitation evaluation. She is oriented to person only and is somewhat restless. A safety sitter is with her at all times.
M)Y., an 80-yr-old Asian American man, had an ORIF 2 days ago for a fractured left hip. He has a 3-yr history of Alzheimer's disease and is confused to place and time. Although he has a history of agitation, he has been pleasant and cooperative. He has a personal alarm and bed alarm on for safety. His hip dressing is dry and intact and the drainage in the hemovac is minimal.
B)V., a 24-yr-old white man, was admitted to the ICU 3 weeks ago after suffering a C5-6 cervical spinal cord injury. B.V. dove into the shallow end of a neighbor's backyard pool and struck his head on the bottom. He was initially placed in cervical traction, intubated, and mechanically ventilated. He has since undergone surgical stabilization and the traction was removed. He was weaned from the ventilator 2 days ago. He was transferred to the medical-surgical unit yesterday. He is currently requesting medication for a "severe headache."
M)L. is a 58-yr-old white retired nurse who suffered an L4 compression fracture after falling 1 week ago. She underwent vertebroplasty yesterday and was kept in the hospital overnight for observation after experiencing some postoperative hypotension. She has a 6-yr history of Addison's disease. She is planning to be discharged home today.
B)V.'s bladder scan revealed 700 mL of urine. After you have the LPN catheterize him using a local anesthetic gel, his symptoms subside. You take this time to further teach B.V. about the clinical manifestations of autonomic dysreflexia and the need to report any symptom as soon as it appears. You also take the time to discuss bladder training strategies and how to avoid bladder distention in the future. B.V. is grateful for the information and your caring attitude. Just as you are finishing, the UAP informs you that M.Y. has pulled out his hemovac drain.
Priority and Management Decision: As you enter M.L.'s room to discuss her discharge plans, you find her all packed up and walking out the door. She tells you the UAP already told her what she needed to do. What is your best initial action
A) Ask M.L. if she has any further questions.
B) Call the UAP to M.L's room to find out what she told her.
C) Review discharge instructions with M.L. to ascertain correct understanding.
D) Give M.L. a telephone number to call in case she has any concerns when she gets home.
Patients
A)J. is a 66-yr-old white woman who had an ischemic stroke 2 days ago. She has a history of migraines, hypertension, and atrial fibrillation. She is alert, oriented, and able to answer questions appropriately but has mild slowness in responding. She has left-sided arm weakness (3/5) and left leg weakness (4/5). Her vital signs are BP 160/84, HR 88, RR 20, T 37° C. She is receiving ASA 325 mg po daily, Lovenox 80 mg subcutaneously q12hr, lisinopril 10 mg po daily, Cardizem CD 180 mg po daily, and Coumadin 5 mg po daily. Her most recent INR was 1.7. She is scheduled to receive physical therapy today.
J)P. is a 24-yr-old woman who fell and hit her head after experiencing a tonic-clonic seizure. Her boyfriend found her lying semiconscious on the floor in her apartment. She had an emergency evacuation of a subdural hematoma and was initially admitted to the ICU. She was transferred to the medical-surgical unit yesterday and is scheduled for rehabilitation evaluation. She is oriented to person only and is somewhat restless. A safety sitter is with her at all times.
M)Y., an 80-yr-old Asian American man, had an ORIF 2 days ago for a fractured left hip. He has a 3-yr history of Alzheimer's disease and is confused to place and time. Although he has a history of agitation, he has been pleasant and cooperative. He has a personal alarm and bed alarm on for safety. His hip dressing is dry and intact and the drainage in the hemovac is minimal.
B)V., a 24-yr-old white man, was admitted to the ICU 3 weeks ago after suffering a C5-6 cervical spinal cord injury. B.V. dove into the shallow end of a neighbor's backyard pool and struck his head on the bottom. He was initially placed in cervical traction, intubated, and mechanically ventilated. He has since undergone surgical stabilization and the traction was removed. He was weaned from the ventilator 2 days ago. He was transferred to the medical-surgical unit yesterday. He is currently requesting medication for a "severe headache."
M)L. is a 58-yr-old white retired nurse who suffered an L4 compression fracture after falling 1 week ago. She underwent vertebroplasty yesterday and was kept in the hospital overnight for observation after experiencing some postoperative hypotension. She has a 6-yr history of Addison's disease. She is planning to be discharged home today.
B)V.'s bladder scan revealed 700 mL of urine. After you have the LPN catheterize him using a local anesthetic gel, his symptoms subside. You take this time to further teach B.V. about the clinical manifestations of autonomic dysreflexia and the need to report any symptom as soon as it appears. You also take the time to discuss bladder training strategies and how to avoid bladder distention in the future. B.V. is grateful for the information and your caring attitude. Just as you are finishing, the UAP informs you that M.Y. has pulled out his hemovac drain.
Priority and Management Decision: As you enter M.L.'s room to discuss her discharge plans, you find her all packed up and walking out the door. She tells you the UAP already told her what she needed to do. What is your best initial action
A) Ask M.L. if she has any further questions.
B) Call the UAP to M.L's room to find out what she told her.
C) Review discharge instructions with M.L. to ascertain correct understanding.
D) Give M.L. a telephone number to call in case she has any concerns when she gets home.

Unlock Deck
Unlock for access to all 22 flashcards in this deck.
Unlock Deck
k this deck



