Deck 18: Diseases of the Renal System
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
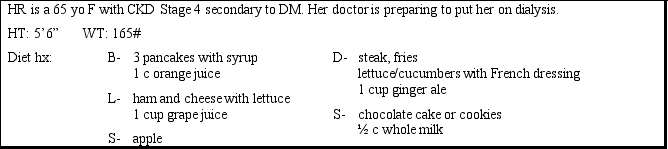
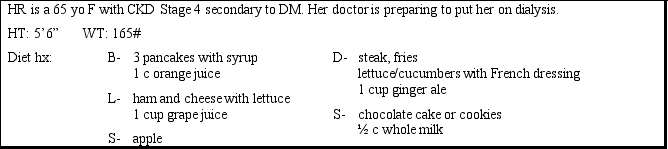
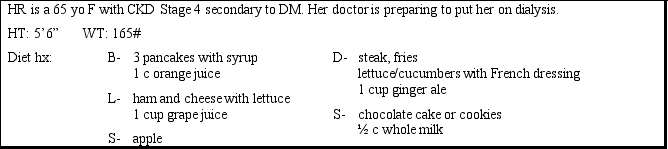
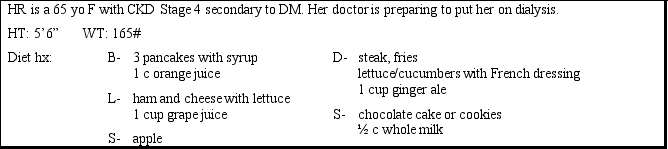
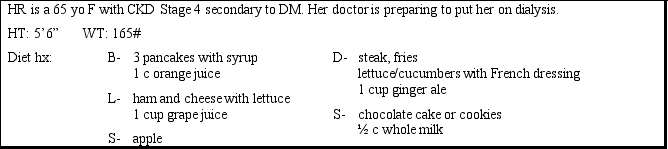
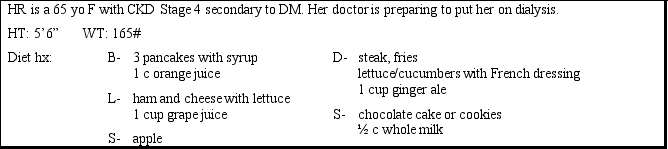
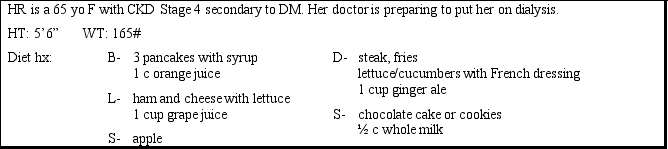
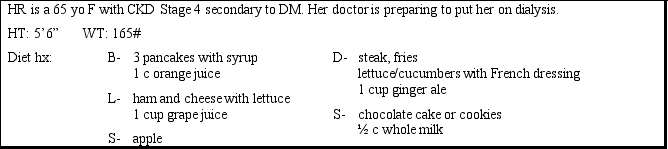
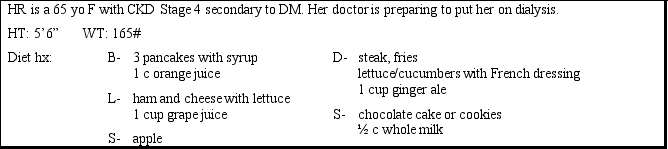
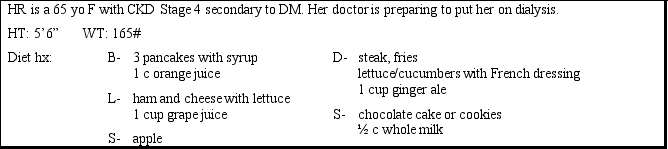
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Match between columns
Question
Match between columns

Unlock Deck
Sign up to unlock the cards in this deck!
Unlock Deck
Unlock Deck
1/46
Play
Full screen (f)
Deck 18: Diseases of the Renal System
1
The mechanism that best describes how diabetes leads to CKD is:
A)insulin has a negative effect on the nephrons.
B)albumin penetrates the walls of the collecting tubules.
C)hyperglycemia may cause the glomerulus to thicken and increase its permeability.
D)blood glucose levels remain elevated because of the impaired excretory function of the kidneys.
A)insulin has a negative effect on the nephrons.
B)albumin penetrates the walls of the collecting tubules.
C)hyperglycemia may cause the glomerulus to thicken and increase its permeability.
D)blood glucose levels remain elevated because of the impaired excretory function of the kidneys.
C
2
The basic principles of dialysis involve all of the following except:
A)diffusion of particles from areas of high concentration to low concentration.
B)osmosis of water moving to where solutes are more concentrated.
C)ultrafiltration, which utilizes the semipermeable membrane.
D)electrolyte movement from the ICF to the ECF.
A)diffusion of particles from areas of high concentration to low concentration.
B)osmosis of water moving to where solutes are more concentrated.
C)ultrafiltration, which utilizes the semipermeable membrane.
D)electrolyte movement from the ICF to the ECF.
D
3
Which of the following measures is used to best estimate kidney disease progression?
A)BUN
B)GFR
C)Cr
D)Cr clearance
A)BUN
B)GFR
C)Cr
D)Cr clearance
B
4
A GFR of 15 mL/min/173 m3 means:
A)a renal diet is warranted.
B)you are on renal replacement therapy.
C)your blood Cr level should be low.
D)the Cr clearance should be high.
A)a renal diet is warranted.
B)you are on renal replacement therapy.
C)your blood Cr level should be low.
D)the Cr clearance should be high.

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
5
As kidney function declines, serum creatinine will:
A)decrease.
B)increase.
C)stay the same.
A)decrease.
B)increase.
C)stay the same.

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
6
Your patient has been diagnosed with CKD He consumes very-high-fat foods and has elevated cholesterol The focus of your nutrition therapy should be:
A)heart-healthy eating.
B)supplementing with B vitamins.
C)decreasing protein intake.
D)monitoring P and K.
A)heart-healthy eating.
B)supplementing with B vitamins.
C)decreasing protein intake.
D)monitoring P and K.

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
7
Anemia is a common complication of CKD because of:
A)deficiency of B vitamins.
B)decreased EPO.
C)azotemia.
D)proteinuria.
A)deficiency of B vitamins.
B)decreased EPO.
C)azotemia.
D)proteinuria.

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
8
If a patient with renal disease shows depleted vitamin D levels, which function of the kidneys is affected?
A)excretory
B)production of hormones
C)pH homeostasis
D)filtering
A)excretory
B)production of hormones
C)pH homeostasis
D)filtering

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
9
The latest guidelines published about CKD are from which organization?
A)NKF K/DOQI
B)ADA
C)NIH
D)CDC
A)NKF K/DOQI
B)ADA
C)NIH
D)CDC

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
10
Which of the following persons is at highest risk for developing CKD?
A)a female with ARF
B)a male with high protein intake who has had ARF in the past
C)a male diabetic with diagnosed proteinuria
D)a female African American who has lupus
A)a female with ARF
B)a male with high protein intake who has had ARF in the past
C)a male diabetic with diagnosed proteinuria
D)a female African American who has lupus

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
11
If a patient with renal disease is diagnosed with an acid-base disorder, such metabolic acidosis, this would mean which function of the kidneys is affected?
A)excretory
B)production of hormones
C)pH homeostasis
D)filtering
A)excretory
B)production of hormones
C)pH homeostasis
D)filtering

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
12
In the regulation of blood pressure, the kidney is responsible for producing
A)erythropoietin.
B)renin.
C)angiotensin.
A)erythropoietin.
B)renin.
C)angiotensin.

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
13
When a person is unable to produce enough urine to excrete metabolic wastes, we say that the condition of _____ exists
A)oliguria
B)diuresis
C)homeostasis
A)oliguria
B)diuresis
C)homeostasis

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
14
The difference between azotemia and uremia is that in uremia there is/are:
A)accumulation of nitrogenous waste.
B)a rise in K.
C)a rise in BUN.
D)symptoms of weakness.
A)accumulation of nitrogenous waste.
B)a rise in K.
C)a rise in BUN.
D)symptoms of weakness.

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
15
Which of the following statements is not true about CKD?
A)It can progress to ESRD.
B)It is reversible if controlled properly.
C)There are 5 stages.
D)Metabolic abnormalities are common.
A)It can progress to ESRD.
B)It is reversible if controlled properly.
C)There are 5 stages.
D)Metabolic abnormalities are common.

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
16
The most important intervention in CKD is:
A)decreasing the dietary protein that the kidney has to metabolize.
B)maintaining normal electrolyte and organic solute balance.
C)preventing anemia.
D)slowing the progression of the disease.
A)decreasing the dietary protein that the kidney has to metabolize.
B)maintaining normal electrolyte and organic solute balance.
C)preventing anemia.
D)slowing the progression of the disease.

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
17
What is the normal serum creatinine value?
A)0.8-1.2 mg/dL for males, 0.6-1.0 mg/dL for females
B)0.6-1.0 mg/dL for males, 0.8-1.2 mg/dL for females
C)3.5-5.0 g/dL for males and females
D)9.0-10.5 mg/dL for males and females
A)0.8-1.2 mg/dL for males, 0.6-1.0 mg/dL for females
B)0.6-1.0 mg/dL for males, 0.8-1.2 mg/dL for females
C)3.5-5.0 g/dL for males and females
D)9.0-10.5 mg/dL for males and females

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
18
The minimum amount of urine that needs to be produced in order to rid the body of wastes is
A)1 liter.
B)500 mL.
C)1500 mL.
D)There is no minimum.
A)1 liter.
B)500 mL.
C)1500 mL.
D)There is no minimum.

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
19
Which of the following statements is not true of the physiology of the nephron?
A)The afferent arteriole carries blood to the glomerulus.
B)As the filtrate passes through the network of tubules, reabsorption of amino acids, glucose, selective minerals, and water occurs.
C)The cells of the loop of Henle perform active transport.
D)The blood is filtered via active transport and passive diffusion.
A)The afferent arteriole carries blood to the glomerulus.
B)As the filtrate passes through the network of tubules, reabsorption of amino acids, glucose, selective minerals, and water occurs.
C)The cells of the loop of Henle perform active transport.
D)The blood is filtered via active transport and passive diffusion.

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
20
In order to maintain the extracellular environment:
A)the nephron absorbs waste products of metabolism.
B)the nephron adjusts urinary excretion of water and electrolytes to maintain balance.
C)the distal tubule secretes Na and Ca.
D)glucose is absorbed in the collecting ducts.
A)the nephron absorbs waste products of metabolism.
B)the nephron adjusts urinary excretion of water and electrolytes to maintain balance.
C)the distal tubule secretes Na and Ca.
D)glucose is absorbed in the collecting ducts.

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
21
Case Study Multiple Choice
If her doctor starts her on PD, how much protein would she need each day?
A)0.60-0.75 g/kg
B)0.60-0.75 g/kg
C)1.2 g/kg
D)1.2-1.3 g/kg
If her doctor starts her on PD, how much protein would she need each day?
A)0.60-0.75 g/kg
B)0.60-0.75 g/kg
C)1.2 g/kg
D)1.2-1.3 g/kg

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
22
The main difference in medical nutrition therapy between Stage 3 CKD and Stage 5 CKD is:
A)the amount of sodium allowed.
B)the amount of protein.
C)the servings of CHO.
D)Ca recommendations.
A)the amount of sodium allowed.
B)the amount of protein.
C)the servings of CHO.
D)Ca recommendations.

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
23
Which of the following foods is not a high-P food?
A)broth
B)cocoa
C)cheese
D)liver
A)broth
B)cocoa
C)cheese
D)liver

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
24
Case Study Multiple Choice
If her doctor starts her on HD, how much protein would she need each day?
A)0.60-0.75 g/kg
B)0.60-0.75 g/kg
C)1.2 g/kg
D)1.2-1.3 g/kg
If her doctor starts her on HD, how much protein would she need each day?
A)0.60-0.75 g/kg
B)0.60-0.75 g/kg
C)1.2 g/kg
D)1.2-1.3 g/kg

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
25
When someone has acute renal failure that we determine is a result of exposure to contrast dye, which of the following is a likely cause?
A)nephrotoxicity
B)acute tubular necrosis
C)severe dehydration
D)ureter blockage
A)nephrotoxicity
B)acute tubular necrosis
C)severe dehydration
D)ureter blockage

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
26
Patients on PD (peritoneal dialysis) require
A)low-protein diets.
B)K restrictions.
C)high-kcalorie diets.
D)phosphate binders.
A)low-protein diets.
B)K restrictions.
C)high-kcalorie diets.
D)phosphate binders.

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
27
The primary nutrition intervention in ARF is:
A)monitoring serum albumin.
B)delivering adequate calories and protein.
C)high protein intake.
D)calcium supplementation.
A)monitoring serum albumin.
B)delivering adequate calories and protein.
C)high protein intake.
D)calcium supplementation.

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
28
Of the following foods, which is the lowest in potassium?
A)bananas
B)tomatoes
C)prunes
D)grapes
A)bananas
B)tomatoes
C)prunes
D)grapes

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
29
When someone has acute renal failure that we determine is a result of inadequate perfusion, which of the following is a likely cause?
A)nephrotoxicity
B)glomerulonephritis
C)severe dehydration
D)ureter blockage
A)nephrotoxicity
B)glomerulonephritis
C)severe dehydration
D)ureter blockage

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
30
Case Study Multiple Choice
Which of the above foods is contributing the most potassium?
A)orange juice
B)pancakes
C)steak
D)milk
Which of the above foods is contributing the most potassium?
A)orange juice
B)pancakes
C)steak
D)milk

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
31
When educating your patients on the amount of Ca to include in their renal diet, it is important to also include:
A)bioavailable dairy.
B)the inverse relationship with P.
C)phosphate binders.
D)oxalates.
A)bioavailable dairy.
B)the inverse relationship with P.
C)phosphate binders.
D)oxalates.

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
32
If intradialytic weight gain exceeds 5%, one can assume:
A)the patient needs more fluid restriction.
B)the patient is experiencing hypertension.
C)the patient is following a strict 2-gram sodium diet.
D)the patient consumed too much food.
A)the patient needs more fluid restriction.
B)the patient is experiencing hypertension.
C)the patient is following a strict 2-gram sodium diet.
D)the patient consumed too much food.

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
33
Case Study Multiple Choice
Which of the above foods is contributing the most phosphorus?
A)orange juice
B)pancakes
C)steak
D)milk
Which of the above foods is contributing the most phosphorus?
A)orange juice
B)pancakes
C)steak
D)milk

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
34
Secondary hyperparathyroidism can lead to:
A)azotemia.
B)increased serum Ca.
C)osteitis fibrosa cystica.
D)decreased inactive vitamin D.
A)azotemia.
B)increased serum Ca.
C)osteitis fibrosa cystica.
D)decreased inactive vitamin D.

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
35
In nephrotic syndrome:
A)protein spills into urine.
B)serum glucose becomes elevated.
C)urine output decreases.
D)ALB remains normal.
A)protein spills into urine.
B)serum glucose becomes elevated.
C)urine output decreases.
D)ALB remains normal.

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
36
We often use a form of dialysis to assist in the treatment of acute renal failure This mode of dialysis is called:
A)CCPD
B)CRRT
C)hemodialysis
D)CAPD
A)CCPD
B)CRRT
C)hemodialysis
D)CAPD

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
37
KL is a 45 yo M admitted to the hospital with an infection.He is on PD secondary to congenital disease of the kidney.
HT: 6' WT: 170#
How many grams of protein does KL require?
A)87 g
B)93 g
C)46 g
D)62 g
HT: 6' WT: 170#
How many grams of protein does KL require?
A)87 g
B)93 g
C)46 g
D)62 g

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
38
Proteinuria is caused by:
A)exogenous dietary protein beyond that required.
B)permeability of the glomerular membrane.
C)excess secretion by the loop of Henle.
D)PEM.
A)exogenous dietary protein beyond that required.
B)permeability of the glomerular membrane.
C)excess secretion by the loop of Henle.
D)PEM.

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
39
Case Study Multiple Choice
Based on the National Kidney Foundation guidelines, how would you estimate HR's calorie needs?
A)20-25 kcal/kg
B)25-30 kcal/kg
C)30-35 kcal/kg
D)15-20 kcal/kg
Based on the National Kidney Foundation guidelines, how would you estimate HR's calorie needs?
A)20-25 kcal/kg
B)25-30 kcal/kg
C)30-35 kcal/kg
D)15-20 kcal/kg

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
40
Which condition is a result of the loss of the glomerular barrier to protein and results in large protein losses in the urine?
A)end-stage renal disease
B)kidney stones
C)nephrotic syndrome
D)acute renal failure
A)end-stage renal disease
B)kidney stones
C)nephrotic syndrome
D)acute renal failure

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
41
KL is a 45 yo M admitted to the hospital with an infection.He is on PD secondary to congenital disease of the kidney.
HT: 6' WT: 170#
How many kcalories does KL require?
A)2700 kcal
B)1931kcal
C)2160 kcal
D)1800 kcal
HT: 6' WT: 170#
How many kcalories does KL require?
A)2700 kcal
B)1931kcal
C)2160 kcal
D)1800 kcal

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
42
KL is a 45 yo M admitted to the hospital with an infection.He is on PD secondary to congenital disease of the kidney.
HT: 6' WT: 170#
Which of the following true about KL?
A)he goes to a dialysis center three times per week
B)his caloric intake will have to be adjusted to account for calories in dialysate
C)he will have to wait 6 weeks for the fistula to mature
D)he is not a candidate for a kidney transplant
HT: 6' WT: 170#
Which of the following true about KL?
A)he goes to a dialysis center three times per week
B)his caloric intake will have to be adjusted to account for calories in dialysate
C)he will have to wait 6 weeks for the fistula to mature
D)he is not a candidate for a kidney transplant

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
43
KL is a 45 yo M admitted to the hospital with an infection.He is on PD secondary to congenital disease of the kidney.
HT: 6' WT: 170#
KL has visited the dietitian Which of the following is true about his diet?
A)he has less of a potassium restriction than he would on HD
B)his phosphorus is unrestricted
C)his fluid intake must be output + 1000 cc
D)he needs to limit protein of high biological value
HT: 6' WT: 170#
KL has visited the dietitian Which of the following is true about his diet?
A)he has less of a potassium restriction than he would on HD
B)his phosphorus is unrestricted
C)his fluid intake must be output + 1000 cc
D)he needs to limit protein of high biological value

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
44
KL is a 45 yo M admitted to the hospital with an infection.He is on PD secondary to congenital disease of the kidney.
HT: 6' WT: 170#
What is likely the source of his infection?
A)fistula
B)AV graft
C)catheter
D)UTI
HT: 6' WT: 170#
What is likely the source of his infection?
A)fistula
B)AV graft
C)catheter
D)UTI

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
45
Match between columns

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck
46
Match between columns

Unlock Deck
Unlock for access to all 46 flashcards in this deck.
Unlock Deck
k this deck



