Deck 15: Diseases of the Lower Gastrointestinal Tract
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question

Unlock Deck
Sign up to unlock the cards in this deck!
Unlock Deck
Unlock Deck
1/80
Play
Full screen (f)
Deck 15: Diseases of the Lower Gastrointestinal Tract
1
How much fiber is recommended for adults daily?
A) 10-15 g
B) 20-25 g
C) 25-38 g
D) 40-50 g
E) 50-60 g
A) 10-15 g
B) 20-25 g
C) 25-38 g
D) 40-50 g
E) 50-60 g
C
2
The standard first step in reducing symptoms of fat malabsorption would be to:
A) increase intake of fat-soluble vitamins
B) restrict carbohydrate intake
C) limit fluids
D) restrict fat intake to 25-30 g/day
E) decrease protein intake
A) increase intake of fat-soluble vitamins
B) restrict carbohydrate intake
C) limit fluids
D) restrict fat intake to 25-30 g/day
E) decrease protein intake
D
3
Which of the following substances aid in electrolyte and fluid absorption in the large intestine?
A) bile salts and pancreatic lipase
B) triglycerides and chylomicrons
C) potassium and bicarbonate
D) hydrogen and sodium
E) aminopeptidases and chloride
A) bile salts and pancreatic lipase
B) triglycerides and chylomicrons
C) potassium and bicarbonate
D) hydrogen and sodium
E) aminopeptidases and chloride
C
4
Which of the following is an anticholinergic, antidiarrheal medication?
A) hyoscyamine
B) pectin
C) kaolin
D) metronidazole
E) olsazine
A) hyoscyamine
B) pectin
C) kaolin
D) metronidazole
E) olsazine

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
5
Which symptom is included as part of the Rome IV Criteria for diagnosing constipation?
A) blood in the stools
B) abdominal pain
C) sensation of incomplete evacuation
D) fewer than six defecations per week
E) flatulence
A) blood in the stools
B) abdominal pain
C) sensation of incomplete evacuation
D) fewer than six defecations per week
E) flatulence

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
6
Which statement best describes the action of the opiate antidiarrheal medications?
A) They enter bacteria and destroy their DNA.
B) They decrease fluid secretions and reduce stool output.
C) They decrease intestinal muscle tone and peristalsis of the GI tract.
D) They inhibit acetylcholine and decrease peristalsis.
E) They work as anti-inflammatory agents and immune suppressants in the colon.
A) They enter bacteria and destroy their DNA.
B) They decrease fluid secretions and reduce stool output.
C) They decrease intestinal muscle tone and peristalsis of the GI tract.
D) They inhibit acetylcholine and decrease peristalsis.
E) They work as anti-inflammatory agents and immune suppressants in the colon.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
7
The primary enzyme involved in starch digestion is:
A) motilin
B) pancreatic amylase
C) vasoactive intestinal polypeptide
D) substance P
E) cholecystokinin
A) motilin
B) pancreatic amylase
C) vasoactive intestinal polypeptide
D) substance P
E) cholecystokinin

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
8
Identify the mechanism of diarrhea that is caused by the excessive consumption of erythromycin.
A) collagenous colitis
B) secretory diarrhea
C) motility diarrhea
D) exudative diarrhea
E) pseudomembranous colitis
A) collagenous colitis
B) secretory diarrhea
C) motility diarrhea
D) exudative diarrhea
E) pseudomembranous colitis

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
9
Which of the following is a component of the WHO's standard recipe for an ORS?
A) four tablespoons of table salt
B) half a tablespoon of potassium bicarbonate
C) half a tablespoon of sodium bicarbonate
D) a quarter tablespoon potassium sulphate
E) ten tablespoons of sugar
A) four tablespoons of table salt
B) half a tablespoon of potassium bicarbonate
C) half a tablespoon of sodium bicarbonate
D) a quarter tablespoon potassium sulphate
E) ten tablespoons of sugar

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
10
Which sphincter or valve protects the small intestine from the harmful bacteria that are present in the large intestine?
A) pyloric sphincter
B) ileocecal valve
C) sphincter of Oddi
D) lower esophageal sphincter
E) internal anal sphincter
A) pyloric sphincter
B) ileocecal valve
C) sphincter of Oddi
D) lower esophageal sphincter
E) internal anal sphincter

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
11
Which of the following is a true statement regarding osmotic diarrhea?
A) It is typically caused by a lack of fiber in the diet.
B) It is caused by endotoxins that are released by bacteria.
C) It is associated with those who travel to other countries.
D) It develops from an underlying disease.
E) It stops when the causative agent is removed.
A) It is typically caused by a lack of fiber in the diet.
B) It is caused by endotoxins that are released by bacteria.
C) It is associated with those who travel to other countries.
D) It develops from an underlying disease.
E) It stops when the causative agent is removed.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
12
A dietitian is working with a client to help her improve her fiber intake. What would the dietitian most likely recommend?
A) Use white flour for baking and cooking.
B) Increase fiber intake by 20 g per day until tolerated.
C) Avoid dried beans and peas.
D) Choose fruit and vegetable juices over fresh produce.
E) Consume brown or wild rice instead of white rice or potatoes.
A) Use white flour for baking and cooking.
B) Increase fiber intake by 20 g per day until tolerated.
C) Avoid dried beans and peas.
D) Choose fruit and vegetable juices over fresh produce.
E) Consume brown or wild rice instead of white rice or potatoes.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
13
Which of the following is a brush border enzyme?
A) trypsinogen
B) chymotrypsinogen
C) elastase
D) procarboxypeptidase
E) alpha-dextrinase
A) trypsinogen
B) chymotrypsinogen
C) elastase
D) procarboxypeptidase
E) alpha-dextrinase

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
14
The primary function of the large intestine is to:
A) inhibit gastric emptying and postprandial glucagon release
B) provide a site for reabsorption of water, electrolytes, and some vitamins
C) stimulate acid secretion and pancreatic HCO3secretion
D) provide enzymatic digestion before defecation
E) provide sodium, iron, and water for chyme production
A) inhibit gastric emptying and postprandial glucagon release
B) provide a site for reabsorption of water, electrolytes, and some vitamins
C) stimulate acid secretion and pancreatic HCO3secretion
D) provide enzymatic digestion before defecation
E) provide sodium, iron, and water for chyme production

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
15
Where are stem cells and enterocytes of the small intestine found?
A) within the folds of Kerckring
B) on the outside of the villi
C) on the surface of the brush border
D) in the crypts between the villi
E) within the cells of the microvilli
A) within the folds of Kerckring
B) on the outside of the villi
C) on the surface of the brush border
D) in the crypts between the villi
E) within the cells of the microvilli

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
16
Recommendations for the prevention of diarrhea worldwide include strategies such as:
A) washing hands with soap after touching food
B) promoting hygiene education
C) exclusive formula feeding for infants
D) preventing weaning practices
E) immunizing all adults
A) washing hands with soap after touching food
B) promoting hygiene education
C) exclusive formula feeding for infants
D) preventing weaning practices
E) immunizing all adults

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
17
The most likely cause of steatorrhea is:
A) increased secretion of pancreatic lipase
B) the improper absorption of vitamin B12in the ileum
C) the excretion of bile acids
D) the excessive breakdown of low-density lipoproteins
E) the improper digestion or absorption of lipids
A) increased secretion of pancreatic lipase
B) the improper absorption of vitamin B12in the ileum
C) the excretion of bile acids
D) the excessive breakdown of low-density lipoproteins
E) the improper digestion or absorption of lipids

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
18
Which condition would most likely be a possible cause of malabsorption?
A) glomerulosclerosis
B) amyloidosis
C) appendicitis
D) albuminuria
E) colon polyps
A) glomerulosclerosis
B) amyloidosis
C) appendicitis
D) albuminuria
E) colon polyps

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
19
Current practice of nutrition therapy for diarrhea involves:
A) making the patient NPO
B) feeding clear liquids
C) enteral nutrition for three days
D) parenteral nutrition until diarrhea resolves
E) stimulating the GI tract by feeding the patient
A) making the patient NPO
B) feeding clear liquids
C) enteral nutrition for three days
D) parenteral nutrition until diarrhea resolves
E) stimulating the GI tract by feeding the patient

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
20
Which of the following best describes the migrating motility complex (MMC)?
A) weak contractions that rid the small intestine of leftover bacteria or waste
B) segmentation motility that mixes chyme with digestive secretions
C) a hormone called gastrin that stimulates the onset of segmental contractions
D) a muscular valve that controls the rate of movement of food from the ileum
E) a substance that neutralizes the very acidic chyme as it enters from the stomach
A) weak contractions that rid the small intestine of leftover bacteria or waste
B) segmentation motility that mixes chyme with digestive secretions
C) a hormone called gastrin that stimulates the onset of segmental contractions
D) a muscular valve that controls the rate of movement of food from the ileum
E) a substance that neutralizes the very acidic chyme as it enters from the stomach

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
21
What recommendations should the dietitian make for a client with a newly placed ostomy?
A) Eat the largest meal of the day in the evening to reduce output overnight.
B) Limit dairy products to reduce odor in output.
C) Drink at least 4-5 cups of fluid every day.
D) Choose foods that can thicken stools, such as peanut butter, margarine, and yogurt.
E) Avoid spicy or fried foods, which can cause diarrhea.
A) Eat the largest meal of the day in the evening to reduce output overnight.
B) Limit dairy products to reduce odor in output.
C) Drink at least 4-5 cups of fluid every day.
D) Choose foods that can thicken stools, such as peanut butter, margarine, and yogurt.
E) Avoid spicy or fried foods, which can cause diarrhea.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
22
Which is a true statement regarding diverticulosis?
A) Diverticulosis is most commonly found in infants.
B) Diverticulosis is asymptomatic in most people.
C) Factors associated with diverticulosis include lactose and gluten intolerance.
D) Diverticulosis develops because of low fiber intake.
E) People with a history of constipation are more likely to develop diverticulosis.
A) Diverticulosis is most commonly found in infants.
B) Diverticulosis is asymptomatic in most people.
C) Factors associated with diverticulosis include lactose and gluten intolerance.
D) Diverticulosis develops because of low fiber intake.
E) People with a history of constipation are more likely to develop diverticulosis.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
23
Which condition is associated with irritable bowel syndrome?
A) pernicious anemia
B) Graves' disease
C) systemic lupus erythematosus
D) type 1 diabetes
E) temporomandibular joint (TMJ) syndrome
A) pernicious anemia
B) Graves' disease
C) systemic lupus erythematosus
D) type 1 diabetes
E) temporomandibular joint (TMJ) syndrome

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
24
Damage to the intestinal mucosa observed in celiac disease occurs when the small intestine is exposed to:
A) α- gliadin
B) lactate dehydrogenase
C) glycophorin
D) fibronectin
E) selectin
A) α- gliadin
B) lactate dehydrogenase
C) glycophorin
D) fibronectin
E) selectin

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
25
Which condition is most likely a cause of short bowel syndrome among children?
A) obesity treatment
B) necrotizing enterocolitis
C) mesenteric ischemia
D) strangulated hernia
E) surgical bypass
A) obesity treatment
B) necrotizing enterocolitis
C) mesenteric ischemia
D) strangulated hernia
E) surgical bypass

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
26
Which symptoms are the indicators of ulcerative colitis?
A) nausea and vomiting, and headache
B) epigastric pain and abdominal fullness
C) nausea, bloating, and steatorrhea
D) abdominal pain, bloody diarrhea, and tenesmus
E) nausea, constipation, and flatulence
A) nausea and vomiting, and headache
B) epigastric pain and abdominal fullness
C) nausea, bloating, and steatorrhea
D) abdominal pain, bloody diarrhea, and tenesmus
E) nausea, constipation, and flatulence

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
27
A patient has just undergone a surgery to remove the colon and the rectum. This would most likely be a result of:
A) gastrostomy
B) jejunostomy
C) colostomy
D) urostomy
E) ileostomy
A) gastrostomy
B) jejunostomy
C) colostomy
D) urostomy
E) ileostomy

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
28
A patient with Crohn's disease is undergoing a sigmoidoscopy. What is the function of this procedure?
A) imaging of the stomach, liver, and pancreas
B) evaluation of the colon and distal ileum
C) assessment of the small intestine
D) evaluation of the colon up to the splenic flexure
E) evaluation of the esophagus, stomach, and duodenum
A) imaging of the stomach, liver, and pancreas
B) evaluation of the colon and distal ileum
C) assessment of the small intestine
D) evaluation of the colon up to the splenic flexure
E) evaluation of the esophagus, stomach, and duodenum

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
29
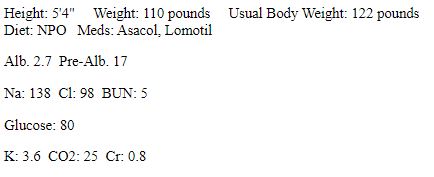
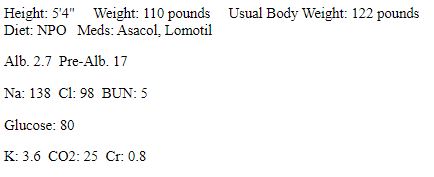
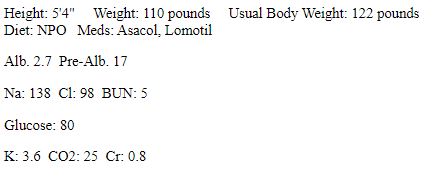
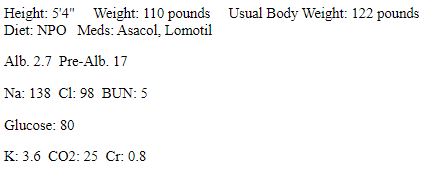
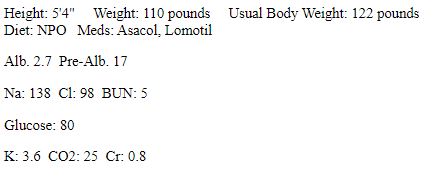
RD is a 29-year-old female who is admitted to a hospital. She has intractable diarrhea and abdominal pain. She has a past medical history of Crohn's disease and has had two resections of the small intestine. She frequently experiences pain in the right lower quadrant of the abdomen after eating. She claims the pain often gets so bad that she is afraid to eat and has been progressively consuming less than her caloric needs. She takes Asacol and Lomotil to manage the symptoms of Crohn's disease. During a colonoscopy, an obstruction resulting from stricture in the terminal ileum was discovered. A surgery was performed to remove the obstruction and a resection was done with the remaining intestine. RD's gastroenterologist recommends bowel rest and expects her to have a full recovery. 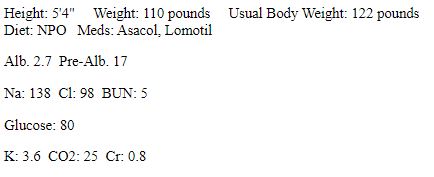 What type of medication would most likely be prescribed for RD during the acute phase of Crohn's disease?
What type of medication would most likely be prescribed for RD during the acute phase of Crohn's disease?
A) proton pump inhibitors
B) biologic therapies
C) corticosteroids
D) purine antagonists
E) H2receptor agonists
 What type of medication would most likely be prescribed for RD during the acute phase of Crohn's disease?
What type of medication would most likely be prescribed for RD during the acute phase of Crohn's disease?A) proton pump inhibitors
B) biologic therapies
C) corticosteroids
D) purine antagonists
E) H2receptor agonists

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
30
What should be offered to a patient to eat or drink after a surgery that results in short bowel syndrome?
A) low-residue hypertonic liquids
B) hypotonic clear liquids
C) lactose-free milk or dairy
D) low-sugar, isotonic liquids
E) yogurt with probiotics
A) low-residue hypertonic liquids
B) hypotonic clear liquids
C) lactose-free milk or dairy
D) low-sugar, isotonic liquids
E) yogurt with probiotics

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
31
RD is a 29-year-old female who is admitted to a hospital. She has intractable diarrhea and abdominal pain. She has a past medical history of Crohn's disease and has had two resections of the small intestine. She frequently experiences pain in the right lower quadrant of the abdomen after eating. She claims the pain often gets so bad that she is afraid to eat and has been progressively consuming less than her caloric needs. She takes Asacol and Lomotil to manage the symptoms of Crohn's disease. During a colonoscopy, an obstruction resulting from stricture in the terminal ileum was discovered. A surgery was performed to remove the obstruction and a resection was done with the remaining intestine. RD's gastroenterologist recommends bowel rest and expects her to have a full recovery. 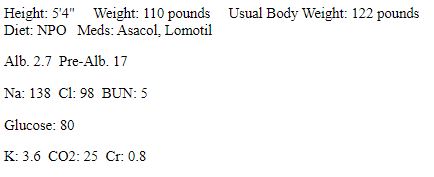
What type of foods would a nutritionist recommend for RD for rehabilitation during a period of remission?
A) foods high in oxalate
B) low-residue foods
C) foods that contain probiotics
D) lactose-free foods
E) foods without glutamine
What type of foods would a nutritionist recommend for RD for rehabilitation during a period of remission?
A) foods high in oxalate
B) low-residue foods
C) foods that contain probiotics
D) lactose-free foods
E) foods without glutamine

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
32
Which of the following foods may increase the risk of urolithiasis or kidney stones?
A) beets
B) corn
C) mushrooms
D) okra
E) green peas
A) beets
B) corn
C) mushrooms
D) okra
E) green peas

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
33
RD is a 29-year-old female who is admitted to a hospital. She has intractable diarrhea and abdominal pain. She has a past medical history of Crohn's disease and has had two resections of the small intestine. She frequently experiences pain in the right lower quadrant of the abdomen after eating. She claims the pain often gets so bad that she is afraid to eat and has been progressively consuming less than her caloric needs. She takes Asacol and Lomotil to manage the symptoms of Crohn's disease. During a colonoscopy, an obstruction resulting from stricture in the terminal ileum was discovered. A surgery was performed to remove the obstruction and a resection was done with the remaining intestine. RD's gastroenterologist recommends bowel rest and expects her to have a full recovery. 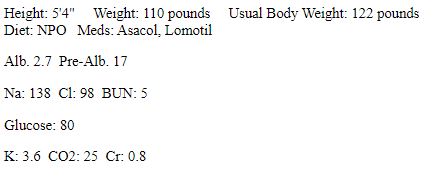
Which condition would most likely place RD at a risk of folate deficiency?
A) anorexia
B) healing after surgery
C) medication use
D) high-volume diarrhea
E) blood loss
Which condition would most likely place RD at a risk of folate deficiency?
A) anorexia
B) healing after surgery
C) medication use
D) high-volume diarrhea
E) blood loss

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
34
Which statement is true of small intestinal bacterial overgrowth?
A) The patient is exposed to the contaminated instruments during surgery.
B) Cross-contamination of bacteria occurs from the colon to the small intestine.
C) The colon is perforated, and bacteria enter the peritoneum.
D) The surgical incision becomes infected because of bacterial overgrowth.
E) The patient passes excess bacteria from the stomach to the small intestine.
A) The patient is exposed to the contaminated instruments during surgery.
B) Cross-contamination of bacteria occurs from the colon to the small intestine.
C) The colon is perforated, and bacteria enter the peritoneum.
D) The surgical incision becomes infected because of bacterial overgrowth.
E) The patient passes excess bacteria from the stomach to the small intestine.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
35
Which of the following sequences of amino acids found in gluten is present in rye?
A) gastrin
B) gliadin
C) secalin
D) hordein
E) motilin
A) gastrin
B) gliadin
C) secalin
D) hordein
E) motilin

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
36
What is the most appropriate treatment for celiac disease?
A) symptomatic management with antidiarrheal medications
B) supplementation with probiotics
C) adherence to a gluten-free diet
D) antibiotics and immunomodulator medications
E) total colectomy
A) symptomatic management with antidiarrheal medications
B) supplementation with probiotics
C) adherence to a gluten-free diet
D) antibiotics and immunomodulator medications
E) total colectomy

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
37
RD is a 29-year-old female who is admitted to a hospital. She has intractable diarrhea and abdominal pain. She has a past medical history of Crohn's disease and has had two resections of the small intestine. She frequently experiences pain in the right lower quadrant of the abdomen after eating. She claims the pain often gets so bad that she is afraid to eat and has been progressively consuming less than her caloric needs. She takes Asacol and Lomotil to manage the symptoms of Crohn's disease. During a colonoscopy, an obstruction resulting from stricture in the terminal ileum was discovered. A surgery was performed to remove the obstruction and a resection was done with the remaining intestine. RD's gastroenterologist recommends bowel rest and expects her to have a full recovery. 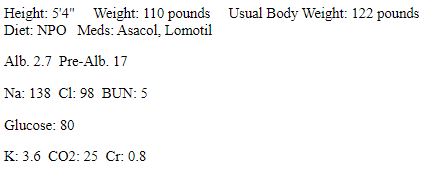
RD's frequent diarrhea most likely puts her at risk of which nutrient deficiency?
A) calcium
B) iron
C) vitamin D
D) vitamin B12
E) magnesium
RD's frequent diarrhea most likely puts her at risk of which nutrient deficiency?
A) calcium
B) iron
C) vitamin D
D) vitamin B12
E) magnesium

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
38
What of the following foods is recommended under a low-FODMAP diet?
A) apples
B) ice cream
C) sweet potatoes
D) rum
E) baked beans
A) apples
B) ice cream
C) sweet potatoes
D) rum
E) baked beans

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
39
RD is a 29-year-old female who is admitted to a hospital. She has intractable diarrhea and abdominal pain. She has a past medical history of Crohn's disease and has had two resections of the small intestine. She frequently experiences pain in the right lower quadrant of the abdomen after eating. She claims the pain often gets so bad that she is afraid to eat and has been progressively consuming less than her caloric needs. She takes Asacol and Lomotil to manage the symptoms of Crohn's disease. During a colonoscopy, an obstruction resulting from stricture in the terminal ileum was discovered. A surgery was performed to remove the obstruction and a resection was done with the remaining intestine. RD's gastroenterologist recommends bowel rest and expects her to have a full recovery. 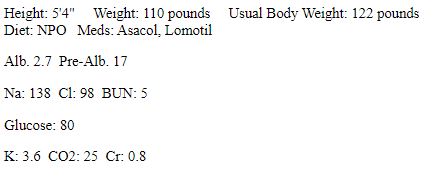
What is a common complication of Crohn's disease that may require surgery?
A) weight loss
B) diarrhea
C) intestinal perforation
D) tenesmus
E) muscle wasting
What is a common complication of Crohn's disease that may require surgery?
A) weight loss
B) diarrhea
C) intestinal perforation
D) tenesmus
E) muscle wasting

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
40
A patient with inflammatory bowel disease is taking medication to manage his acute symptoms. What must a dietitian consider when planning the nutrition interventions for this patient?
A) The patient may have increased nutrient requirements.
B) The patient should remain NPO during periods of exacerbation of symptoms.
C) The patient will need parenteral nutrition in addition to medication.
D) The patient will have decreased fluid requirements.
E) The patient will experience nausea, which will impact food intake.
A) The patient may have increased nutrient requirements.
B) The patient should remain NPO during periods of exacerbation of symptoms.
C) The patient will need parenteral nutrition in addition to medication.
D) The patient will have decreased fluid requirements.
E) The patient will experience nausea, which will impact food intake.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
41
Haustration in the large intestine is accomplished by alternating waves of relaxation and contraction of circular muscle.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
42
As chyme enters the duodenum from the stomach, gastrin stimulates the segmental contractions of the small intestine.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
43
Substances in food that stimulate the beneficial flora of the large intestine and elicit a health benefit to the host are called _______________.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
44
The _______________ colon ends in the rectum where another sphincter (the anal sphincter) controls voluntary release of intestinal contents.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
45
During a fecal microbiota transplantation, stool is obtained from a healthy donor and is delivered into the GI tract, usually via _______________.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
46
At least two-thirds of IBS patients associate the signs and symptoms they experience with characteristics of the foods that they eat.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
47
The _______________ is the primary site for reabsorption of bile acids.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
48
Damage to the anatomy and physiology of the small intestine due to disease is the most common cause of malabsorption.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
49
_______________ is a measurement of the concentration of particles in solution.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
50
The tissue of the small intestine is circularly folded into folds of Kerckring.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
51
Celiac disease is often associated with other chronic, infectious diseases, including hepatitis, varicella, and cytomegalovirus.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
52
Vitamin K, biotin, and folate are endogenously produced vitamins through interaction with the _______________.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
53
_______________ starch is defined as starch components that enter the large intestine undigested.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
54
_______________ is a hormone secreted by the small intestine that assists in the control of the migrating motility complex.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
55
_______________ absorption is much more difficult due to its insolubility in water.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
56
Treatment for diverticulosis involves nutrition therapy, with a specific focus on fiber intake.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
57
Approximately 95% of patients with ulcerative colitis have disease only involving the rectum.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
58
Consumption of fructans or fructo-oligosaccharides (FOS) has been shown to soften feces and to assist in relieving constipation.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
59
The _______________ absorption test assists in distinguishing between pancreatic dysfunction and small bowel malabsorption.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
60
When defecation relieves cramping, diarrhea is generally from the small intestine.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
61
Absorption of _______________ is of specific concern because it requires adequate ileal receptors and a normal transit time.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
62
List four components of the Rome IV Consensus Criteria for diagnosing constipation.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
63
Describe the process of lipid digestion and absorption in the small intestine.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
64
_______________ symptoms that can occur in the absence of GI problems include bone and joint pain, muscle cramping, fatigue, and peripheral neuropathy.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
65
Briefly describe the process of restriction and reintroduction of dairy products to clients with lactose malabsorption.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
66
A(n) _______________ is a surgically created artificial opening into the abdomen from which waste products can be excreted.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
67
One nutritional intervention for treating IBS is the use of a traditional _______________ diet, which eliminates all possible foods related to the patient's symptoms.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
68
Explain the nutrition assessment for the lower gastrointestinal tract, including the components of client history, anthropometric measurements, and biochemical data. Also, give examples of each component.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
69
Describe what a dietitian would recommend to a client to increase fiber in his or her diet. Also, list examples of fiber-rich foods.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
70
As chyme enters the duodenum from the stomach, the hormone gastrin and the _______________ stimulate the onset of segmental contractions.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
71
Small intestinal bacterial overgrowth syndrome is treated by both correcting the underlying cause and administering medications such as _______________.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
72
Explain the differences between ulcerative colitis and Crohn's disease in terms of clinical manifestations and medical treatment.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
73
The most common surgical procedure in ulcerative colitis is a _______________.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
74
Define the following components that maintain the health of the colon and gut microbiota: resistant starch, prebiotics, probiotics, and synbiotics.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
75
With chronic ulcerative colitis, the intestinal wall can become so thin that the mucosa is ulcerated. This is referred to as _______________.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
76
Briefly describe the segmentation motility associated with digestion in the small intestine.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
77
Describe the FODMAP diet, and give examples of foods included in a low-FODMAP diet plan.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
78
The only current recommendation for fiber supplementation in IBS patients is the use of ispaghula husk, which is more commonly known as _______________.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
79
Explain the etiological factors that are associated with the development of IBS, especially communication between body systems, GI tract function and environment, and GI symptoms.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
80
_______________ supplements, which are triglycerides that contain primarily caprylic (C8) and capric (C10) fatty acids, can be used to increase caloric intake.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck



