Deck 3: Office/Health Center
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question

Unlock Deck
Sign up to unlock the cards in this deck!
Unlock Deck
Unlock Deck
1/900
Play
Full screen (f)
Deck 3: Office/Health Center
1
The fall risk in elderly patients taking a hypnotic medication is being evaluated in a retrospective case-control study. The investigators report the following association between medication consumption and fall incidence over the subsequent week:
Unadjusted odds ratio: 1.40 (95% confidence interval: 1.2-1.6)
Odds ratio adjusted for age and gender: 1.34 (95% confidence interval: 1.1-1.5)
Odds ratio adjusted for age, gender, and handgrip strength: 1.12 (95% confidence interval: 0.8-1.4)
Which of the following is the best interpretation of the study results?
A)Age and gender are not significant predictors of fall occurrence
B)40% of falls in the study population are associated with use of the medication
C)Frailty confounds the association between the medication and fall occurrence
D)The medication causes elderly patients to fall
E)The study is grossly underpowered to detect any meaningful difference
Unadjusted odds ratio: 1.40 (95% confidence interval: 1.2-1.6)
Odds ratio adjusted for age and gender: 1.34 (95% confidence interval: 1.1-1.5)
Odds ratio adjusted for age, gender, and handgrip strength: 1.12 (95% confidence interval: 0.8-1.4)
Which of the following is the best interpretation of the study results?
A)Age and gender are not significant predictors of fall occurrence
B)40% of falls in the study population are associated with use of the medication
C)Frailty confounds the association between the medication and fall occurrence
D)The medication causes elderly patients to fall
E)The study is grossly underpowered to detect any meaningful difference
C
Explanation:
The odds ratio (OR) is a measure of association between an exposure and an outcome. It represents the odds that an outcome will occur given a particular exposure as compared to the odds of the outcome occurring in the absence of that exposure. Odds ratios are most commonly used in case-control studies. For the unadjusted or crude odds ratio, no other factors (eg, confounders) are taken into account. However, confounding factors (eg, age, sex, socioeconomic status) can certainly affect the outcome. ORs may subsequently be adjusted for confounding factors using stratification methods or logistic regression. A fully adjusted odds ratio strips away the effects of all potential confounders, revealing the true association between exposure and outcome.
In this example, adjustment for age and gender reduces the odds ratio slightly to 1.34 (95% confidence interval 1.1-1.5) (Choice A). Although the odds ratio was reduced, an association between medication consumption and falls still exists. However, further adjustment for handgrip strength (a correlate of frailty) reduces the odds ratio to 1.12 with a 95% confidence interval of 0.8-1.4 (which now contains the null hypothesis of 1.0), implying that there is no real association between medication consumption and falls. In other words, frailty is a major confounder of the relationship between medication consumption and falls.
(Choice B) Direct calculation of absolute and relative risk is not possible in case-control studies because the study design does not allow the researcher to calculate disease prevalence. However, if the prevalence of the disease is low, the odds ratio is approximately equal to the relative risk (rare disease assumption).
(Choice D) Case-control studies may prove an association but they cannot demonstrate causation.
(Choice E) Because the 95% confidence interval associated with the crude odds ratio did not contain the null hypothesis, this study was sufficiently powered to detect a difference between exposed and unexposed groups.
Educational objective:
The odds ratio represents the odds that an outcome will occur given a particular exposure compared to the odds of the outcome occurring in the absence of that exposure. No other factors (eg, confounders) are taken into account when calculating the unadjusted or crude odds ratio. Adjustment for confounders allows the true association between exposure and outcome to be calculated (adjusted odds ratio).
__________
References:
Explaining odds ratios.
(http://www.ncbi.nlm.nih.gov/pubmed/20842279)
Statistics notes. the odds ratio.
(http://www.ncbi.nlm.nih.gov/pubmed/10827061)
Explanation:
The odds ratio (OR) is a measure of association between an exposure and an outcome. It represents the odds that an outcome will occur given a particular exposure as compared to the odds of the outcome occurring in the absence of that exposure. Odds ratios are most commonly used in case-control studies. For the unadjusted or crude odds ratio, no other factors (eg, confounders) are taken into account. However, confounding factors (eg, age, sex, socioeconomic status) can certainly affect the outcome. ORs may subsequently be adjusted for confounding factors using stratification methods or logistic regression. A fully adjusted odds ratio strips away the effects of all potential confounders, revealing the true association between exposure and outcome.
In this example, adjustment for age and gender reduces the odds ratio slightly to 1.34 (95% confidence interval 1.1-1.5) (Choice A). Although the odds ratio was reduced, an association between medication consumption and falls still exists. However, further adjustment for handgrip strength (a correlate of frailty) reduces the odds ratio to 1.12 with a 95% confidence interval of 0.8-1.4 (which now contains the null hypothesis of 1.0), implying that there is no real association between medication consumption and falls. In other words, frailty is a major confounder of the relationship between medication consumption and falls.
(Choice B) Direct calculation of absolute and relative risk is not possible in case-control studies because the study design does not allow the researcher to calculate disease prevalence. However, if the prevalence of the disease is low, the odds ratio is approximately equal to the relative risk (rare disease assumption).
(Choice D) Case-control studies may prove an association but they cannot demonstrate causation.
(Choice E) Because the 95% confidence interval associated with the crude odds ratio did not contain the null hypothesis, this study was sufficiently powered to detect a difference between exposed and unexposed groups.
Educational objective:
The odds ratio represents the odds that an outcome will occur given a particular exposure compared to the odds of the outcome occurring in the absence of that exposure. No other factors (eg, confounders) are taken into account when calculating the unadjusted or crude odds ratio. Adjustment for confounders allows the true association between exposure and outcome to be calculated (adjusted odds ratio).
__________
References:
Explaining odds ratios.
(http://www.ncbi.nlm.nih.gov/pubmed/20842279)
Statistics notes. the odds ratio.
(http://www.ncbi.nlm.nih.gov/pubmed/10827061)
2
An analysis of results from 18,317 patients pooled from 5 large randomized controlled trials on drug X revealed the following relative rates (RR) for drug X compared to the control:
RR of cardiovascular mortality = 0.90 (95% confidence interval [CI], 0.73-1.38)
RR of heart failure = 2.09 (95% CI, 1.52-2.88)
RR of myocardial infarction = 1.18 (95% CI, 0.86-1.31)
Based on the results of this meta-analysis, there is a statistically significant increase in which of the following events among patients taking drug X?
A)Cardiovascular mortality and myocardial infarction
B)Cardiovascular mortality only
C)Heart failure and myocardial infarction
D)Heart failure only
E)Myocardial infarction only
RR of cardiovascular mortality = 0.90 (95% confidence interval [CI], 0.73-1.38)
RR of heart failure = 2.09 (95% CI, 1.52-2.88)
RR of myocardial infarction = 1.18 (95% CI, 0.86-1.31)
Based on the results of this meta-analysis, there is a statistically significant increase in which of the following events among patients taking drug X?
A)Cardiovascular mortality and myocardial infarction
B)Cardiovascular mortality only
C)Heart failure and myocardial infarction
D)Heart failure only
E)Myocardial infarction only
D
Explanation:
In this example, the relative risk (RR) is the risk of an event in the exposed (drug X) group compared to the risk of that event in the unexposed (control) group. An RR = 1 indicates no difference in risk, an RR >1 indicates increased risk, and an RR <1 indicates decreased risk. The 95% confidence interval (CI) is a reflection of statistical significance; a CI that crosses the null value (1 in the case of RR) is not statistically significant. Although the RRs for heart failure (RR = 2.09) and myocardial infarction (RR = 1.18) are both >1, the 95% CI for myocardial infarction (95% CI = 0.86-1.31) crosses the null value of 1 and is therefore not statistically significant. Based on these results, there was a significantly increased rate of heart failure only among patients taking drug X.
Educational objective:
The relative risk is the risk of an event in the exposed group compared to the risk of that event in the unexposed group. A confidence interval that crosses the null value is not statistically significant.
__________
Explanation:
In this example, the relative risk (RR) is the risk of an event in the exposed (drug X) group compared to the risk of that event in the unexposed (control) group. An RR = 1 indicates no difference in risk, an RR >1 indicates increased risk, and an RR <1 indicates decreased risk. The 95% confidence interval (CI) is a reflection of statistical significance; a CI that crosses the null value (1 in the case of RR) is not statistically significant. Although the RRs for heart failure (RR = 2.09) and myocardial infarction (RR = 1.18) are both >1, the 95% CI for myocardial infarction (95% CI = 0.86-1.31) crosses the null value of 1 and is therefore not statistically significant. Based on these results, there was a significantly increased rate of heart failure only among patients taking drug X.
Educational objective:
The relative risk is the risk of an event in the exposed group compared to the risk of that event in the unexposed group. A confidence interval that crosses the null value is not statistically significant.
__________
3
A 76-year-old man comes to the office because of lightheadedness. It occurs occasionally while he does yard work and is sometimes accompanied by chest pressure. He denies any syncope, shortness of breath, or palpitations. He has a history of hypertension, hyperlipidemia, gout, and osteoarthritis. He is an ex-smoker.
His blood pressure is 148/78 mm Hg, pulse is 78 /min, and respirations are 16 /min. The patient's pulse oximetry showed 97% on room air. His BMI is 28 kg/m2. Cardiac examination reveals a soft S2. There is a 3/6 late peaking systolic ejection murmur at the right upper sternal border. The carotid, radial, and femoral pulses are 2+ and are not delayed. There is 1+ edema in the lower extremities.
Echocardiogram shows normal left ventricular size and function with moderate concentric left ventricular hypertrophy. The aortic valve is calcified with restricted opening, and the mean gradient across the aortic valve is 50 mm Hg.
Which of the following would be the role of heart catheterization in this patient?
A)Confirm valvular abnormality
B)Define coronary anatomy
C)Measure cardiac output
D)Measure pulmonary arterial pressures
E)Obtain left ventricular ejection fraction
His blood pressure is 148/78 mm Hg, pulse is 78 /min, and respirations are 16 /min. The patient's pulse oximetry showed 97% on room air. His BMI is 28 kg/m2. Cardiac examination reveals a soft S2. There is a 3/6 late peaking systolic ejection murmur at the right upper sternal border. The carotid, radial, and femoral pulses are 2+ and are not delayed. There is 1+ edema in the lower extremities.
Echocardiogram shows normal left ventricular size and function with moderate concentric left ventricular hypertrophy. The aortic valve is calcified with restricted opening, and the mean gradient across the aortic valve is 50 mm Hg.
Which of the following would be the role of heart catheterization in this patient?
A)Confirm valvular abnormality
B)Define coronary anatomy
C)Measure cardiac output
D)Measure pulmonary arterial pressures
E)Obtain left ventricular ejection fraction
B
Explanation:
This patient's presentation is most consistent with severe aortic stenosis, likely due to fibrocalcification. He presents with some of the classic triad of symptoms (angina, dyspnea on exertion, and dizziness/syncope), and he has a soft S2 and late-peaking murmur on examination. Diminished arterial pulses (parvus et tardus) also indicate severe stenosis, but may be absent in older patients with arterial calcification. Echocardiogram usually shows a mean gradient > 40 mm Hg and an aortic valve area < 0.7cm2. Valve replacement is preferred for severe aortic stenosis in symptomatic patients who are operative candidates.
Cardiac catheterization is recommended prior to valve surgery to define the coronary anatomy, since approximately 40% of patients require concurrent coronary artery bypass grafting. Retrograde cardiac catheterization across a severely calcified aortic valve significantly increases the risk of embolic stroke, and should be performed with caution and only when noninvasive techniques cannot provide the desired information. In younger patients with few risk factors for coronary artery disease, coronary CT angiography is being used more frequently.
(Choice A) An echocardiogram with adequate images can sufficiently make the diagnosis of severe aortic stenosis. Cardiac catheterization is only needed to measure the gradient if the echocardiogram images are inadequate or if there is some inconsistency (i.e., the measurements indicate mild stenosis, but the leaflets are calcified and restricted).
(Choices C and D) Pulmonary arterial catheterization is more useful to measure both cardiac output and pulmonary arterial pressures, which are not needed and unlikely to change this patient's management. This may be indicated if there is concern about additional valvular disease (i.e., mitral stenosis), right-sided heart disease, or to assess hemodynamics in the setting of left ventricular dysfunction.
(Choice E) Left ventricular ejection fraction can be adequately assessed with echocardiography, assuming the images are acceptable.
Educational objective:
Cardiac catheterization is recommended prior to valve surgery to define the coronary anatomy, since approximately 40% of patients require concurrent coronary artery bypass grafting. Cardiac catheterization should be done with extreme caution in patients with severe calcific aortic stenosis (due to increased risk of embolic stroke), and only when noninvasive techniques do not provide the desired information.
__________
References:
Should we cross the valve: the risk of retrograde catheterization of the left ventricle in patients with aortic stenosis.
(http://www.ncbi.nlm.nih.gov/pubmed/15215790)
Explanation:
This patient's presentation is most consistent with severe aortic stenosis, likely due to fibrocalcification. He presents with some of the classic triad of symptoms (angina, dyspnea on exertion, and dizziness/syncope), and he has a soft S2 and late-peaking murmur on examination. Diminished arterial pulses (parvus et tardus) also indicate severe stenosis, but may be absent in older patients with arterial calcification. Echocardiogram usually shows a mean gradient > 40 mm Hg and an aortic valve area < 0.7cm2. Valve replacement is preferred for severe aortic stenosis in symptomatic patients who are operative candidates.
Cardiac catheterization is recommended prior to valve surgery to define the coronary anatomy, since approximately 40% of patients require concurrent coronary artery bypass grafting. Retrograde cardiac catheterization across a severely calcified aortic valve significantly increases the risk of embolic stroke, and should be performed with caution and only when noninvasive techniques cannot provide the desired information. In younger patients with few risk factors for coronary artery disease, coronary CT angiography is being used more frequently.
(Choice A) An echocardiogram with adequate images can sufficiently make the diagnosis of severe aortic stenosis. Cardiac catheterization is only needed to measure the gradient if the echocardiogram images are inadequate or if there is some inconsistency (i.e., the measurements indicate mild stenosis, but the leaflets are calcified and restricted).
(Choices C and D) Pulmonary arterial catheterization is more useful to measure both cardiac output and pulmonary arterial pressures, which are not needed and unlikely to change this patient's management. This may be indicated if there is concern about additional valvular disease (i.e., mitral stenosis), right-sided heart disease, or to assess hemodynamics in the setting of left ventricular dysfunction.
(Choice E) Left ventricular ejection fraction can be adequately assessed with echocardiography, assuming the images are acceptable.
Educational objective:
Cardiac catheterization is recommended prior to valve surgery to define the coronary anatomy, since approximately 40% of patients require concurrent coronary artery bypass grafting. Cardiac catheterization should be done with extreme caution in patients with severe calcific aortic stenosis (due to increased risk of embolic stroke), and only when noninvasive techniques do not provide the desired information.
__________
References:
Should we cross the valve: the risk of retrograde catheterization of the left ventricle in patients with aortic stenosis.
(http://www.ncbi.nlm.nih.gov/pubmed/15215790)
4
Cardiovascular disease is the leading cause of morbidity and mortality in women in developed countries. Based on current evidence, which of the following is true for women as compared with men?
A)Women are less likely to receive aggressive treatment for chest pain.
B)Women are more likely to be referred for cardiac catheterization for abnormal stress testing.
C)Women are more likely to get false-positive results on stress imaging studies.
D)Women are more likely to present with typical angina.
E)Women have a lower burden of risk factors during presentation for coronary heart disease.
A)Women are less likely to receive aggressive treatment for chest pain.
B)Women are more likely to be referred for cardiac catheterization for abnormal stress testing.
C)Women are more likely to get false-positive results on stress imaging studies.
D)Women are more likely to present with typical angina.
E)Women have a lower burden of risk factors during presentation for coronary heart disease.

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
5
A 79-year-old woman is referred for perioperative evaluation prior to cataract surgery. Medical history is significant for hypertension, heart failure, mild intermittent asthma, gout, and nonvalvular atrial fibrillation for which she takes warfarin. Medications also include lisinopril, furosemide, carvedilol, and amlodipine. The patient has no history of stroke. Two weeks ago, the INR was 2.5.
Blood pressure is 130/82 mm Hg and pulse is 84/min and irregular. Jugular venous pressure is normal and the lungs are clear to auscultation. The patient has a grade 2/6 systolic ejection murmur at the right upper sternal border without radiation. Pedal edema is not present.
What is the best way to manage this patient's anticoagulation?
A)Continue warfarin with no change in dosing or target INR
B)Discontinue warfarin 5 days prior to procedure and perform perioperative bridging with heparin
C)Hold warfarin until the INR normalizes, then restart warfarin postprocedure with no bridging
D)Permanently discontinue warfarin
E)Reduce warfarin dose and adjust target INR to 1.5 preoperatively
Blood pressure is 130/82 mm Hg and pulse is 84/min and irregular. Jugular venous pressure is normal and the lungs are clear to auscultation. The patient has a grade 2/6 systolic ejection murmur at the right upper sternal border without radiation. Pedal edema is not present.
What is the best way to manage this patient's anticoagulation?
A)Continue warfarin with no change in dosing or target INR
B)Discontinue warfarin 5 days prior to procedure and perform perioperative bridging with heparin
C)Hold warfarin until the INR normalizes, then restart warfarin postprocedure with no bridging
D)Permanently discontinue warfarin
E)Reduce warfarin dose and adjust target INR to 1.5 preoperatively

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
6
A recent study of patients with stage 2 chronic kidney disease (CKD) found that a new drug reduced the progression to end-stage (stage 5) CKD from 37/1,000 placebo-treated cases to 12/1,000 new drug-treated cases over a five-year period.
Which of the following is the number needed to treat in order to obtain a single favorable outcome?
A)2)5
B)10
C)25
D)40
E)100
Which of the following is the number needed to treat in order to obtain a single favorable outcome?
A)2)5
B)10
C)25
D)40
E)100

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
7
A 56-year-old woman who is post-operative day #1 after a laparoscopic cholecystectomy complains of chest discomfort. The patient reports that in the early hours of the morning, she was awakened from sleep with nausea, one episode of vomiting, and persistent burning in her chest. Her only medical history includes hypertension, which has been well-controlled with medication. Her other current medications include ondansetron, acetaminophen, and hydrocodone.
Her temperature is 37.9 C (100.2 F), blood pressure is 92/60 mm Hg, heart rate is 90 /min, and respirations are 18 /min. Her BMI is 31 kg/m2. She is in moderate distress and appears anxious. There is no murmur on cardiac examination and bilateral fine crackles are heard at the lung bases. Her abdomen is distended and non-tender with an incision that is clean and intact. Bowel sounds are diminished. There is no rebound tenderness or rigidity. There is no peripheral edema.
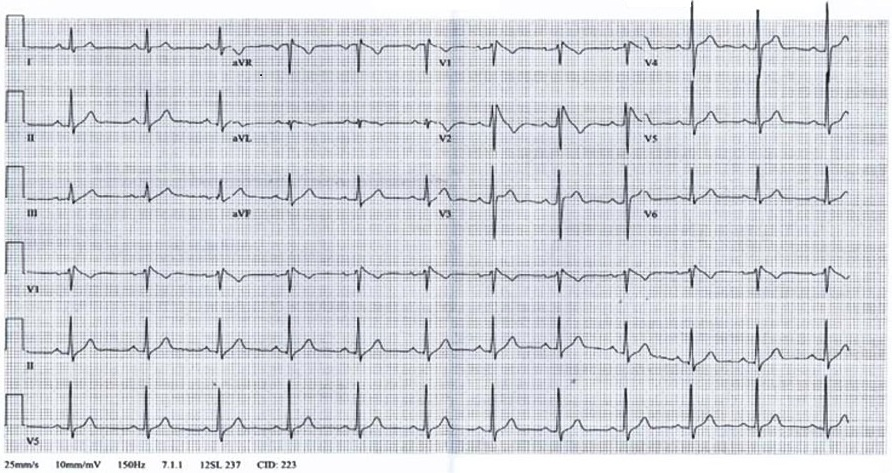
A 12 lead EKG is performed and displayed below:
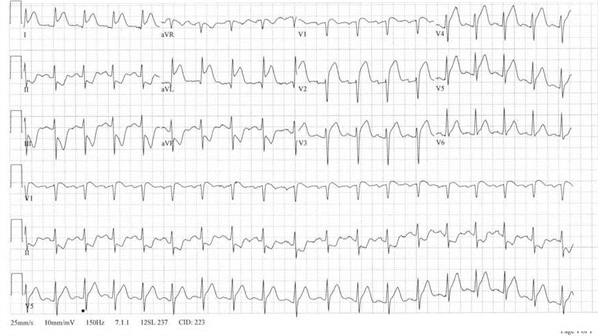
Which of the following would be the most appropriate next step in managing this patient?
A)Coronary angiography
B)CT scan of the chest with contrast
C)Intravenous metoprolol
D)Pantoprazole and morphine
E)Transthoracic echocardiogram
Her temperature is 37.9 C (100.2 F), blood pressure is 92/60 mm Hg, heart rate is 90 /min, and respirations are 18 /min. Her BMI is 31 kg/m2. She is in moderate distress and appears anxious. There is no murmur on cardiac examination and bilateral fine crackles are heard at the lung bases. Her abdomen is distended and non-tender with an incision that is clean and intact. Bowel sounds are diminished. There is no rebound tenderness or rigidity. There is no peripheral edema.
A 12 lead EKG is performed and displayed below:
Which of the following would be the most appropriate next step in managing this patient?
A)Coronary angiography
B)CT scan of the chest with contrast
C)Intravenous metoprolol
D)Pantoprazole and morphine
E)Transthoracic echocardiogram

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
8
A 29-year-old Middle Eastern man is evaluated for difficulty breathing and nonproductive cough for the past month. He reports difficulty walking and frequent falls over the last year but has not seen a physician. The patient has no other medical problems. He is married and has a 3-year-old son.
His blood pressure is 96/60 mm Hg and pulse is 100/min. Jugular venous pressure is estimated at 12 mm H2O. Lung examination shows bibasilar crackles. The point of maximal impulse is displaced to the left and a third heart sound is present. The proximal extremity muscles are atrophied, but both calves are prominently enlarged.
Chest x-ray shows cardiomegaly.
The son's risk of developing his father's condition is closest to which of the following?
A)100%
B)75%
C)50%
D)25%
E)0%
His blood pressure is 96/60 mm Hg and pulse is 100/min. Jugular venous pressure is estimated at 12 mm H2O. Lung examination shows bibasilar crackles. The point of maximal impulse is displaced to the left and a third heart sound is present. The proximal extremity muscles are atrophied, but both calves are prominently enlarged.
Chest x-ray shows cardiomegaly.
The son's risk of developing his father's condition is closest to which of the following?
A)100%
B)75%
C)50%
D)25%
E)0%

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
9
A 67-year-old man comes to the office for routine follow-up. He has a history of hypertension, osteoarthritis, and chronic aortic regurgitation. He reports that he is doing well overall and plays doubles tennis three times a week for exercise, which he does without any chest pain or pressure. He denies shortness of breath, orthopnea, paroxysmal nocturnal dyspnea, or edema. His medications include aspirin, nebivolol, simvastatin, chlorthalidone, and acetaminophen.
His blood pressure is 128/60 mm Hg and pulse is 67 /min. His BMI is 27 kg/m2. Cardiovascular examination reveals a normal S1 and S2. There is 2/6 mid-systolic murmur at the right upper sternal border followed by a high-pitched diastolic decrescendo murmur best heard at the left upper sternal border. The intensity of the diastolic murmur is increased with handgrip. His peripheral pulses are 3+ bilaterally.
A transthoracic echocardiogram demonstrates normal left ventricular size and function. The aortic valve is calcified and demonstrates mild stenosis (mean gradient = 13 mm Hg) with moderate aortic regurgitation. When compared to the echocardiogram from two years ago, both the aortic stenosis and regurgitation are worse.
Which of the following would be the most appropriate next step?
A)Aortic valve replacement
B)Coronary angiography
C)Lisinopril
D)Repeat echocardiogram in 6-12 months
E)Transesophageal echocardiography
His blood pressure is 128/60 mm Hg and pulse is 67 /min. His BMI is 27 kg/m2. Cardiovascular examination reveals a normal S1 and S2. There is 2/6 mid-systolic murmur at the right upper sternal border followed by a high-pitched diastolic decrescendo murmur best heard at the left upper sternal border. The intensity of the diastolic murmur is increased with handgrip. His peripheral pulses are 3+ bilaterally.
A transthoracic echocardiogram demonstrates normal left ventricular size and function. The aortic valve is calcified and demonstrates mild stenosis (mean gradient = 13 mm Hg) with moderate aortic regurgitation. When compared to the echocardiogram from two years ago, both the aortic stenosis and regurgitation are worse.
Which of the following would be the most appropriate next step?
A)Aortic valve replacement
B)Coronary angiography
C)Lisinopril
D)Repeat echocardiogram in 6-12 months
E)Transesophageal echocardiography

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
10
A 36-year-old man comes to the physician with decreased appetite, right-sided facial pain, and fever. He also complains of scant nasal discharge. He has had 3 episodes of sinusitis over the last year that responded well to amoxicillin-clavulanate. Six months ago, he was hospitalized with pneumonia and treated with intravenous antibiotics. His past medical history is unremarkable. He does not use tobacco, alcohol, or illicit drugs. He lives with his girlfriend and has 1 child.
His temperature is 38.3° C (101° F), blood pressure is 144/90 mm Hg, and pulse is 90/min. The right maxillary sinus is tender to palpation. He has 3 small, mobile submandibular nodes. Cardiopulmonary examination is within normal limits. Both upper extremities and the chest have areas of hypopigmented skin.
Laboratory results are as follows:

Urinalysis is unremarkable. Rapid HIV test is negative.
Which of the following conditions is the most likely diagnosis?
A)Common variable immunodeficiency
B)Cystic fibrosis
C)Granulomatosis with polyangiitis (Wegener's granulomatosis)
D)Myeloperoxidase deficiency
E)Primary ciliary dyskinesia
His temperature is 38.3° C (101° F), blood pressure is 144/90 mm Hg, and pulse is 90/min. The right maxillary sinus is tender to palpation. He has 3 small, mobile submandibular nodes. Cardiopulmonary examination is within normal limits. Both upper extremities and the chest have areas of hypopigmented skin.
Laboratory results are as follows:

Urinalysis is unremarkable. Rapid HIV test is negative.
Which of the following conditions is the most likely diagnosis?
A)Common variable immunodeficiency
B)Cystic fibrosis
C)Granulomatosis with polyangiitis (Wegener's granulomatosis)
D)Myeloperoxidase deficiency
E)Primary ciliary dyskinesia

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
11
A 50-year-old man asks about starting a statin to treat his LDL of 130 mg/dL. He has no family history of coronary artery or cerebrovascular disease. He does not smoke, has a normal blood pressure, and is a competitive runner. The patient is especially concerned about the possibility of developing musculoskeletal symptoms that would impact his running. He has read extensively on the subject and specifically requests help in interpreting some studies. In one study, none of 5000 controls and 250 of 5000 statin-treated individuals developed musculoskeletal symptoms. He asks how many patients need to be treated for 1 patient to have musculoskeletal symptoms.
What is the number needed to harm in this study?
A)200
B)20
C)2
D)5
E)50
What is the number needed to harm in this study?
A)200
B)20
C)2
D)5
E)50

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
12
In a study comparing treatment to placebo, the relative risk is given as 2.28 in favor of the treatment group with a 95% confidence interval of 1.32-3.96.
Which of the following represents the best interpretation of the 95% confidence interval?
A)About 95% of patients in the treatment group had a risk between 1.32 and 3.96
B)If the study were repeated 100 times, the confidence interval would be 1.32-3.96 in 95% of cases
C)If the study were repeated 100 times, the relative risk would be 2.28 in 95% of cases
D)If the study were repeated 100 times, the relative risk would be between 1.32 and 3.96 in 95% of cases
E)The results are not statistically significant because the confidence interval does not cross 1.0
Which of the following represents the best interpretation of the 95% confidence interval?
A)About 95% of patients in the treatment group had a risk between 1.32 and 3.96
B)If the study were repeated 100 times, the confidence interval would be 1.32-3.96 in 95% of cases
C)If the study were repeated 100 times, the relative risk would be 2.28 in 95% of cases
D)If the study were repeated 100 times, the relative risk would be between 1.32 and 3.96 in 95% of cases
E)The results are not statistically significant because the confidence interval does not cross 1.0

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
13
A 45-year-old woman comes to the physician because of chronic nasal congestion. Her symptoms began years ago, but they have worsened lately. She often has paroxysms of 10-12 sneezes, especially when waking up in the morning. She also complains of chronic rhinorrhea and post-nasal drip, and she occasionally has itchy eyes. She is unsure if there is a seasonal component to her symptoms, but they may be worse in the Spring. She does not use aspirin and has not had any episodes of sinusitis. She has tried chlorpheniramine in the past, but it made her drowsy. She does not smoke tobacco or drink alcohol and she denies cocaine or other illicit drug use. She has mild hypertension but is in good health otherwise.
Her blood pressure is 134/84 mm Hg and pulse is 67/min. Her nares are patent with a clear discharge. There are no nasal polyps or septal deviation. The turbinates are pale and her conjunctivae appear normal. Neck, pulmonary, and cardiovascular examinations are within normal limits.
Which of the following is the best next step in this patient's management?
A)Leukotriene inhibitor
B)Nasal corticosteroid spray
C)Nasal decongestant spray
D)Oral decongestant
E)Oral non-sedating antihistamine
Her blood pressure is 134/84 mm Hg and pulse is 67/min. Her nares are patent with a clear discharge. There are no nasal polyps or septal deviation. The turbinates are pale and her conjunctivae appear normal. Neck, pulmonary, and cardiovascular examinations are within normal limits.
Which of the following is the best next step in this patient's management?
A)Leukotriene inhibitor
B)Nasal corticosteroid spray
C)Nasal decongestant spray
D)Oral decongestant
E)Oral non-sedating antihistamine

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
14
A 67-year-old male seeks follow-up after a screening ultrasound at a health fair showed an abdominal aortic aneurysm. He has no symptoms and specifically denies claudication. He smoked 1-2 packs of cigarettes per day for 35 years and stopped 10 years ago. He has been told that his cholesterol was high in the past.
His temperature is 37.1 C (98.7 F), blood pressure is 142/92 mm Hg, pulse is 72/min and respirations are 14/min. His Body Mass Index is 29 kg/m2. Examination of the heart, chest, and abdomen are unremarkable. His lower extremity pulses are 2+ with good upstroke.
The patient's laboratory data obtained at the health fair showed a normal complete blood count. His total cholesterol was 240 mg/dL, low density lipoprotein 140 mg/dL, and high density lipoprotein 40 mg/dL. His serum creatinine was 1.3 mg/dL, and the remainder of his laboratory tests were normal. The abdominal ultrasound report revealed an infrarenal abdominal aortic aneurysm with a diameter of 4.2 centimeters.
In addition to addressing the patient's abnormal lipids and blood pressure, which of the following represents the best option at present?
A)Re-measure the aneurysm in 3 months
B)Re-measure the aneurysm in 6-12 months
C)Refer for endovascular repair
D)Refer for open repair
E)Schedule an abdominal CT scan
His temperature is 37.1 C (98.7 F), blood pressure is 142/92 mm Hg, pulse is 72/min and respirations are 14/min. His Body Mass Index is 29 kg/m2. Examination of the heart, chest, and abdomen are unremarkable. His lower extremity pulses are 2+ with good upstroke.
The patient's laboratory data obtained at the health fair showed a normal complete blood count. His total cholesterol was 240 mg/dL, low density lipoprotein 140 mg/dL, and high density lipoprotein 40 mg/dL. His serum creatinine was 1.3 mg/dL, and the remainder of his laboratory tests were normal. The abdominal ultrasound report revealed an infrarenal abdominal aortic aneurysm with a diameter of 4.2 centimeters.
In addition to addressing the patient's abnormal lipids and blood pressure, which of the following represents the best option at present?
A)Re-measure the aneurysm in 3 months
B)Re-measure the aneurysm in 6-12 months
C)Refer for endovascular repair
D)Refer for open repair
E)Schedule an abdominal CT scan

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
15
A 43-year-old woman is being evaluated for a heart murmur. She is physically active and takes a yoga class three times a week without difficulty. She exercises on a treadmill twice per week. She denies any chest pain or pressure, palpitations, and shortness of breath.
She had arthroscopic knee surgery two years ago after sustaining a knee injury while running. Otherwise, her past medical history is unremarkable.
Her blood pressure is 122/78 mm Hg and pulse is 67 /min. Her BMI is 25 kg/m2. There is a blowing 3/6 holosystolic murmur heard best at the apex. Lungs are clear on auscultation. Her physical examination is otherwise unremarkable.
EKG shows normal sinus rhythm with non-specific ST segment and T wave changes. Echocardiogram shows normal left ventricular size and function, an ejection fraction of 65%, and posterior mitral leaflet prolapse with severe eccentric mitral regurgitation. Left atrial size is moderately increased. Pulmonary artery systolic pressure is estimated at 25 mm Hg.
Which of the following is the best recommendation for this patient?
A)Antibiotic prophylaxis prior to dental work
B)Anticoagulation with warfarin
C)Cardiac catheterization
D)Mitral valve replacement
E)Repeat echocardiogram in 6 months
She had arthroscopic knee surgery two years ago after sustaining a knee injury while running. Otherwise, her past medical history is unremarkable.
Her blood pressure is 122/78 mm Hg and pulse is 67 /min. Her BMI is 25 kg/m2. There is a blowing 3/6 holosystolic murmur heard best at the apex. Lungs are clear on auscultation. Her physical examination is otherwise unremarkable.
EKG shows normal sinus rhythm with non-specific ST segment and T wave changes. Echocardiogram shows normal left ventricular size and function, an ejection fraction of 65%, and posterior mitral leaflet prolapse with severe eccentric mitral regurgitation. Left atrial size is moderately increased. Pulmonary artery systolic pressure is estimated at 25 mm Hg.
Which of the following is the best recommendation for this patient?
A)Antibiotic prophylaxis prior to dental work
B)Anticoagulation with warfarin
C)Cardiac catheterization
D)Mitral valve replacement
E)Repeat echocardiogram in 6 months

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
16
A nuclear stress test using a new radioisotope tracer has a sensitivity of 60% and specificity of 80% for detecting hemodynamically significant coronary artery disease, defined as coronary artery narrowing > 50% by coronary angiography. In a patient with a pre-test probability for coronary artery disease of 40%, what is the positive likelihood ratio for the test?
A)0)5
B)1
C)2
D)3
E)4
A)0)5
B)1
C)2
D)3
E)4

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
17
An ultrasound evaluation of the extracranial portion of the internal carotid artery can predict significant (> 70%) angiographic stenosis with a sensitivity of 100% and a specificity of 72%. When this test is applied to a large population of patients with multiple cardiovascular risk factors, which of the following test parameters is expected to be closest to 100%?
A)Accuracy
B)False discovery rate
C)Negative predictive value
D)Positive predictive value
E)Reproducibility
A)Accuracy
B)False discovery rate
C)Negative predictive value
D)Positive predictive value
E)Reproducibility

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
18
A 69-year-old woman comes to the physician with right calf pain when walking. The pain has been present for several months but is now starting to limit her daily walks and shopping. It is described as a deep ache or cramp. The pain initially occurred after the patient walked 6 blocks, but now occurs after 2 blocks. It dissipates rapidly with rest. She has no chest pain or leg edema. The patient has a history of hypertension, hyperlipidemia, diet-controlled type 2 diabetes mellitus, and cigarette use. She has reduced her smoking to about 10 cigarettes a day. Her medications include simvastatin, ramipril, aspirin, calcium, and vitamin D.
The patient's blood pressure is 128/77 mm Hg and pulse is 72/min. Cardiac, lung, and abdominal examinations are unremarkable. Her femoral pulses are 2+ and symmetrical. Popliteal and dorsalis pedis pulses on the right feel diminished relative to the left. Her ankle-brachial index is 0.7 on the right and 0.9 on the left.
Electrocardiogram shows normal sinus rhythm and non-specific ST-segment and T-wave changes.
After smoking cessation, aggressive risk factor modification, and a supervised incremental walking program, which of the following would be the best next step in management if life-style-limiting claudication persists?
A)Cilostazol
B)Pentoxifylline
C)Revascularization therapy
D)Verapamil
E)Warfarin
The patient's blood pressure is 128/77 mm Hg and pulse is 72/min. Cardiac, lung, and abdominal examinations are unremarkable. Her femoral pulses are 2+ and symmetrical. Popliteal and dorsalis pedis pulses on the right feel diminished relative to the left. Her ankle-brachial index is 0.7 on the right and 0.9 on the left.
Electrocardiogram shows normal sinus rhythm and non-specific ST-segment and T-wave changes.
After smoking cessation, aggressive risk factor modification, and a supervised incremental walking program, which of the following would be the best next step in management if life-style-limiting claudication persists?
A)Cilostazol
B)Pentoxifylline
C)Revascularization therapy
D)Verapamil
E)Warfarin

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
19
A large multicenter double-blinded randomized placebo-controlled study is being planned to evaluate a new medication. Primary endpoints addressing mortality benefits are chosen, and a comprehensive analysis strategy is specified, including for predefined subgroups.
In discussing the advantages of this study design, which of the following represents a benefit of randomization?
A)Randomization can be performed at the level of subgroup analysis
B)Randomization distributes known and unknown variables equally among the study groups
C)Randomization ensures that the study results are statistically significant
D)Randomization ensures that the study sample is representative of the population
E)Randomization prevents group allocation concealment from study participants and investigators
In discussing the advantages of this study design, which of the following represents a benefit of randomization?
A)Randomization can be performed at the level of subgroup analysis
B)Randomization distributes known and unknown variables equally among the study groups
C)Randomization ensures that the study results are statistically significant
D)Randomization ensures that the study sample is representative of the population
E)Randomization prevents group allocation concealment from study participants and investigators

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
20
A new nuclear stress test modality is tested in a broad range of patients with suspected coronary artery disease. The patients' pre-test probability of having the disease is determined by their Framingham score. Their post-test probability is then calculated using the results of the new test, and the following curves are constructed.
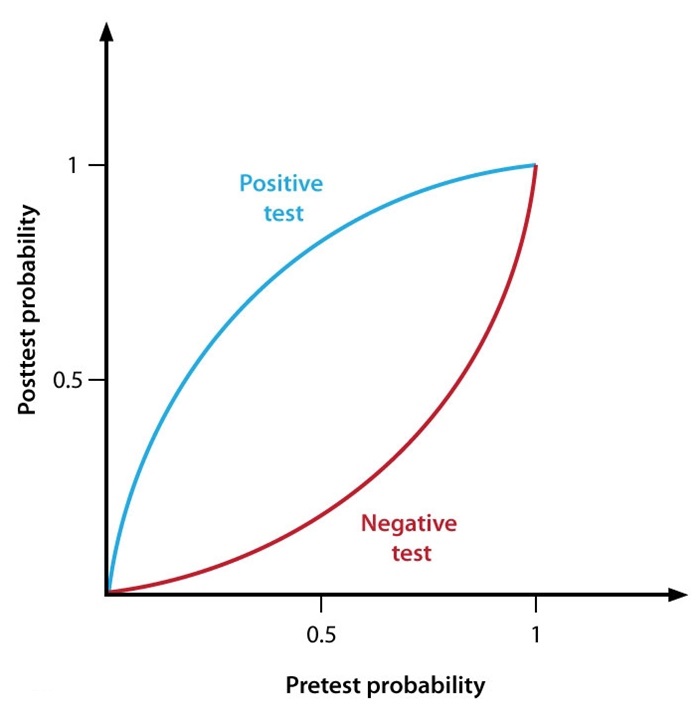
The new test is most useful for diagnosing coronary artery disease in patients with which of the following pretest probabilities?
A)< 10%
B)10%-20%
C)40%-60%
D)80%-90%
E)> 90%
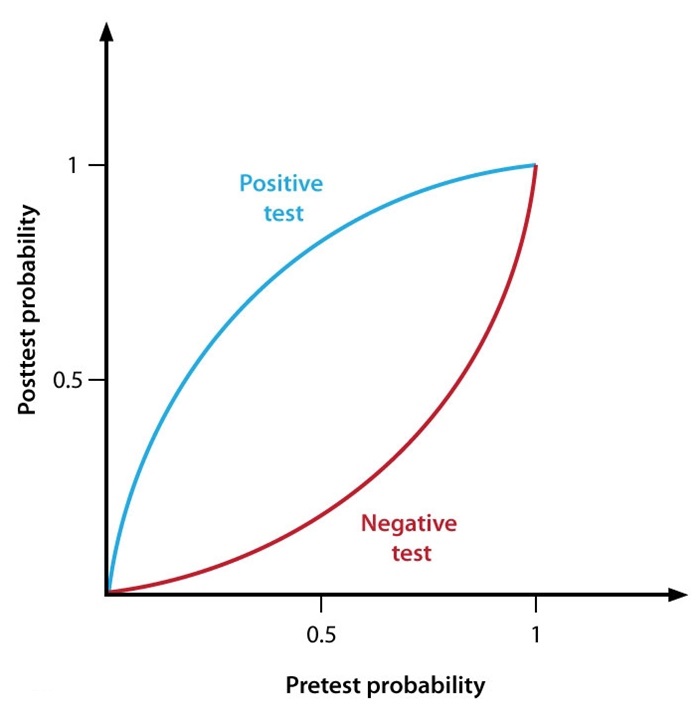
The new test is most useful for diagnosing coronary artery disease in patients with which of the following pretest probabilities?
A)< 10%
B)10%-20%
C)40%-60%
D)80%-90%
E)> 90%

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
21
A 42-year-old woman comes to the physician before undergoing tooth extraction. She recently saw a dentist for lower jaw pain and was told that she needs extraction of a left lower molar. She has a past history of rheumatic heart disease and had mitral valve replacement at 35 years of age with a mechanical valve. She moved to the United States from the Philippines 3 years ago. Her past medical history is otherwise unremarkable. She takes warfarin daily and has been taking amoxicillin for the past 7 days for presumed "tooth infection."
Physical examination reveals crisp opening and closing clicks of a mechanical prosthetic mitral valve. No abnormal murmurs are heard. Her last INR was 2.6.
Which of the following is the most appropriate management for this patient?
A)Continue warfarin and proceed with dental extraction
B)Hold warfarin, give subcutaneous vitamin K, and proceed with dental extraction
C)Hold warfarin until INR is < 1.5, bridge with subcutaneous enoxaparin, and proceed with dental extraction
D)Hold warfarin, wait until INR is < 1.5, and proceed with dental extraction
E)Hold warfarin, wait until INR is < 2.0, and proceed with dental extraction
Physical examination reveals crisp opening and closing clicks of a mechanical prosthetic mitral valve. No abnormal murmurs are heard. Her last INR was 2.6.
Which of the following is the most appropriate management for this patient?
A)Continue warfarin and proceed with dental extraction
B)Hold warfarin, give subcutaneous vitamin K, and proceed with dental extraction
C)Hold warfarin until INR is < 1.5, bridge with subcutaneous enoxaparin, and proceed with dental extraction
D)Hold warfarin, wait until INR is < 1.5, and proceed with dental extraction
E)Hold warfarin, wait until INR is < 2.0, and proceed with dental extraction

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
22
A 78-year-old woman comes to the physician following discharge from the hospital. One week ago, she had gone to the emergency department for palpitations, which she had experienced several times before, and she was diagnosed with atrial fibrillation with rapid ventricular response. The arrhythmia resolved spontaneously overnight, and the patient was discharged the following day. She has no chest pain or shortness of breath and has never had syncope.
Past medical history includes hypertension and hyperlipidemia. The patient's medications include aspirin, diltiazem, atorvastatin, and ramipril. She exercises most days of the week on a stationary bicycle for 20-30 minutes without any difficulty. The patient volunteers at a senior center and helps care for her husband with Alzheimer's dementia.
Blood pressure is 135/75 mm Hg, pulse is 75 and regular, and BMI is 25 kg/m2. Cardiac auscultation shows no murmurs. Her lungs are clear. Distal pulses are normal and symmetric. There is no edema.
Electrocardiogram (ECG) shows normal sinus rhythm with no significant repolarization abnormalities. Transthoracic echocardiogram shows a mildly dilated left atrium, left ventricular ejection fraction of 55%, and mild mitral and tricuspid regurgitation.
Laboratory studies show a TSH of 2.9 µU/mL.
Which of the following is the most appropriate next step in management?
A)Amiodarone
B)Anticoagulation
C)Beta blocker
D)Exercise stress test
E)Transesophageal echocardiogram
Past medical history includes hypertension and hyperlipidemia. The patient's medications include aspirin, diltiazem, atorvastatin, and ramipril. She exercises most days of the week on a stationary bicycle for 20-30 minutes without any difficulty. The patient volunteers at a senior center and helps care for her husband with Alzheimer's dementia.
Blood pressure is 135/75 mm Hg, pulse is 75 and regular, and BMI is 25 kg/m2. Cardiac auscultation shows no murmurs. Her lungs are clear. Distal pulses are normal and symmetric. There is no edema.
Electrocardiogram (ECG) shows normal sinus rhythm with no significant repolarization abnormalities. Transthoracic echocardiogram shows a mildly dilated left atrium, left ventricular ejection fraction of 55%, and mild mitral and tricuspid regurgitation.
Laboratory studies show a TSH of 2.9 µU/mL.
Which of the following is the most appropriate next step in management?
A)Amiodarone
B)Anticoagulation
C)Beta blocker
D)Exercise stress test
E)Transesophageal echocardiogram

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
23
A 23-year-old man comes to the physician for evaluation of a murmur. He has no complaints and describes his exercise tolerance as 'excellent.' He has no other medical conditions and takes no medications. He does not use tobacco, alcohol, or illicit drugs. His paternal uncle died from an unknown cause at a young age.
Physical examination reveals a IV/VI holosystolic murmur which is best heard at the fourth intercostal space along the left sternal border. It is accompanied by a palpable thrill. Carotid pulses are 2+ bilaterally without delay. Otherwise, his physical examination is unremarkable.
Which of the following is the most likely diagnosis?
A)Atrial septal defect
B)Bicuspid aortic valve
C)Ebstein's anomaly
D)Supravalvular aortic stenosis
E)Ventricular septal defect
Physical examination reveals a IV/VI holosystolic murmur which is best heard at the fourth intercostal space along the left sternal border. It is accompanied by a palpable thrill. Carotid pulses are 2+ bilaterally without delay. Otherwise, his physical examination is unremarkable.
Which of the following is the most likely diagnosis?
A)Atrial septal defect
B)Bicuspid aortic valve
C)Ebstein's anomaly
D)Supravalvular aortic stenosis
E)Ventricular septal defect

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
24
A 39-year-old man comes to the physician after he loses consciousness. His wife reports that they were at a school play when she heard her husband making some "gurgling noises." When she looked over at him, he looked "out of it" and started slumping towards her. She could not awaken him. After about ten seconds, he regained consciousness. He denies any prodrome of chest pain or pressure, shortness of breath, or palpitations. He currently has no complaints.
He denies any prior history of syncope or presyncope. He is physically active and plays in a doubles tennis league three times per week. He takes no medications on a regular basis. His family history is unknown as he was adopted.
His blood pressure is 115/70 mm Hg, pulse is 67/min, and BMI is 23 kg/m2. The patient is in no distress. There is a normal S1 and S2 and no murmurs are appreciated. His lungs are clear to auscultation. The abdomen is soft and non-distended. The peripheral pulses are 2+ and symmetric.
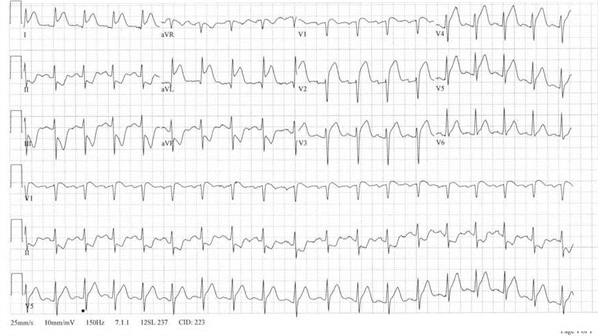
His EKG is shown is this exhibit.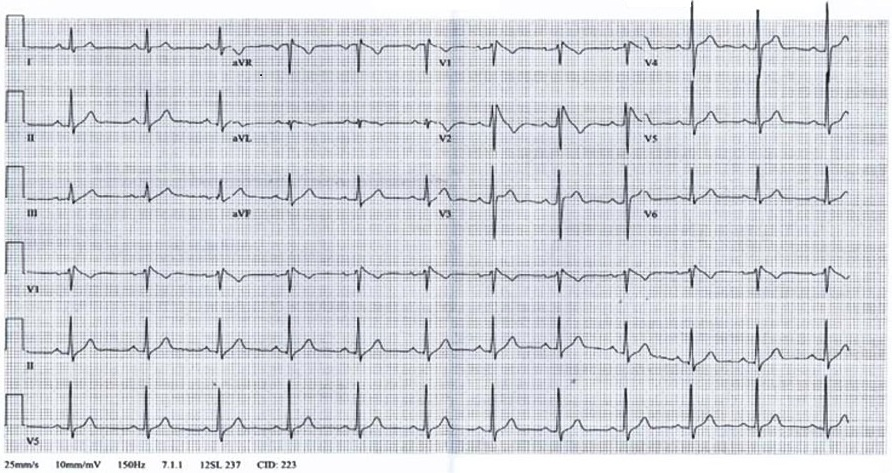
Which of the following is the most likely diagnosis?
A)Acute anterior wall myocardial infarction
B)Brugada syndrome
C)Hypertrophic cardiomyopathy
D)Vasovagal syncope
E)Wolff-Parkinson-White syndrome
He denies any prior history of syncope or presyncope. He is physically active and plays in a doubles tennis league three times per week. He takes no medications on a regular basis. His family history is unknown as he was adopted.
His blood pressure is 115/70 mm Hg, pulse is 67/min, and BMI is 23 kg/m2. The patient is in no distress. There is a normal S1 and S2 and no murmurs are appreciated. His lungs are clear to auscultation. The abdomen is soft and non-distended. The peripheral pulses are 2+ and symmetric.
His EKG is shown is this exhibit.
Which of the following is the most likely diagnosis?
A)Acute anterior wall myocardial infarction
B)Brugada syndrome
C)Hypertrophic cardiomyopathy
D)Vasovagal syncope
E)Wolff-Parkinson-White syndrome

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
25
A 75-year-old man residing in a nursing home comes to the office due to episodic lightheadedness over the last 6 months. He feels like he is "graying out" and then has to lie down and close his eyes. The patient has lost consciousness twice over the past 2 months. Tonic-clonic movements have not been observed and there is no associated incontinence. He has not had chest pain, nausea, palpitations, headache, or speech difficulties. The patient's appetite has been good and he eats 3 meals a day. He describes mild lightheadedness occasionally in the morning, but the more severe episodes usually occur between 2:00 and 3:00 PM and around 8:00 PM.
The patient has a history of hypertension, hyperlipidemia, mild cognitive impairment, and type 2 diabetes mellitus. Current medications include hydrochlorothiazide, metformin, rosuvastatin, lisinopril, and low-dose aspirin. There have been no recent changes in his medications.
Blood pressure is 124/82 mm Hg supine and 116/80 mm Hg upright, pulse is 84/min in both positions, and respirations are 14/min. Cardiac, lung, and abdominal examinations are unremarkable. Neurologic examination reveals a decreased sensation to light touch in both distal lower extremities and absent ankle deep tendon reflexes bilaterally.
Fasting laboratory results are as follows:
 Which of the following is most likely to provide symptomatic improvement in this patient?
Which of the following is most likely to provide symptomatic improvement in this patient?
A)Balance training exercises
B)Discontinuation of rosuvastatin
C)High-carbohydrate meals
D)Smaller and more frequent meals
E)Tighter glucose control
The patient has a history of hypertension, hyperlipidemia, mild cognitive impairment, and type 2 diabetes mellitus. Current medications include hydrochlorothiazide, metformin, rosuvastatin, lisinopril, and low-dose aspirin. There have been no recent changes in his medications.
Blood pressure is 124/82 mm Hg supine and 116/80 mm Hg upright, pulse is 84/min in both positions, and respirations are 14/min. Cardiac, lung, and abdominal examinations are unremarkable. Neurologic examination reveals a decreased sensation to light touch in both distal lower extremities and absent ankle deep tendon reflexes bilaterally.
Fasting laboratory results are as follows:
 Which of the following is most likely to provide symptomatic improvement in this patient?
Which of the following is most likely to provide symptomatic improvement in this patient?A)Balance training exercises
B)Discontinuation of rosuvastatin
C)High-carbohydrate meals
D)Smaller and more frequent meals
E)Tighter glucose control

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
26
A 25-year-old immigrant from the Ukraine comes to the office because of exertional shortness of breath. He was an avid soccer player five years ago, but now describes fatigue and shortness of breath after brisk walking for 5-6 blocks. He denies any chest pain, palpitations, syncope, or lower extremity swelling. His weight has been stable. He takes no medications and has no allergies. He smokes 1 pack of cigarettes daily and drinks alcohol over the weekend. His grandfather died suddenly at the age of 34 years, but both his parents are in good health.
His blood pressure is 105/70 mm Hg in the right arm and 107/72 mm Hg in the left arm, and his pulse is 76/min. Cardiovascular examination reveals a normal apical impulse. There is a normal S1 with a fixed and wide split S2. There is no S3. He has a 2/6 mid-systolic murmur along the left upper sternal border. Femoral pulses are 2+ bilaterally and symmetrical. There is no peripheral edema.
The EKG shows normal sinus rhythm, right axis deviation, and incomplete right bundle branch block.
Which of the following is the most likely finding on transthoracic echocardiography?
A)Bicuspid aortic valve
B)Left ventricular hypertrophy
C)Mitral stenosis
D)Right ventricular enlargement
E)Ventricular septal defect
His blood pressure is 105/70 mm Hg in the right arm and 107/72 mm Hg in the left arm, and his pulse is 76/min. Cardiovascular examination reveals a normal apical impulse. There is a normal S1 with a fixed and wide split S2. There is no S3. He has a 2/6 mid-systolic murmur along the left upper sternal border. Femoral pulses are 2+ bilaterally and symmetrical. There is no peripheral edema.
The EKG shows normal sinus rhythm, right axis deviation, and incomplete right bundle branch block.
Which of the following is the most likely finding on transthoracic echocardiography?
A)Bicuspid aortic valve
B)Left ventricular hypertrophy
C)Mitral stenosis
D)Right ventricular enlargement
E)Ventricular septal defect

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
27
A 40-year-old man comes to the physician for an insurance physical. He has no current complaints. His medical problems include borderline hypertension and seasonal allergies. He takes fexofenadine. He does not smoke and drinks 1-2 alcoholic beverages per weekend. His family history is remarkable for an uncle who died suddenly in his 30s while playing basketball. His older brother had two unexplained syncopes.
His blood pressure is 120/70 mm Hg, pulse is 88 /min, and respirations are 12 /min. The patient's pulse oximetry showed 98% on room air. His BMI is 23 kg/m2. There is a 3/6 systolic murmur heard at the mid and upper sternum bilaterally. Carotid upstrokes are delayed. The intensity of the murmur decreases when the patient assumes a standing position from a sitting position.
Which of the following is the most likely diagnosis?
A)Ebstein's anomaly
B)Hypertrophic cardiomyopathy
C)Mitral valve prolapse
D)Valvular aortic stenosis
E)Ventricular septal defect
His blood pressure is 120/70 mm Hg, pulse is 88 /min, and respirations are 12 /min. The patient's pulse oximetry showed 98% on room air. His BMI is 23 kg/m2. There is a 3/6 systolic murmur heard at the mid and upper sternum bilaterally. Carotid upstrokes are delayed. The intensity of the murmur decreases when the patient assumes a standing position from a sitting position.
Which of the following is the most likely diagnosis?
A)Ebstein's anomaly
B)Hypertrophic cardiomyopathy
C)Mitral valve prolapse
D)Valvular aortic stenosis
E)Ventricular septal defect

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
28
A 32-year old woman comes to the physician because of shortness of breath while walking uphill or climbing steps for the last 3 months. She immigrated with her family to the United States from Thailand 15 years ago. She is a nurse's aide and had a recent work physical performed prior to starting a new job. The physician noted "irregular heart sounds" and performed an EKG, which showed atrial fibrillation with a ventricular rate of 85 beats per minute.
A transthoracic echocardiogram showed normal left ventricular size and function with an ejection fraction of 60%. The left atrium was severely dilated and the mitral valve leaflets were thickened with restricted motion and mild focal calcification. The mitral valve area was calculated at 1.0 cm2 (normal 4-6 cm2) with a moderate degree of mitral regurgitation. The aortic valve was trileaflet without stenosis or regurgitation. There was moderate tricuspid regurgitation with an estimated pulmonary artery systolic pressure of 72 mm Hg, consistent with severe pulmonary hypertension (normal < 30 mm Hg).
Which of the following is a contraindication to percutaneous mitral balloon valvotomy in this patient?
A)Atrial fibrillation
B)Calcification of mitral valve
C)Degree of mitral regurgitation
D)Enlarged left atrium
E)Severity of pulmonary hypertension
A transthoracic echocardiogram showed normal left ventricular size and function with an ejection fraction of 60%. The left atrium was severely dilated and the mitral valve leaflets were thickened with restricted motion and mild focal calcification. The mitral valve area was calculated at 1.0 cm2 (normal 4-6 cm2) with a moderate degree of mitral regurgitation. The aortic valve was trileaflet without stenosis or regurgitation. There was moderate tricuspid regurgitation with an estimated pulmonary artery systolic pressure of 72 mm Hg, consistent with severe pulmonary hypertension (normal < 30 mm Hg).
Which of the following is a contraindication to percutaneous mitral balloon valvotomy in this patient?
A)Atrial fibrillation
B)Calcification of mitral valve
C)Degree of mitral regurgitation
D)Enlarged left atrium
E)Severity of pulmonary hypertension

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
29
A 54-year-old man comes to the clinic 6 weeks after being discharged from the hospital for treatment of aortic valve endocarditis. He has no concerns and says that he feels "fine." The patient's endocarditis was caused by Enterococcus and occurred following cystoscopic evaluation of hematuria. Transesophageal echocardiography during hospitalization showed moderate aortic regurgitation and a 5-mm vegetation on the non-coronary cusp of the aortic valve.
The patient had an uncomplicated hospital stay and completed a full course of intravenous antibiotics as an outpatient. His other medical problems include peptic ulcer disease, kidney stones, and gout. He does not use tobacco. His father had a stroke at age 72.
Temperature is 36.7 C (98 F), blood pressure is 124/78 mm Hg, and pulse is 78/min. The lungs are clear to auscultation. No murmurs are present.
ECG shows normal sinus rhythm and nonspecific T-wave changes. Transthoracic echocardiogram shows normal left ventricular size, a left ventricular ejection fraction of 65%, and moderate eccentric aortic regurgitation.
Which of the following is the next best step in management of this patient?
A)Angiotensin II receptor blocker therapy
B)Education on antibiotic prophylaxis
C)Exercise stress testing
D)Long-term anticoagulation therapy
E)Transesophageal echocardiogram
The patient had an uncomplicated hospital stay and completed a full course of intravenous antibiotics as an outpatient. His other medical problems include peptic ulcer disease, kidney stones, and gout. He does not use tobacco. His father had a stroke at age 72.
Temperature is 36.7 C (98 F), blood pressure is 124/78 mm Hg, and pulse is 78/min. The lungs are clear to auscultation. No murmurs are present.
ECG shows normal sinus rhythm and nonspecific T-wave changes. Transthoracic echocardiogram shows normal left ventricular size, a left ventricular ejection fraction of 65%, and moderate eccentric aortic regurgitation.
Which of the following is the next best step in management of this patient?
A)Angiotensin II receptor blocker therapy
B)Education on antibiotic prophylaxis
C)Exercise stress testing
D)Long-term anticoagulation therapy
E)Transesophageal echocardiogram

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
30
A 62-year-old woman comes to the office for follow-up on hypertension. She has no history of heart disease or stroke and currently takes no medications. The patient has a sedentary lifestyle, is a lifetime nonsmoker, and drinks 2 or 3 glasses of wine each evening. She typically salts her food before tasting it; her diet is high in snacks, processed meats, and saturated fat, and low in fruits and vegetables.
Recent blood pressure readings are 145-155/88-95 mm Hg. BMI is 28 kg/m2.
Laboratory results are as follows:
 The patient previously had a "bad reaction to many different blood pressure pills" and would like to lower her blood pressure through healthier lifestyle habits rather than medication. Which of the following would most likely result in the greatest decrease in this patient's blood pressure?
The patient previously had a "bad reaction to many different blood pressure pills" and would like to lower her blood pressure through healthier lifestyle habits rather than medication. Which of the following would most likely result in the greatest decrease in this patient's blood pressure?
A)Increase dietary intake of flavonoids
B)Initiate a low-carbohydrate diet
C)Initiate a regular aerobic exercise program
D)Initiate the low-sodium Dietary Approaches to Stop Hypertension (DASH) diet
E)Reduce alcohol intake to maximum of 1 beverage a day
Recent blood pressure readings are 145-155/88-95 mm Hg. BMI is 28 kg/m2.
Laboratory results are as follows:
 The patient previously had a "bad reaction to many different blood pressure pills" and would like to lower her blood pressure through healthier lifestyle habits rather than medication. Which of the following would most likely result in the greatest decrease in this patient's blood pressure?
The patient previously had a "bad reaction to many different blood pressure pills" and would like to lower her blood pressure through healthier lifestyle habits rather than medication. Which of the following would most likely result in the greatest decrease in this patient's blood pressure?A)Increase dietary intake of flavonoids
B)Initiate a low-carbohydrate diet
C)Initiate a regular aerobic exercise program
D)Initiate the low-sodium Dietary Approaches to Stop Hypertension (DASH) diet
E)Reduce alcohol intake to maximum of 1 beverage a day

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
31
A 46-year-old woman comes to the office due to frequent episodes of "choking" at night for the past 3 months. She wakes up in the middle of the night and is unable to "catch her breath." The symptoms subside slowly after she gets up and walks around. She has also experienced occasional palpitations. The patient is otherwise physically active and walks on a treadmill 5 times a week for 30-45 minutes. Other medical problems include rheumatic fever at age 12, hypertension, depression, fibromyalgia, and non-Hodgkin lymphoma treated with combination chemotherapy 10 years ago. She is a lifelong nonsmoker.
Temperature is 37.2 C (99 F), blood pressure is 122/80 mm Hg, pulse is 92/min, and respirations are 14/min. The lungs are clear to auscultation. Cardiac examination reveals a loud S1 and a "snapping" sound shortly after S2. There is a 2/6 ejection-type systolic murmur best heard over the second right intercostal space. There is also a faint mid-diastolic murmur heard over the cardiac apex. The remainder of the physical examination is unremarkable.
A transthoracic echocardiogram shows normal left ventricular size and function with an ejection fraction of 60%. The left atrium is moderately dilated. The mitral valve leaflets appear thickened with restricted opening. The estimated mitral valve area is 1.8 cm2 (normal: 4-6 cm2), consistent with moderate mitral stenosis. The aortic valve is sclerotic with mild restriction of leaflet motion and there is evidence of mild aortic stenosis. The pulmonary artery systolic pressure appears to be normal. ECG is shown in the exhibit.
Which of the following is the best next step in evaluating this patient's current symptoms?
A)Cardiac event monitor
B)CT scan of the chest
C)Exercise stress test
D)Split-night sleep study
E)Transesophageal echocardiogram
Temperature is 37.2 C (99 F), blood pressure is 122/80 mm Hg, pulse is 92/min, and respirations are 14/min. The lungs are clear to auscultation. Cardiac examination reveals a loud S1 and a "snapping" sound shortly after S2. There is a 2/6 ejection-type systolic murmur best heard over the second right intercostal space. There is also a faint mid-diastolic murmur heard over the cardiac apex. The remainder of the physical examination is unremarkable.
A transthoracic echocardiogram shows normal left ventricular size and function with an ejection fraction of 60%. The left atrium is moderately dilated. The mitral valve leaflets appear thickened with restricted opening. The estimated mitral valve area is 1.8 cm2 (normal: 4-6 cm2), consistent with moderate mitral stenosis. The aortic valve is sclerotic with mild restriction of leaflet motion and there is evidence of mild aortic stenosis. The pulmonary artery systolic pressure appears to be normal. ECG is shown in the exhibit.
Which of the following is the best next step in evaluating this patient's current symptoms?
A)Cardiac event monitor
B)CT scan of the chest
C)Exercise stress test
D)Split-night sleep study
E)Transesophageal echocardiogram

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
32
A 57-year-old man comes to the office after a recent hospitalization. Two weeks ago, he went to the emergency department due to chest pressure and was diagnosed with an acute ST elevation myocardial infarction. Emergency coronary angiography revealed an occluded left anterior descending artery, which was opened with a stent. The patient did well after the procedure and remained in the hospital for 2 days.
Since leaving the hospital, he has had no further chest discomfort. The patient notes dyspnea on exertion, and his current exercise tolerance is limited to walking 2 blocks on a flat surface. Other medical issues include hypertension, hyperlipidemia, and type 2 diabetes mellitus. Current medications include carvedilol, sacubitril-valsartan, aspirin, ticagrelor, atorvastatin, dapagliflozin, and furosemide.
Temperature is 36.7 C (98 F), blood pressure is 125/70 mm Hg, and pulse is 88/min. BMI is 33 kg/m2. The patient is in no acute distress. Estimated jugular venous pressure is 12 cm H2O. There is a 2/6 holosystolic apical murmur that radiates to the axilla. Crackles are heard at the right lung base that clear with deep inspiration. There is 1+ pitting lower extremity edema bilaterally to the mid-shin.
Laboratory results are as follows:
 ECG shows normal sinus rhythm. There are Q waves in the anterior precordial leads with a QRS complex duration of 80 msec. Echocardiography performed prior to discharge showed hypokinesis of the anterior and anterolateral walls, moderate mitral regurgitation, and a left ventricular ejection fraction of 30%.
ECG shows normal sinus rhythm. There are Q waves in the anterior precordial leads with a QRS complex duration of 80 msec. Echocardiography performed prior to discharge showed hypokinesis of the anterior and anterolateral walls, moderate mitral regurgitation, and a left ventricular ejection fraction of 30%.
Which of the following would be the most appropriate next step in the management of this patient?
A)Add amlodipine
B)Add an aldosterone antagonist
C)Add hydralazine
D)Refer for implantable cardioverter-defibrillator placement
E)Refer for mitral valve repair
Since leaving the hospital, he has had no further chest discomfort. The patient notes dyspnea on exertion, and his current exercise tolerance is limited to walking 2 blocks on a flat surface. Other medical issues include hypertension, hyperlipidemia, and type 2 diabetes mellitus. Current medications include carvedilol, sacubitril-valsartan, aspirin, ticagrelor, atorvastatin, dapagliflozin, and furosemide.
Temperature is 36.7 C (98 F), blood pressure is 125/70 mm Hg, and pulse is 88/min. BMI is 33 kg/m2. The patient is in no acute distress. Estimated jugular venous pressure is 12 cm H2O. There is a 2/6 holosystolic apical murmur that radiates to the axilla. Crackles are heard at the right lung base that clear with deep inspiration. There is 1+ pitting lower extremity edema bilaterally to the mid-shin.
Laboratory results are as follows:
 ECG shows normal sinus rhythm. There are Q waves in the anterior precordial leads with a QRS complex duration of 80 msec. Echocardiography performed prior to discharge showed hypokinesis of the anterior and anterolateral walls, moderate mitral regurgitation, and a left ventricular ejection fraction of 30%.
ECG shows normal sinus rhythm. There are Q waves in the anterior precordial leads with a QRS complex duration of 80 msec. Echocardiography performed prior to discharge showed hypokinesis of the anterior and anterolateral walls, moderate mitral regurgitation, and a left ventricular ejection fraction of 30%.Which of the following would be the most appropriate next step in the management of this patient?
A)Add amlodipine
B)Add an aldosterone antagonist
C)Add hydralazine
D)Refer for implantable cardioverter-defibrillator placement
E)Refer for mitral valve repair

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
33
A 20-year-old man comes to the office for a sports physical. The patient has played varsity basketball since high school. He has had no chest pain, shortness of breath, palpitations, or fainting spells. He has no medical history and takes no medications. There is no family history of sudden death.
Blood pressure is 115/75 mm Hg, pulse is 56/min, and BMI is 22 kg/m2. The patient is in no distress. The apical precordial impulse is hyperdynamic. There is a normal S1 and S2, and an S4 is heard. He has a 2/6 systolic murmur at the left sternal border that increases with Valsalva maneuver. The lungs are clear to auscultation. The abdomen is soft and nondistended. Peripheral pulses demonstrate a rapid upstroke followed by a decline and secondary rise.
Transthoracic echocardiogram reveals interventricular septal thickness of 1.8 cm (normal: <1.1 cm) and posterior left ventricular wall thickness of 0.9 cm (normal: <1.1 cm). Left ventricular ejection fraction is 75%. At rest, there is no left ventricular outflow gradient; however, Valsalva maneuver generates a gradient of 30 mm Hg.
Which of the following is the most appropriate recommendation for this patient?
A)Alcohol septal ablation
B)Avoid high-intensity physical activity
C)Implantable cardioverter defibrillator
D)Metoprolol
E)Nifedipine
Blood pressure is 115/75 mm Hg, pulse is 56/min, and BMI is 22 kg/m2. The patient is in no distress. The apical precordial impulse is hyperdynamic. There is a normal S1 and S2, and an S4 is heard. He has a 2/6 systolic murmur at the left sternal border that increases with Valsalva maneuver. The lungs are clear to auscultation. The abdomen is soft and nondistended. Peripheral pulses demonstrate a rapid upstroke followed by a decline and secondary rise.
Transthoracic echocardiogram reveals interventricular septal thickness of 1.8 cm (normal: <1.1 cm) and posterior left ventricular wall thickness of 0.9 cm (normal: <1.1 cm). Left ventricular ejection fraction is 75%. At rest, there is no left ventricular outflow gradient; however, Valsalva maneuver generates a gradient of 30 mm Hg.
Which of the following is the most appropriate recommendation for this patient?
A)Alcohol septal ablation
B)Avoid high-intensity physical activity
C)Implantable cardioverter defibrillator
D)Metoprolol
E)Nifedipine

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
34
A 56-year-old man comes to the office due to a 3-month history of upper abdominal discomfort. CT scan of the abdomen reveals a cystic pancreatic lesion; an endoscopic ultrasound-guided biopsy is planned. Medical history is significant for hypertension, hyperlipidemia, and a bicuspid aortic valve that was diagnosed at age 24. The patient underwent an aortic valve replacement with a bileaflet mechanical aortic valve at age 44 due to symptomatic aortic regurgitation. He takes warfarin daily and attends regular follow-up visits at an anticoagulation clinic. He had an episode of epistaxis a year ago that required nasal packing for 2 days.
ECG is unremarkable. An echocardiogram 2 months ago showed normal left ventricular size and function with an ejection fraction of 60%. The mechanical aortic valve prosthesis had normal leaflet motion, and there was mild mitral and tricuspid regurgitation. The aortic root size was normal.
Which of the following is the best next step in management of this patient?
A)Continue current warfarin regimen and proceed with biopsy
B)Explore alternate options to diagnose this patient's disease
C)Stop warfarin, give subcutaneous vitamin K, then proceed with biopsy
D)Stop warfarin, start intravenous heparin when INR <1.5, then proceed with biopsy
E)Stop warfarin, then proceed with biopsy when INR <1.5
ECG is unremarkable. An echocardiogram 2 months ago showed normal left ventricular size and function with an ejection fraction of 60%. The mechanical aortic valve prosthesis had normal leaflet motion, and there was mild mitral and tricuspid regurgitation. The aortic root size was normal.
Which of the following is the best next step in management of this patient?
A)Continue current warfarin regimen and proceed with biopsy
B)Explore alternate options to diagnose this patient's disease
C)Stop warfarin, give subcutaneous vitamin K, then proceed with biopsy
D)Stop warfarin, start intravenous heparin when INR <1.5, then proceed with biopsy
E)Stop warfarin, then proceed with biopsy when INR <1.5

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
35
A 58-year-old woman comes to the physician because of a two-week history of malaise, low-grade fevers, and poor appetite. She was hospitalized one month ago for a complicated urinary tract infection and underwent ureteroscopy due to a distal ureteral stone. Her other medical problems include hypertension, hepatitis C, and chronic lower back pain. Her current medications include hydrochlorothiazide and amlodipine.
Her temperature is 38.0 C (100.4 F), blood pressure is 120/70 mm Hg, pulse is 88/min, and respirations are 14/min. Physical examination reveals a soft, 2/6 decrescendo-type murmur at the left sternal border. A small petechial lesion is noted on her right big toe.
An EKG shows normal sinus rhythm. Transesophageal echocardiography (TEE) shows a 0.7 cm mobile mass attached to the non-coronary cusp of the aortic valve as well as mild-to-moderate aortic regurgitation. Blood cultures grow Enterococcus faecalis susceptible to ampicillin and gentamicin. Intravenous antibiotics are initiated.
On the fifth day of hospitalization, the patient still complains of malaise. Her temperature is 38.2 C (100.7 F). Physical examination shows a soft, 2/6 decrescendo-type murmur at the left sternal border, which is unchanged from admission. Repeat EKG is shown in this exhibit.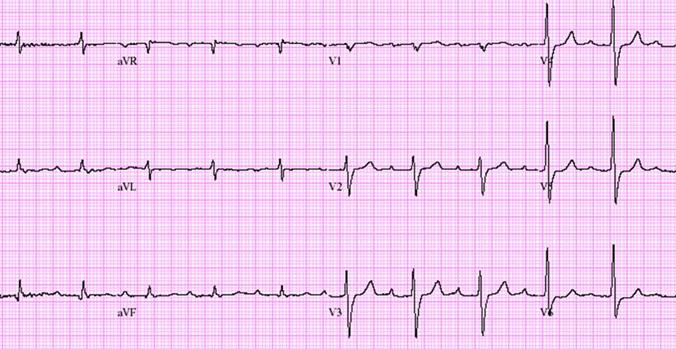
Which of the following is the most likely diagnosis?
A)Drug toxicity
B)Embolism to the coronary artery
C)Pericarditis
D)Perivalvular abscess
E)Sinus node dysfunction
Her temperature is 38.0 C (100.4 F), blood pressure is 120/70 mm Hg, pulse is 88/min, and respirations are 14/min. Physical examination reveals a soft, 2/6 decrescendo-type murmur at the left sternal border. A small petechial lesion is noted on her right big toe.
An EKG shows normal sinus rhythm. Transesophageal echocardiography (TEE) shows a 0.7 cm mobile mass attached to the non-coronary cusp of the aortic valve as well as mild-to-moderate aortic regurgitation. Blood cultures grow Enterococcus faecalis susceptible to ampicillin and gentamicin. Intravenous antibiotics are initiated.
On the fifth day of hospitalization, the patient still complains of malaise. Her temperature is 38.2 C (100.7 F). Physical examination shows a soft, 2/6 decrescendo-type murmur at the left sternal border, which is unchanged from admission. Repeat EKG is shown in this exhibit.
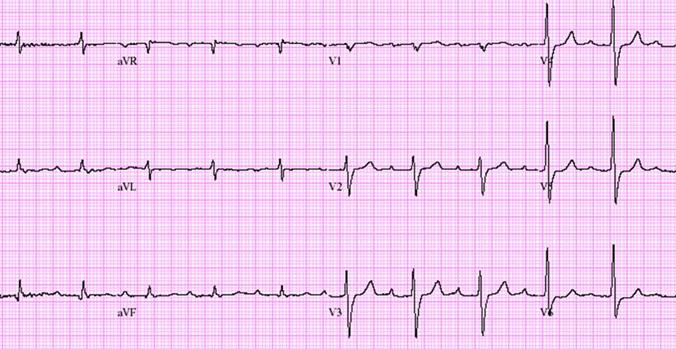
Which of the following is the most likely diagnosis?
A)Drug toxicity
B)Embolism to the coronary artery
C)Pericarditis
D)Perivalvular abscess
E)Sinus node dysfunction

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
36
A 67-year-old woman comes to the physician because of edema and shortness of breath. She reports that the edema has been present for approximately 3-4 months and involves her lower extremities. The shortness of breath occurs with minimal exertion and occasionally at rest. She denies chest pain or pressure, cough, and fever.
She has history of breast cancer diagnosed 12 years ago that was treated with mastectomy, chemotherapy, and chest wall radiation therapy. Her medications include aspirin, fish oil, and simvastatin.
Her blood pressure is 115/70 mm Hg, pulse is 62/min, and BMI is 27 kg/m2. The patient is in no acute distress. Her lungs are clear bilaterally. There is a normal S1 and S2 with a 2/6 apical murmur that radiates to the axilla. She has 3+ pitting edema below the knees bilaterally.
Her electrocardiogram is shown below.
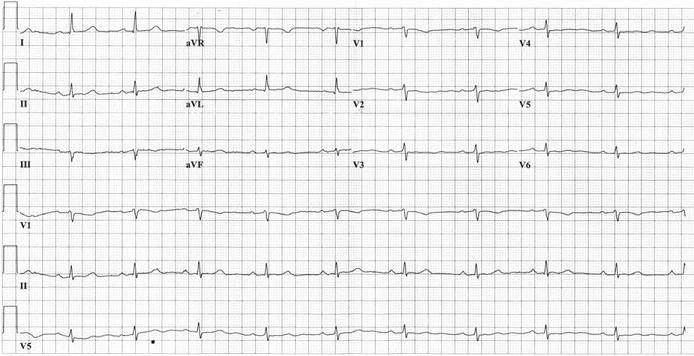
A transthoracic echocardiogram shows a normal left ventricular cavity size, a left ventricular ejection fraction of 70%, biatrial dilatation, severe left ventricular hypertrophy, and moderate mitral regurgitation.
Which of the following is the most likely additional finding in this patient?
A)Ascending aortic aneurysm
B)Carotid artery occlusion
C)Cavitary lung lesions
D)Hyperthyroidism
E)Significant proteinuria
She has history of breast cancer diagnosed 12 years ago that was treated with mastectomy, chemotherapy, and chest wall radiation therapy. Her medications include aspirin, fish oil, and simvastatin.
Her blood pressure is 115/70 mm Hg, pulse is 62/min, and BMI is 27 kg/m2. The patient is in no acute distress. Her lungs are clear bilaterally. There is a normal S1 and S2 with a 2/6 apical murmur that radiates to the axilla. She has 3+ pitting edema below the knees bilaterally.
Her electrocardiogram is shown below.
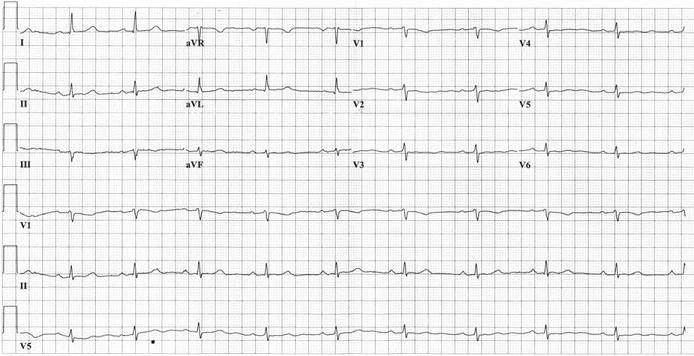
A transthoracic echocardiogram shows a normal left ventricular cavity size, a left ventricular ejection fraction of 70%, biatrial dilatation, severe left ventricular hypertrophy, and moderate mitral regurgitation.
Which of the following is the most likely additional finding in this patient?
A)Ascending aortic aneurysm
B)Carotid artery occlusion
C)Cavitary lung lesions
D)Hyperthyroidism
E)Significant proteinuria

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
37
A 44-year-old man comes to the physician because of muscle cramps and stiffness involving his legs over the last two weeks. He also describes fatigue and needs to rest after walking several blocks. His other medical problems include type 2 diabetes mellitus, hyperlipidemia, and migraine headaches. His medications include metformin, low-dose aspirin, glyburide, and simvastatin. He was recently started on daily verapamil for migraine prevention. He has a strong family history of diabetes and coronary artery disease.
His blood pressure is 123/70 mm Hg and his pulse is 70/min. His BMI is 31 kg/m2. There is no muscle tenderness on physical examination. Muscle strength is 5/5 bilaterally and deep tendon reflexes are 2+ and symmetrical bilaterally.
Laboratory results are as follows:
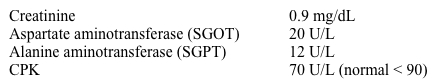
Which of the following is the most appropriate next step in managing this patient?
A)Antinuclear antibodies and ESR
B)Electromyography
C)Lactic acid level
D)Morning serum cortisol
E)Thyroid function tests
His blood pressure is 123/70 mm Hg and his pulse is 70/min. His BMI is 31 kg/m2. There is no muscle tenderness on physical examination. Muscle strength is 5/5 bilaterally and deep tendon reflexes are 2+ and symmetrical bilaterally.
Laboratory results are as follows:
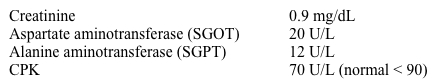
Which of the following is the most appropriate next step in managing this patient?
A)Antinuclear antibodies and ESR
B)Electromyography
C)Lactic acid level
D)Morning serum cortisol
E)Thyroid function tests

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
38
A 77-year-old woman comes to the physician because she "passed out." She says that over the last few months she has had several episodes where she feels very lightheaded and must sit down. On one occasion, she did actually lose consciousness and hit her head against a bathroom counter. There are no clear precipitants of these episodes. She denies chest pain or pressure. She thinks that she is more short of breath while playing tennis than she used to be in the past. Her other medical problems include hypertension and mild chronic kidney disease. Her medications include amlodipine, lisinopril, simvastatin, and aspirin.
Her blood pressure is 115/70 mm Hg, pulse is 62/min, and BMI is 23 kg/m2. The patient is in no acute distress. There is a normal S1 and a soft S2. There is a III/VI mid-peaking systolic ejection murmur at the right upper sternal border that radiates to both carotid arteries. Her lungs are clear to auscultation. Her abdomen is soft and non-distended. Peripheral pulses are 2+ and symmetric.
An echocardiogram showed normal left ventricular function, mild left ventricular hypertrophy, and moderate calcific aortic stenosis with an estimated aortic valve area of 1.4 cm2 (normal 3-4 cm2).
The patient was given a 24-hour Holter monitor. The tracing below was recorded at 1:25 pm.
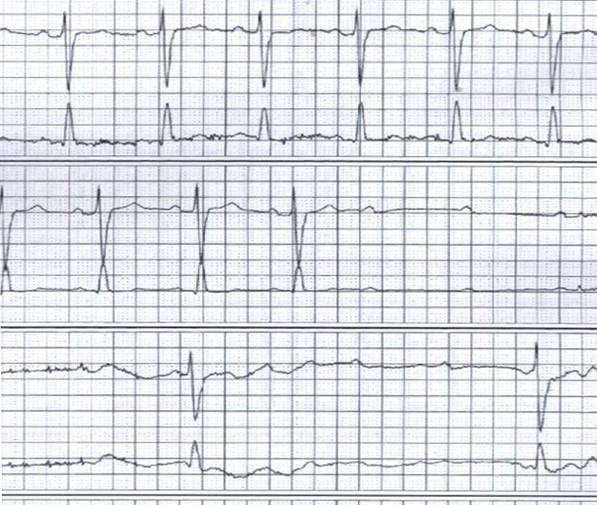
Which of the following would be the best next step in managing this patient?
A)Aortic valve replacement
B)Discontinuation of amlodipine with close follow-up
C)Exercise stress testing
D)Permanent pacemaker placement
E)Tilt table testing
Her blood pressure is 115/70 mm Hg, pulse is 62/min, and BMI is 23 kg/m2. The patient is in no acute distress. There is a normal S1 and a soft S2. There is a III/VI mid-peaking systolic ejection murmur at the right upper sternal border that radiates to both carotid arteries. Her lungs are clear to auscultation. Her abdomen is soft and non-distended. Peripheral pulses are 2+ and symmetric.
An echocardiogram showed normal left ventricular function, mild left ventricular hypertrophy, and moderate calcific aortic stenosis with an estimated aortic valve area of 1.4 cm2 (normal 3-4 cm2).
The patient was given a 24-hour Holter monitor. The tracing below was recorded at 1:25 pm.
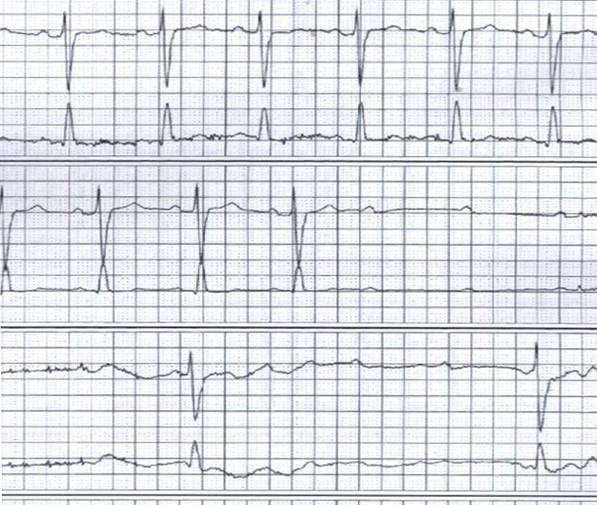
Which of the following would be the best next step in managing this patient?
A)Aortic valve replacement
B)Discontinuation of amlodipine with close follow-up
C)Exercise stress testing
D)Permanent pacemaker placement
E)Tilt table testing

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
39
A 63-year-old woman is admitted to the hospital for sudden-onset shortness of breath and chest heaviness that began 2 hours ago. She had a similar episode of shortness of breath with hypertensive urgency 8 months ago. An echocardiogram at that time showed left ventricular hypertrophy, modest diastolic dysfunction, and an ejection fraction of 60%. Stress testing showed no evidence of ischemia. The patient's medical problems include a 5-year history of intermittent claudication, hypertension, hyperlipidemia, and type 2 diabetes mellitus. She is a former smoker with a 35-pack-year history. She works as an accountant and admits to feeling stressed at work.
Blood pressure is 210/100 mm Hg, pulse is 110/min, and respirations are 20/min. BMI is 34 kg/m2. Pulses are equal in all 4 extremities. She appears dyspneic. Jugular venous pressure is normal. There are bibasilar lung crackles and a prolonged expiratory phase of respiration.
ECG shows sinus tachycardia, left ventricular hypertrophy, and nonspecific T-wave abnormalities. Chest x-ray reveals pulmonary edema. The patient is treated with intravenous furosemide, antihypertensive agents, and noninvasive positive-pressure ventilation.
Four hours later, her symptoms resolve and she appears comfortable. Blood pressure is 144/89 mm Hg and pulse is 75/min.
Laboratory results are as follows:
 Urinalysis shows 1+ protein.
Urinalysis shows 1+ protein.
This patient should be evaluated for which of the following conditions?
A)Adrenal cortisol-producing tumor
B)Bilateral renal artery stenosis
C)Coarctation of the aorta
D)Hashimoto thyroiditis
E)Intracranial carotid artery stenosis
Blood pressure is 210/100 mm Hg, pulse is 110/min, and respirations are 20/min. BMI is 34 kg/m2. Pulses are equal in all 4 extremities. She appears dyspneic. Jugular venous pressure is normal. There are bibasilar lung crackles and a prolonged expiratory phase of respiration.
ECG shows sinus tachycardia, left ventricular hypertrophy, and nonspecific T-wave abnormalities. Chest x-ray reveals pulmonary edema. The patient is treated with intravenous furosemide, antihypertensive agents, and noninvasive positive-pressure ventilation.
Four hours later, her symptoms resolve and she appears comfortable. Blood pressure is 144/89 mm Hg and pulse is 75/min.
Laboratory results are as follows:
 Urinalysis shows 1+ protein.
Urinalysis shows 1+ protein.This patient should be evaluated for which of the following conditions?
A)Adrenal cortisol-producing tumor
B)Bilateral renal artery stenosis
C)Coarctation of the aorta
D)Hashimoto thyroiditis
E)Intracranial carotid artery stenosis

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
40
A 32-year-old paramedic comes to the office for a routine health maintenance examination. He has had headaches for the past several months as well as episodes of nosebleeds. He has no other medical problems. The patient does not use tobacco or illicit drugs but drinks 1 or 2 cans of beer daily. He has no family history of heart failure or sudden death.
Temperature is 36.1 C (97 F); blood pressure is 188/96 mm Hg in the right arm, 184/94 mm Hg in the left arm, and 114/76 mm Hg in the right leg; pulse is 68/min, and respirations are 14/min. Height is 180 cm (5 ft 11 in). Examination reveals no audible carotid bruits. There is a 2/6 mid-systolic murmur heard at the left sternal border as well as a continuous "rumbling" sound heard in the back over the interscapular area.
Diagnostic testing is most likely to demonstrate which of the following findings?
A)Atrial septal defect
B)Bicuspid aortic valve
C)Pulmonic stenosis
D)Right ventricular dysplasia
E)Wolff-Parkinson-White syndrome
Temperature is 36.1 C (97 F); blood pressure is 188/96 mm Hg in the right arm, 184/94 mm Hg in the left arm, and 114/76 mm Hg in the right leg; pulse is 68/min, and respirations are 14/min. Height is 180 cm (5 ft 11 in). Examination reveals no audible carotid bruits. There is a 2/6 mid-systolic murmur heard at the left sternal border as well as a continuous "rumbling" sound heard in the back over the interscapular area.
Diagnostic testing is most likely to demonstrate which of the following findings?
A)Atrial septal defect
B)Bicuspid aortic valve
C)Pulmonic stenosis
D)Right ventricular dysplasia
E)Wolff-Parkinson-White syndrome

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
41
A 22-year-old man comes to the office due to 6 months of exertional shortness of breath. He describes himself as nonathletic and has never engaged in competitive sports. The patient has recently experienced dyspnea on moderate exertion. He also describes a pounding sensation in his head at night. He does not use tobacco, alcohol, or illicit drugs.
Blood pressure is 150/65 mm Hg and pulse is 90/min. No jugular venous distension is present. There is no digital clubbing or cyanosis. The apical impulse is brisk and displaced to the left. A 2/6 continuous murmur is heard below the left clavicle. Upper and lower extremity pulses are prominent and equal. The lungs are clear on auscultation.
If untreated, this patient's risk for which of the following is most increased?
A)Aortic dissection
B)Constrictive pericarditis
C)Infective endarteritis
D)Intracranial aneurysm
E)Mitral stenosis
Blood pressure is 150/65 mm Hg and pulse is 90/min. No jugular venous distension is present. There is no digital clubbing or cyanosis. The apical impulse is brisk and displaced to the left. A 2/6 continuous murmur is heard below the left clavicle. Upper and lower extremity pulses are prominent and equal. The lungs are clear on auscultation.
If untreated, this patient's risk for which of the following is most increased?
A)Aortic dissection
B)Constrictive pericarditis
C)Infective endarteritis
D)Intracranial aneurysm
E)Mitral stenosis

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
42
A 76-year-old woman comes to the office for preoperative evaluation. She has had worsening pain in her left knee with occasional swelling over the past several months. Her daughter has had to assist with household chores because the patient has difficulty using the stairs due to pain. Two weeks earlier she was seen by an orthopedic surgeon who recommended knee replacement surgery. The patient has no chest pain, although she admits she is not very active due to the knee pain. She also has no palpitations or shortness of breath while lying flat. Her other medical problems include obesity, hypertension, type 2 diabetes mellitus, obstructive sleep apnea, and history of peptic ulcer disease. Current medications include metformin, atorvastatin, and lisinopril. The patient monitors her blood glucose at home, with values around 110 mg/dL. She had a femoral hernia surgery 12 years ago without complications.
Blood pressure is 132/76 mm Hg and pulse is 72/min. BMI is 33.1 kg/m2. Examination shows normal jugular venous distension and no carotid bruits. Heart sounds are normal and the lungs are clear to auscultation.
Hemoglobin is 12.2 g/dL, creatinine is 0.7 mg/dL, and potassium is 4.3 mEq/L. ECG shows normal sinus rhythm with T-wave inversion in lead III.
Which of the following is the most appropriate next step before surgery?
A)Coagulation profile
B)Dipyridamole myocardial perfusion imaging
C)Exercise stress test
D)No further testing
E)Transthoracic echocardiogram
Blood pressure is 132/76 mm Hg and pulse is 72/min. BMI is 33.1 kg/m2. Examination shows normal jugular venous distension and no carotid bruits. Heart sounds are normal and the lungs are clear to auscultation.
Hemoglobin is 12.2 g/dL, creatinine is 0.7 mg/dL, and potassium is 4.3 mEq/L. ECG shows normal sinus rhythm with T-wave inversion in lead III.
Which of the following is the most appropriate next step before surgery?
A)Coagulation profile
B)Dipyridamole myocardial perfusion imaging
C)Exercise stress test
D)No further testing
E)Transthoracic echocardiogram

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
43
A 68-year-old man comes to the physician because of lower extremity edema. His edema has been present for the last six months, but it has worsened lately. He denies chest pain or pressure, although he reports some exertional shortness of breath and a dry cough that occurs mostly at night. He denies any recent change in diet or medications. His other medical problems include chronic obstructive pulmonary disease and hyperlipidemia. His current medications include albuterol/ipratropium inhaler, simvastatin, and aspirin. He has smoked 1 pack of cigarettes per day for the last 48 years, but he denies alcohol or illicit drug use.
His blood pressure is 140/75 mm Hg in both arms, pulse is 60/min, and respirations are 14/min. He is in no acute distress. His jugular veins are distended with the peak of the 'a' wave poorly visualized at 90 degrees. There is a sustained parasternal lift best felt at the left lower parasternal border. There is a normal S1 with a loud S2. There is a holosystolic murmur best heard at the left sternal border that increases with inspiration. The lungs are clear bilaterally. The liver is slightly enlarged. There is 2+ pitting edema to the thighs bilaterally.
A 12 lead ECG is shown in this exhibit.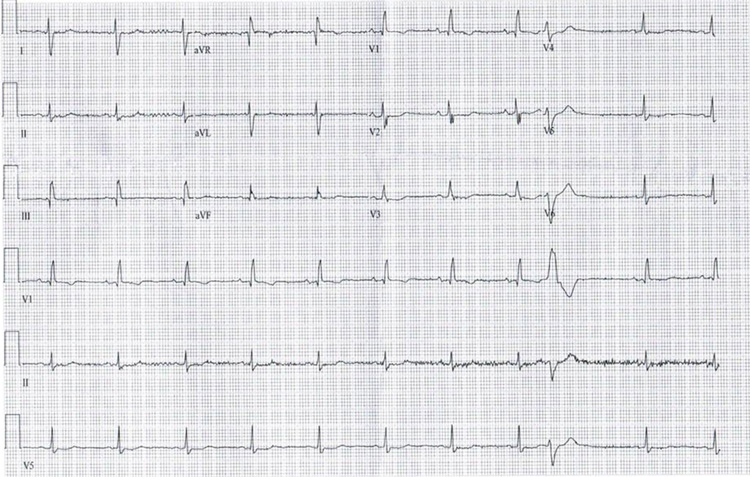
Which of the following will most likely be seen on echocardiography?
A)Aortic stenosis
B)Asymmetric septal hypertrophy
C)Left ventricular aneurysm
D)Pericardial effusion
E)Right ventricular dilatation
His blood pressure is 140/75 mm Hg in both arms, pulse is 60/min, and respirations are 14/min. He is in no acute distress. His jugular veins are distended with the peak of the 'a' wave poorly visualized at 90 degrees. There is a sustained parasternal lift best felt at the left lower parasternal border. There is a normal S1 with a loud S2. There is a holosystolic murmur best heard at the left sternal border that increases with inspiration. The lungs are clear bilaterally. The liver is slightly enlarged. There is 2+ pitting edema to the thighs bilaterally.
A 12 lead ECG is shown in this exhibit.
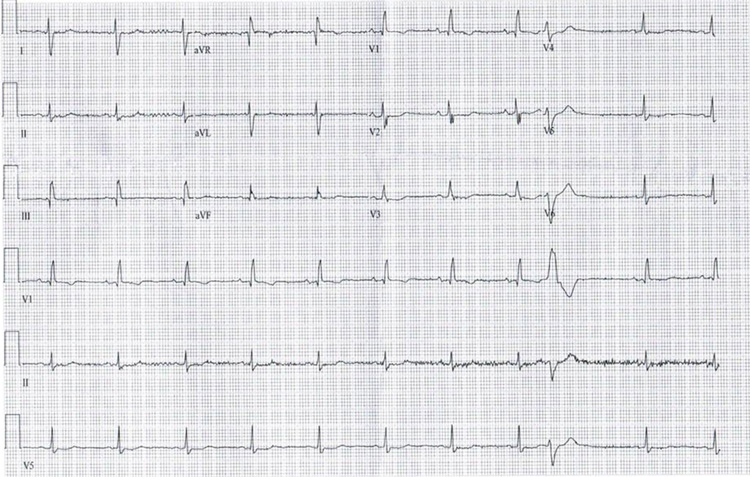
Which of the following will most likely be seen on echocardiography?
A)Aortic stenosis
B)Asymmetric septal hypertrophy
C)Left ventricular aneurysm
D)Pericardial effusion
E)Right ventricular dilatation

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
44
A 42-year-old man comes to the office due to fatigue and shortness of breath. His symptoms began 6 months ago with decreased exercise tolerance during his typical morning jog. Since then, his fatigue has gradually progressed and he has also had occasional palpitations, which he describes as his "heart races fast." The patient reports a weight gain of 5 kg (11 lb) over the last month and has had shortness of breath with mild exertion and leg swelling for the past 2 weeks. The patient does not remember any recent viral illness and has no prior medical conditions. He takes no medications, is a lifelong nonsmoker, and drinks alcohol occasionally. Family history is unremarkable.
Temperature is 37.2 C (99 F), blood pressure is 122/80 mm Hg, pulse is 135/min and irregular, and respirations are 18/min. Jugular venous pressure is 12 cm H2O. Lung examination reveals decreased breath sounds at the bases with occasional bibasilar crackles. Cardiac examination reveals a 2/6 holosystolic murmur best heard at the apex. There is 2+ bilateral lower extremity pitting edema.
Blood cell counts, serum chemistry, and TSH are within normal limits. ECG is shown in the exhibit.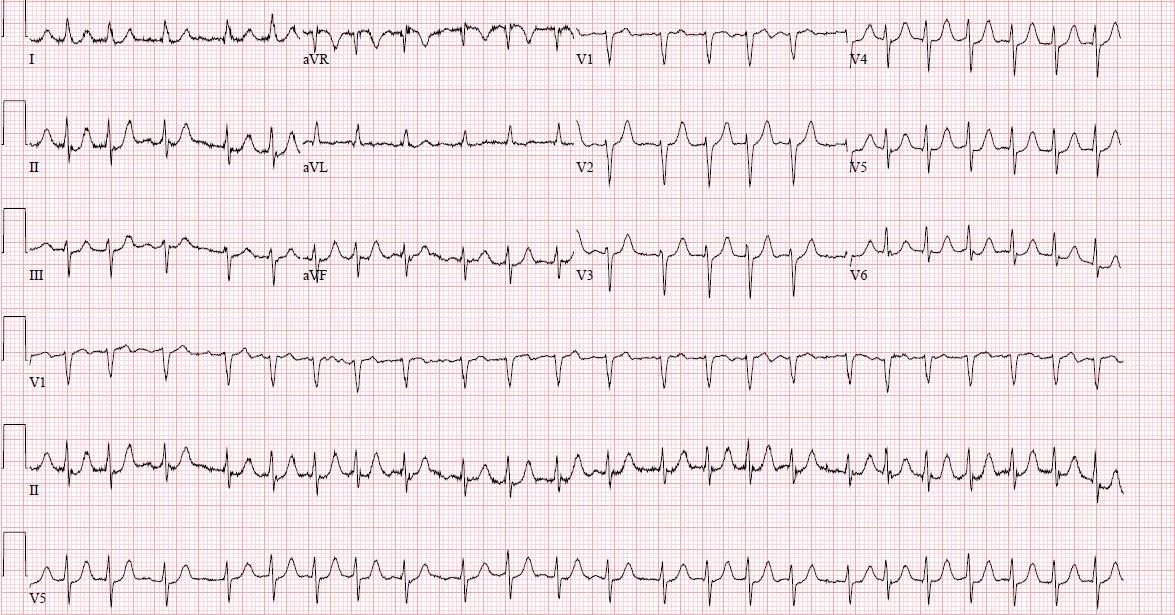 Echocardiography shows a dilated and diffusely hypokinetic left ventricle with an ejection fraction of 25%. The right ventricle is mildly hypokinetic. The left atrium is mildly dilated. There is a central jet of moderate mitral regurgitation.
Echocardiography shows a dilated and diffusely hypokinetic left ventricle with an ejection fraction of 25%. The right ventricle is mildly hypokinetic. The left atrium is mildly dilated. There is a central jet of moderate mitral regurgitation.
Which of the following is most likely to provide the greatest long-term improvement in this patient's left ventricular function?
A)Afterload reduction
B)Coronary artery revascularization
C)Diuresis and fluid optimization
D)Heart rate control
E)Mitral valve surgery
Temperature is 37.2 C (99 F), blood pressure is 122/80 mm Hg, pulse is 135/min and irregular, and respirations are 18/min. Jugular venous pressure is 12 cm H2O. Lung examination reveals decreased breath sounds at the bases with occasional bibasilar crackles. Cardiac examination reveals a 2/6 holosystolic murmur best heard at the apex. There is 2+ bilateral lower extremity pitting edema.
Blood cell counts, serum chemistry, and TSH are within normal limits. ECG is shown in the exhibit.
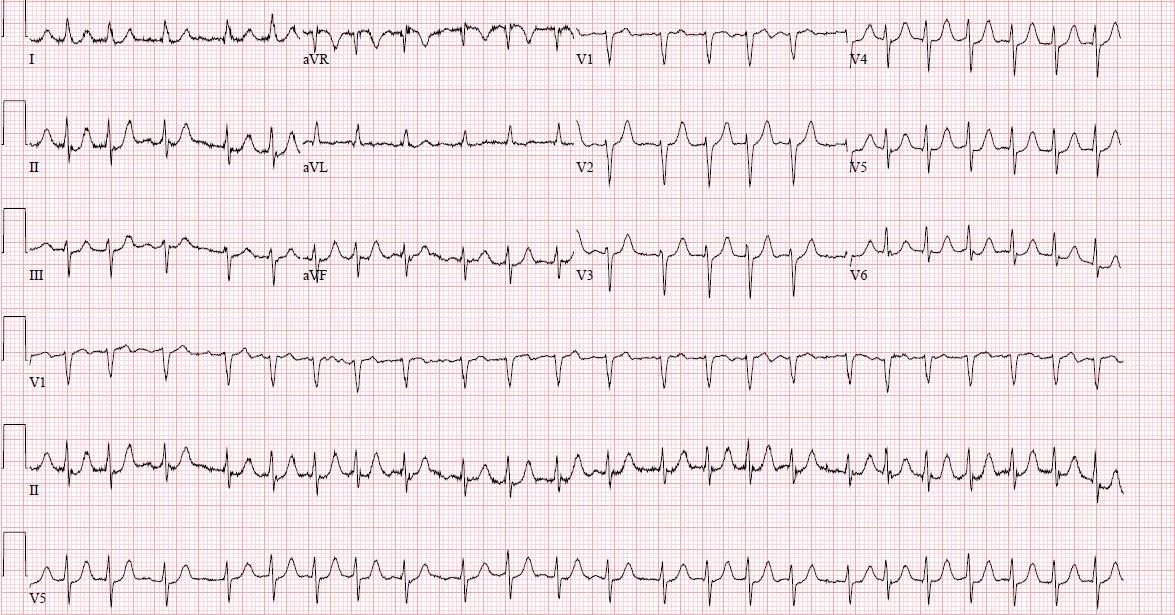 Echocardiography shows a dilated and diffusely hypokinetic left ventricle with an ejection fraction of 25%. The right ventricle is mildly hypokinetic. The left atrium is mildly dilated. There is a central jet of moderate mitral regurgitation.
Echocardiography shows a dilated and diffusely hypokinetic left ventricle with an ejection fraction of 25%. The right ventricle is mildly hypokinetic. The left atrium is mildly dilated. There is a central jet of moderate mitral regurgitation.Which of the following is most likely to provide the greatest long-term improvement in this patient's left ventricular function?
A)Afterload reduction
B)Coronary artery revascularization
C)Diuresis and fluid optimization
D)Heart rate control
E)Mitral valve surgery

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
45
A 29-year-old woman comes to the physician accompanied by her husband for an initial consultation. She has no current symptoms. She is physically active and walks for 45 minutes on a treadmill 3-4 days a week. She has a past history of "heart failure," which was diagnosed 1 week after the birth of her first child 2 years ago.
She was found to have a reduced LV ejection fraction of 25%, but further evaluation did not reveal any specific cause of her cardiomyopathy. She has been taking daily furosemide, potassium supplements, carvedilol, and quinapril since that time. Her last echocardiogram 2 months ago showed an improved LV ejection fraction of 40%, mild left atrial enlargement, and mild mitral regurgitation. The couple is contemplating another pregnancy and was referred by the obstetrician for a second opinion.
Which of the following is the most appropriate recommendation?
A)Advise avoiding pregnancy
B)Continue current medications throughout pregnancy
C)Discontinue carvedilol and quinapril
D)Discontinue quinapril and continue carvedilol
E)Discontinue quinapril and start digoxin
She was found to have a reduced LV ejection fraction of 25%, but further evaluation did not reveal any specific cause of her cardiomyopathy. She has been taking daily furosemide, potassium supplements, carvedilol, and quinapril since that time. Her last echocardiogram 2 months ago showed an improved LV ejection fraction of 40%, mild left atrial enlargement, and mild mitral regurgitation. The couple is contemplating another pregnancy and was referred by the obstetrician for a second opinion.
Which of the following is the most appropriate recommendation?
A)Advise avoiding pregnancy
B)Continue current medications throughout pregnancy
C)Discontinue carvedilol and quinapril
D)Discontinue quinapril and continue carvedilol
E)Discontinue quinapril and start digoxin

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
46
A 72-year-old man comes to the physician complaining of 2 weeks of muscle cramps and stiffness in his legs. He also feels fatigued and has to rest after walking several blocks. His past medical history is significant for coronary artery disease, type 2 diabetes mellitus, paroxysmal atrial fibrillation, and hyperlipidemia.
The patient underwent coronary revascularization with placement of 2 drug-eluting stents in his left anterior descending artery 6 months ago. His medications include metformin, low-dose-aspirin, clopidogrel, metoprolol, valsartan, and atorvastatin. He was recently started on amiodarone due to recurrent episodes of highly symptomatic atrial fibrillation.
The patient's blood pressure is 129/72 mm Hg and pulse is 65/min. His body mass index is 30 kg/m2. There is no muscle tenderness on physical examination. His muscle strength is 5/5 bilaterally and deep-tendon reflexes are 2+ and symmetrical bilaterally.
Laboratory results are as follows:
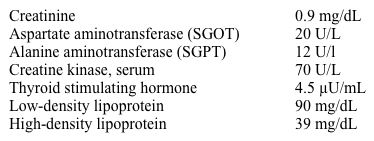
His atorvastatin is discontinued and his symptoms resolve completely within 4 weeks.
Which of the following is the best next step in management of this patient?
A)Avoid lipid-lowering therapy
B)Resume atorvastatin at a lower dose
C)Start ezetimibe
D)Start gemfibrozil
E)Start rosuvastatin
The patient underwent coronary revascularization with placement of 2 drug-eluting stents in his left anterior descending artery 6 months ago. His medications include metformin, low-dose-aspirin, clopidogrel, metoprolol, valsartan, and atorvastatin. He was recently started on amiodarone due to recurrent episodes of highly symptomatic atrial fibrillation.
The patient's blood pressure is 129/72 mm Hg and pulse is 65/min. His body mass index is 30 kg/m2. There is no muscle tenderness on physical examination. His muscle strength is 5/5 bilaterally and deep-tendon reflexes are 2+ and symmetrical bilaterally.
Laboratory results are as follows:
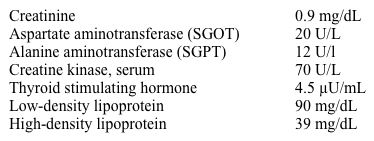
His atorvastatin is discontinued and his symptoms resolve completely within 4 weeks.
Which of the following is the best next step in management of this patient?
A)Avoid lipid-lowering therapy
B)Resume atorvastatin at a lower dose
C)Start ezetimibe
D)Start gemfibrozil
E)Start rosuvastatin

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
47
A 76-year-old man comes to the office for a preoperative evaluation. The patient is scheduled for an elective prostatectomy in 2 weeks. He initially had difficulty urinating and was found to have an enlarged, irregular prostate; subsequent evaluation revealed adenocarcinoma of the prostate. Medical history is notable for hypertension and diet-controlled diabetes mellitus. The patient also had a stroke 6 years ago and has residual right upper extremity weakness. Medications include daily low-dose aspirin, atorvastatin, valsartan, tamsulosin, and finasteride. He walks 2 miles most days and smokes half a pack of cigarettes daily.
Physical examination is normal except for mild weakness in the right upper extremity.
ECG shows normal sinus rhythm at 74/min with occasional premature atrial beats. Hemoglobin is 14.1 g/dL, platelet count is 340,000/mm3, and creatinine is 0.8 mg/dL.
Which of the following is the most appropriate next step in management of this patient?
A)Obtain pharmacologic radionuclide stress testing
B)Order exercise stress testing
C)Recommend proceeding with surgery without additional intervention
D)Start high-dose metoprolol 7 days prior to surgery
E)Start low-dose metoprolol the day of surgery
Physical examination is normal except for mild weakness in the right upper extremity.
ECG shows normal sinus rhythm at 74/min with occasional premature atrial beats. Hemoglobin is 14.1 g/dL, platelet count is 340,000/mm3, and creatinine is 0.8 mg/dL.
Which of the following is the most appropriate next step in management of this patient?
A)Obtain pharmacologic radionuclide stress testing
B)Order exercise stress testing
C)Recommend proceeding with surgery without additional intervention
D)Start high-dose metoprolol 7 days prior to surgery
E)Start low-dose metoprolol the day of surgery

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
48
A 54-year-old man comes to the physician with fatigue and decreased exercise tolerance over the last 6 months. He denies cough, chest pain, syncope, or weight loss. He had aortic valve replacement with a mechanical valve due to bicuspid aortic valve stenosis 7 years ago. Coronary angiography prior to surgery showed no evidence of coronary artery disease. His medications include warfarin and antacids for occasional heartburn.
His blood pressure is 122/70 mm Hg and pulse is 89/min and regular. Jugular venous pressure is estimated at 9 cm H2O. A faint early diastolic murmur is heard at the left sternal border. Lungs are clear on auscultation. The liver span is 9 cm, and the tip of the spleen is not palpable. There is no edema of the lower extremities.
Laboratory results are as follows:
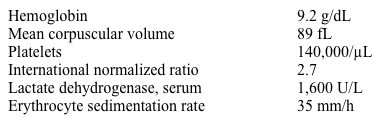
Which of the following is the most likely diagnosis?
A)Colonic angiodysplasia
B)Hemolytic anemia
C)Large-vessel vasculitis
D)Lymphoma
E)Staphylococcus aureus endocarditis
His blood pressure is 122/70 mm Hg and pulse is 89/min and regular. Jugular venous pressure is estimated at 9 cm H2O. A faint early diastolic murmur is heard at the left sternal border. Lungs are clear on auscultation. The liver span is 9 cm, and the tip of the spleen is not palpable. There is no edema of the lower extremities.
Laboratory results are as follows:
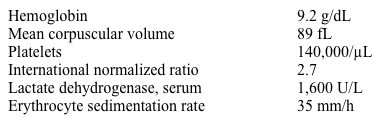
Which of the following is the most likely diagnosis?
A)Colonic angiodysplasia
B)Hemolytic anemia
C)Large-vessel vasculitis
D)Lymphoma
E)Staphylococcus aureus endocarditis

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
49
A 35-year-old woman comes to the physician for follow-up of hypertension. When the patient was seen in the office 2 weeks ago, her blood pressure was 145/95 mm Hg initially and 140/92 mm Hg after recheck. Since then, she had her blood pressure taken 3 times at a nearby pharmacy, with readings averaging 120/80 mm Hg. The patient has no symptoms and feels "pretty healthy." She takes no medications.
The patient's father has hypertension and coronary artery disease, which required coronary artery bypass grafting. Her mother has hypertension and type 2 diabetes mellitus. The patient regularly salts her food before tasting it. She drinks alcohol socially and does not use tobacco or illicit drugs. The patient works as an information technology consultant and exercises moderately 3 times a week.
Blood pressure during this visit is 149/94 mm Hg initially and 138/94 mm Hg after 20 minutes. BMI is 28 kg/m2. The ocular fundi appear normal. Physical examination is unremarkable.
A complete blood count, urinalysis, and comprehensive metabolic panel are normal. Serum creatinine is 0.9 mg/dL. ECG shows normal sinus rhythm and T-wave inversion in leads V1 and V2.
Which of the following is the best next step in management of this patient's blood pressure?
A)Evaluate for pheochromocytoma
B)Obtain echocardiogram to evaluate for left ventricular hypertrophy
C)Order 24-hour ambulatory blood pressure monitoring
D)Schedule repeat office blood pressure checks
E)Start low-dose thiazide diuretic
The patient's father has hypertension and coronary artery disease, which required coronary artery bypass grafting. Her mother has hypertension and type 2 diabetes mellitus. The patient regularly salts her food before tasting it. She drinks alcohol socially and does not use tobacco or illicit drugs. The patient works as an information technology consultant and exercises moderately 3 times a week.
Blood pressure during this visit is 149/94 mm Hg initially and 138/94 mm Hg after 20 minutes. BMI is 28 kg/m2. The ocular fundi appear normal. Physical examination is unremarkable.
A complete blood count, urinalysis, and comprehensive metabolic panel are normal. Serum creatinine is 0.9 mg/dL. ECG shows normal sinus rhythm and T-wave inversion in leads V1 and V2.
Which of the following is the best next step in management of this patient's blood pressure?
A)Evaluate for pheochromocytoma
B)Obtain echocardiogram to evaluate for left ventricular hypertrophy
C)Order 24-hour ambulatory blood pressure monitoring
D)Schedule repeat office blood pressure checks
E)Start low-dose thiazide diuretic

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
50
A 54-year-old woman comes to the office due to lower extremity swelling and discomfort over the past week. The patient says that she can no longer fit into her shoes. Otherwise, she feels fine and has no orthopnea, dyspnea on exertion, or chest pain. She was recently diagnosed with essential hypertension (systolic blood pressure 165-170 mm Hg and diastolic blood pressure 95-100 mm Hg) and was started on amlodipine. Complete blood count and chemistry panel were normal at that time.
The patient's current blood pressure is 156/95 mm Hg, pulse is 84/min, and respirations are 14/min. Pulse oximetry is 98% on room air. Her BMI is 28 kg/m2. Jugular venous pressure is estimated at 8 cm H2O. Lungs are clear to auscultation. There are no murmurs or additional heart sounds. The liver span is 10 cm and the spleen is not palpable. There is 2+ symmetric pitting edema involving her lower extremities.
Laboratory results are as follows:
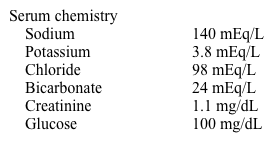
Which of the following therapies, if it had been initiated with amlodipine, could have most likely prevented this patient's current condition?
A)ACE inhibitor
B)Beta blocker
C)Digoxin
D)Hydralazine
E)Thiazide diuretic
The patient's current blood pressure is 156/95 mm Hg, pulse is 84/min, and respirations are 14/min. Pulse oximetry is 98% on room air. Her BMI is 28 kg/m2. Jugular venous pressure is estimated at 8 cm H2O. Lungs are clear to auscultation. There are no murmurs or additional heart sounds. The liver span is 10 cm and the spleen is not palpable. There is 2+ symmetric pitting edema involving her lower extremities.
Laboratory results are as follows:
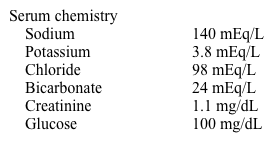
Which of the following therapies, if it had been initiated with amlodipine, could have most likely prevented this patient's current condition?
A)ACE inhibitor
B)Beta blocker
C)Digoxin
D)Hydralazine
E)Thiazide diuretic

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
51
A 35-year-old woman comes to the office as she missed her period 10 days ago and believes that she may be pregnant. She otherwise has regular monthly menstrual cycles. The patient moved to the United States from South Africa 6 months ago, and has a history of rheumatic heart disease. She had a "ministroke" 8 years ago and was found to be in atrial fibrillation at that time; she has since been on warfarin for anticoagulation. The patient took antibiotic prophylaxis for secondary prevention of rheumatic fever with intramuscular penicillin until age 30.
Temperature is 37.2 C (99 F), blood pressure is 122/82 mm Hg, pulse is 96/min, and respirations are 14/min. The lungs are clear to auscultation. Cardiac examination reveals irregular heart sounds, an accentuated S1, and a loud "snapping" sound shortly after S2. There is also a faint mid-diastolic murmur heard over the cardiac apex.
Urine pregnancy test is positive. ECG is shown in the exhibit.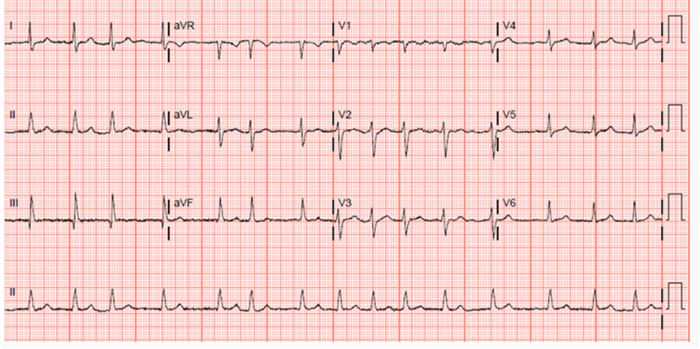
Which of the following is the best next step in management of this patient?
A)Continue warfarin with close INR monitoring throughout pregnancy
B)Stop warfarin and monitor closely throughout pregnancy
C)Stop warfarin and start daily dabigatran
D)Stop warfarin and start daily subcutaneous unfractionated heparin
E)Stop warfarin and start subcutaneous low-molecular-weight heparin
Temperature is 37.2 C (99 F), blood pressure is 122/82 mm Hg, pulse is 96/min, and respirations are 14/min. The lungs are clear to auscultation. Cardiac examination reveals irregular heart sounds, an accentuated S1, and a loud "snapping" sound shortly after S2. There is also a faint mid-diastolic murmur heard over the cardiac apex.
Urine pregnancy test is positive. ECG is shown in the exhibit.
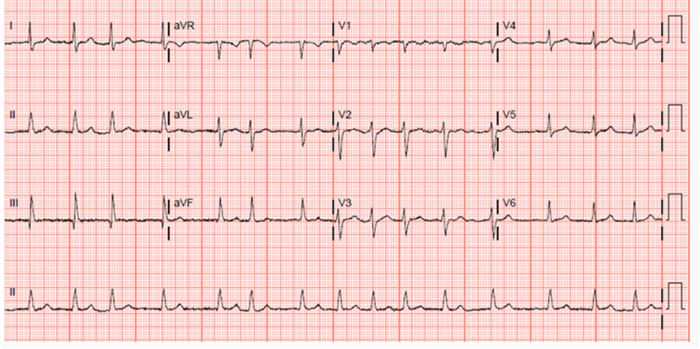
Which of the following is the best next step in management of this patient?
A)Continue warfarin with close INR monitoring throughout pregnancy
B)Stop warfarin and monitor closely throughout pregnancy
C)Stop warfarin and start daily dabigatran
D)Stop warfarin and start daily subcutaneous unfractionated heparin
E)Stop warfarin and start subcutaneous low-molecular-weight heparin

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
52
A 72-year-old man comes to the office 4 weeks following discharge from the hospital due to an episode of acute decompensated heart failure. The patient feels much better now but claims that he gets tired easily. He becomes short of breath after walking a few blocks on a level surface. He has a history of myocardial infarction, coronary artery bypass grafting, ischemic cardiomyopathy, hypertension, hyperlipidemia, and type 2 diabetes mellitus. The patient has had several hospital admissions for decompensated heart failure over the past 2 years. His home medications include aspirin, carvedilol, sacubitril-valsartan, atorvastatin, furosemide, and insulin.
Temperature is 37.2 C (99 F), blood pressure is 128/76 mm Hg, pulse is 76/min, and respirations are 16/min. Pulse oximetry is 94% on room air. The patient is in no apparent respiratory distress. Jugular venous pressure is measured at 8 cm H2O. Lung examination reveals clear lung fields with decreased breath sounds at the bases. Cardiac examination reveals normal S1 and S2 along with a 2/6 holosystolic murmur heard over the cardiac apex. There is minimal pitting edema around the ankles.
Laboratory results are as follows:
 ECG is shown in the exhibit.
ECG is shown in the exhibit. 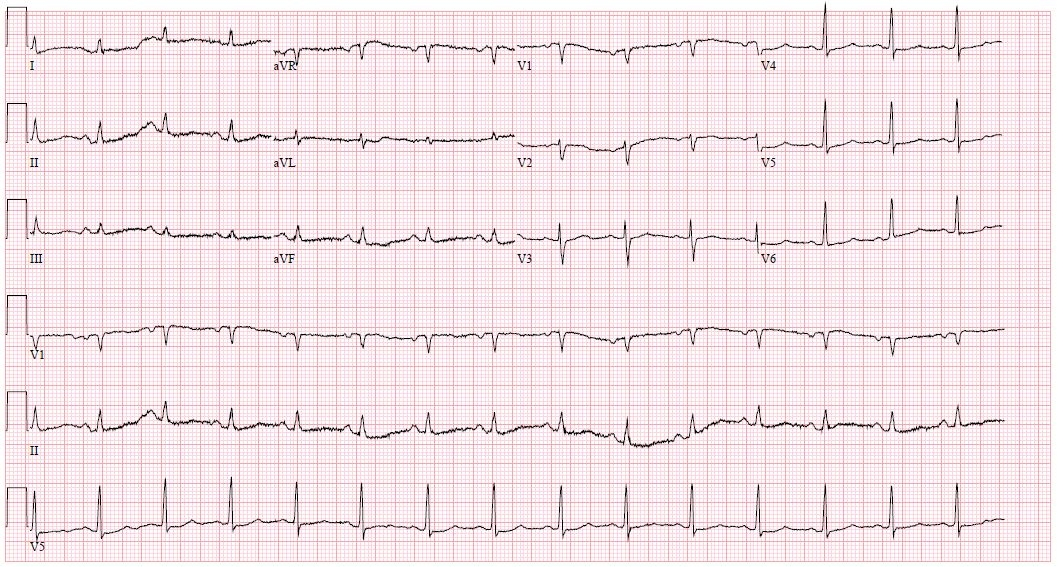 A recent echocardiogram showed a mildly dilated left ventricular cavity with akinesis of the anterior and anteroseptal walls as well as a left ventricular ejection fraction of 30%.
A recent echocardiogram showed a mildly dilated left ventricular cavity with akinesis of the anterior and anteroseptal walls as well as a left ventricular ejection fraction of 30%.
Which of the following additional treatments would most benefit this patient?
A)Biventricular pacing
B)Digoxin
C)Hydralazine
D)Metolazone
E)Spironolactone
Temperature is 37.2 C (99 F), blood pressure is 128/76 mm Hg, pulse is 76/min, and respirations are 16/min. Pulse oximetry is 94% on room air. The patient is in no apparent respiratory distress. Jugular venous pressure is measured at 8 cm H2O. Lung examination reveals clear lung fields with decreased breath sounds at the bases. Cardiac examination reveals normal S1 and S2 along with a 2/6 holosystolic murmur heard over the cardiac apex. There is minimal pitting edema around the ankles.
Laboratory results are as follows:
 ECG is shown in the exhibit.
ECG is shown in the exhibit. 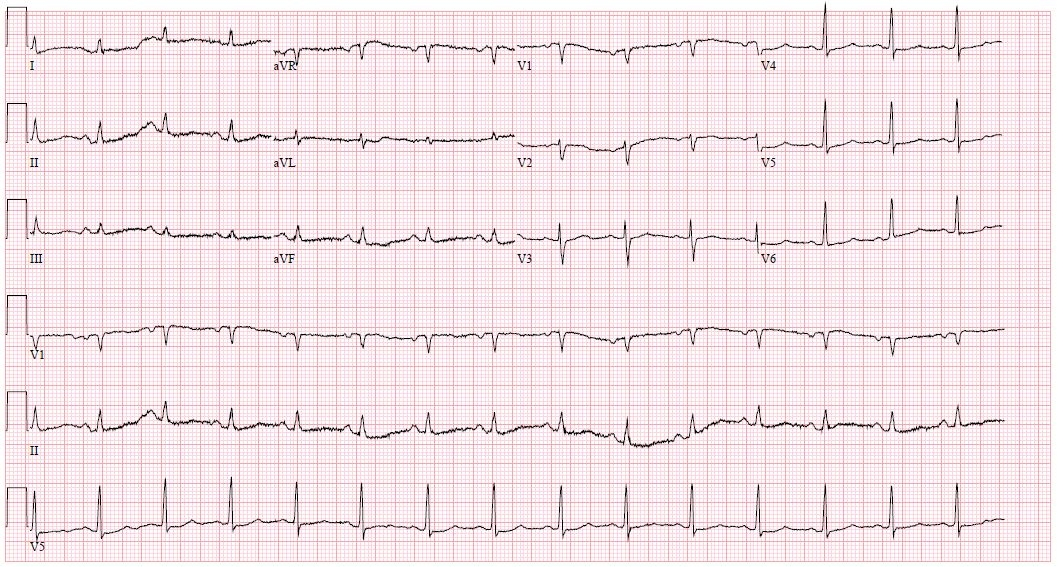 A recent echocardiogram showed a mildly dilated left ventricular cavity with akinesis of the anterior and anteroseptal walls as well as a left ventricular ejection fraction of 30%.
A recent echocardiogram showed a mildly dilated left ventricular cavity with akinesis of the anterior and anteroseptal walls as well as a left ventricular ejection fraction of 30%.Which of the following additional treatments would most benefit this patient?
A)Biventricular pacing
B)Digoxin
C)Hydralazine
D)Metolazone
E)Spironolactone

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
53
A 74-year-old man is admitted to the intensive care unit due to progressive shortness of breath for the last several days. He has a past medical history of coronary artery bypass grafting at age 50, mitral valve repair at age 64, ischemic cardiomyopathy with left ventricular ejection fraction of 20%, atrial fibrillation, type 2 diabetes mellitus, peripheral vascular disease, and stage III chronic kidney disease. The patient has had several hospital admissions for decompensated congestive heart failure over the past 2 years.
His temperature is 37.2 C (99 F), blood pressure is 90/60 mm Hg, pulse is 96/min, and respirations are 22/min. The patient's pulse oximetry is 88% on room air. He is in mild respiratory distress. Jugular venous pressure is elevated at 15 cm H2O. Lung examination reveals decreased breath sounds at the bases with bibasilar crackles up to the middle of the chest. Cardiac examination reveals irregular heart tones and a II/VI holosystolic murmur heard over the cardiac apex. There is 3+ lower extremity edema up to the mid thighs.
ECG shows atrial fibrillation at a rate of 94/min and low-voltage QRS complexes in the precordial leads. Chest x-ray reveals cardiomegaly and significant pulmonary vascular congestion in addition to small bilateral pleural effusions.
Which of the following best describes the benefits of milrinone infusion in this patient?
A)Alleviating symptoms of dyspnea
B)Decreasing frequency of hypotensive episodes
C)Decreasing risk of arrhythmias
D)Improving long-term mortality
E)Reducing frequency of ischemic events
His temperature is 37.2 C (99 F), blood pressure is 90/60 mm Hg, pulse is 96/min, and respirations are 22/min. The patient's pulse oximetry is 88% on room air. He is in mild respiratory distress. Jugular venous pressure is elevated at 15 cm H2O. Lung examination reveals decreased breath sounds at the bases with bibasilar crackles up to the middle of the chest. Cardiac examination reveals irregular heart tones and a II/VI holosystolic murmur heard over the cardiac apex. There is 3+ lower extremity edema up to the mid thighs.
ECG shows atrial fibrillation at a rate of 94/min and low-voltage QRS complexes in the precordial leads. Chest x-ray reveals cardiomegaly and significant pulmonary vascular congestion in addition to small bilateral pleural effusions.
Which of the following best describes the benefits of milrinone infusion in this patient?
A)Alleviating symptoms of dyspnea
B)Decreasing frequency of hypotensive episodes
C)Decreasing risk of arrhythmias
D)Improving long-term mortality
E)Reducing frequency of ischemic events

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
54
A 60-year-old man comes to the physician due to nighttime chest pain. The patient was diagnosed with extensive coronary artery disease a year ago and was offered coronary artery bypass grafting surgery. He refused surgery and instead opted for medical management. Since the medical therapy was started, the patient's symptoms have improved. He has angina during the daytime only after moderate to severe exertion. However, the patient still has been waking up 3-4 times per week in the middle of the night with substernal chest pain, which usually resolves spontaneously in 7-8 minutes but sometimes requires nitroglycerin. His other medical problems include difficult-to-control hypertension, hyperlipidemia, and peripheral vascular disease. The patient has smoked cigarettes for 35 years and quit 5 years ago. His medications include aspirin, metoprolol, isosorbide mononitrate, amlodipine, lisinopril, rosuvastatin, and nitroglycerin as needed. He takes all his medications during the morning hours.
His blood pressure is 150/82 mm Hg, pulse is 62/min and regular, and respirations are 14/min. The patient is obese with large neck circumference and a BMI of 34 kg/m2. Chest is clear to auscultation. There is no peripheral edema. The remainder of the examination is normal.
An electrocardiogram (ECG) performed in the office shows normal sinus rhythm with nonspecific T wave changes. His most recent echocardiogram showed a left ventricular ejection fraction of 60%. During exercise single photon emission computed tomography (SPECT) performed a month ago, the patient exercised for 8 minutes and reached 85% of age-predicted maximal predicted heart rate. He stopped due to fatigue and mild chest discomfort. Stress SPECT images showed a moderately extensive inferior wall reversible defect.
Which of the following is the most appropriate next step in management of this patient?
A)Add an evening dose of isosorbide mononitrate
B)Evaluate for esophageal disease
C)Increase the metoprolol dose and add an evening dose of ranolazine
D)Order pulmonary function tests with bronchodilator response
E)Refer for full nighttime polysomnography
His blood pressure is 150/82 mm Hg, pulse is 62/min and regular, and respirations are 14/min. The patient is obese with large neck circumference and a BMI of 34 kg/m2. Chest is clear to auscultation. There is no peripheral edema. The remainder of the examination is normal.
An electrocardiogram (ECG) performed in the office shows normal sinus rhythm with nonspecific T wave changes. His most recent echocardiogram showed a left ventricular ejection fraction of 60%. During exercise single photon emission computed tomography (SPECT) performed a month ago, the patient exercised for 8 minutes and reached 85% of age-predicted maximal predicted heart rate. He stopped due to fatigue and mild chest discomfort. Stress SPECT images showed a moderately extensive inferior wall reversible defect.
Which of the following is the most appropriate next step in management of this patient?
A)Add an evening dose of isosorbide mononitrate
B)Evaluate for esophageal disease
C)Increase the metoprolol dose and add an evening dose of ranolazine
D)Order pulmonary function tests with bronchodilator response
E)Refer for full nighttime polysomnography

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
55
A 37-year-old school teacher comes to the physician for a preventive care appointment. She denies any current symptoms, and she has not seen a doctor for many years. She takes over-the-counter vitamin and calcium supplements. She does not smoke and she drinks alcohol only on social occasions.
Her temperature is 37.2 C (99 F), blood pressure is 122/80 mm Hg, pulse is 84/min, and respirations are 14/min. Jugular venous pressure is normal. Cardiac auscultation reveals wide and fixed splitting of the second heart sound. There is a 2/6 mid-systolic ejection murmur heard best over the left second intercostal space. The remainder of her physical examination is unremarkable.
Which of the following would most likely be present on her electrocardiogram?
A)Abnormal Q waves in the inferior leads
B)Electrical alternans
C)Left ventricular hypertrophy
D)Right bundle branch block
E)Short PR interval and delta waves
Her temperature is 37.2 C (99 F), blood pressure is 122/80 mm Hg, pulse is 84/min, and respirations are 14/min. Jugular venous pressure is normal. Cardiac auscultation reveals wide and fixed splitting of the second heart sound. There is a 2/6 mid-systolic ejection murmur heard best over the left second intercostal space. The remainder of her physical examination is unremarkable.
Which of the following would most likely be present on her electrocardiogram?
A)Abnormal Q waves in the inferior leads
B)Electrical alternans
C)Left ventricular hypertrophy
D)Right bundle branch block
E)Short PR interval and delta waves

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
56
A 76-year-old woman comes to the office for follow-up. While vacationing in Florida 6 weeks ago, she had an episode of dizziness and palpitations that lasted several hours. She was seen in the local emergency department, where she was found to be in atrial fibrillation with rapid ventricular rate. The patient was then admitted to the hospital for further evaluation and treatment.
Echocardiography showed a mildly dilated left atrium, a normal left ventricle with an ejection fraction of 65%, and no significant valvular abnormalities. Discharge medications included apixaban and long-acting diltiazem. The patient has had no symptoms since hospital discharge.
Physical examination today is unremarkable. ECG performed in the office shows persistent atrial fibrillation with a ventricular rate of 68/min. The patient asks about the possibility of using medications to keep her sinus rhythm normal.
Compared to her current treatment, the use of antiarrhythmic medications in this patient will more likely result in which of the following?
A)Fewer hospitalizations
B)Higher risk of medication toxicity
C)Lower risk of congestive heart failure
D)Lower risk of major bleeding
E)Lower risk of systemic thromboembolic events
Echocardiography showed a mildly dilated left atrium, a normal left ventricle with an ejection fraction of 65%, and no significant valvular abnormalities. Discharge medications included apixaban and long-acting diltiazem. The patient has had no symptoms since hospital discharge.
Physical examination today is unremarkable. ECG performed in the office shows persistent atrial fibrillation with a ventricular rate of 68/min. The patient asks about the possibility of using medications to keep her sinus rhythm normal.
Compared to her current treatment, the use of antiarrhythmic medications in this patient will more likely result in which of the following?
A)Fewer hospitalizations
B)Higher risk of medication toxicity
C)Lower risk of congestive heart failure
D)Lower risk of major bleeding
E)Lower risk of systemic thromboembolic events

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
57
A 72-year-old man comes to the office due to occasional lightheadedness over the last 3 months. It occurs both during exertion and at rest and lasts about 2 minutes. The patient has no chest pain, dyspnea, or syncope. Other medical issues include hypertension, hyperlipidemia, and a right hemicolectomy 8 years ago for colon cancer. Medications include low-dose aspirin, hydrochlorothiazide, lisinopril, and rosuvastatin. The patient quit smoking 20 years ago and usually drinks 2 or 3 beers on weekends. He does not participate in any regular exercise program.
Physical examination is unremarkable. A treadmill exercise stress test is performed. The patient exercises for 7 minutes and 20 seconds and achieves a workload of 7.0 metabolic equivalents at 90% of his maximal age-predicted heart rate. No symptoms except fatigue are reported during the exercise. ECG shows no ST-segment changes suggestive of myocardial ischemia. During the last minute of exercise and the recovery period, he has a transient episode of third-degree atrioventricular block noted on the rhythm strip. Coronary angiogram shows 70% stenosis in the distal left anterior descending artery.
Which of the following is the most appropriate next step in management of this patient?
A)Order tilt table testing
B)Perform 24-hour ECG (Holter) monitor
C)Provide reassurance and follow up in 4-6 weeks
D)Refer for percutaneous coronary intervention
E)Refer for permanent pacemaker implantation
Physical examination is unremarkable. A treadmill exercise stress test is performed. The patient exercises for 7 minutes and 20 seconds and achieves a workload of 7.0 metabolic equivalents at 90% of his maximal age-predicted heart rate. No symptoms except fatigue are reported during the exercise. ECG shows no ST-segment changes suggestive of myocardial ischemia. During the last minute of exercise and the recovery period, he has a transient episode of third-degree atrioventricular block noted on the rhythm strip. Coronary angiogram shows 70% stenosis in the distal left anterior descending artery.
Which of the following is the most appropriate next step in management of this patient?
A)Order tilt table testing
B)Perform 24-hour ECG (Holter) monitor
C)Provide reassurance and follow up in 4-6 weeks
D)Refer for percutaneous coronary intervention
E)Refer for permanent pacemaker implantation

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
58
A 48-year-old man comes to the office for evaluation of palpitations. The patient wakes up frequently at night with a pounding sensation in his chest. He has also experienced "skipped beats" and palpitations during the day on several occasions. He has had no chest pain, dyspnea, lightheadedness, or syncope. The patient lives alone after a recent divorce and says he is afraid that he may die in his sleep. He also states that he feels "stressed out" and has had frequent headaches and feels tired throughout the day. He has smoked a pack of cigarettes daily for the past 20 years and drinks alcohol on the weekends, sometimes excessively.
Blood pressure is 152/89 mm Hg and pulse is 78/min. BMI is 33 kg/m2. Heart sounds are normal and the lungs are clear on auscultation. The remainder of the physical examination is within normal limits.
Blood cell counts, serum chemistry studies, and thyroid function tests obtained on a previous visit are within normal limits. ECG shows sinus rhythm with nonspecific T-wave changes, and echocardiography reveals mild left atrial enlargement but is otherwise normal.
Continuous ambulatory ECG (Holter) monitoring is performed for 24 hours and shows frequent premature ventricular contractions, several episodes of bradycardia with heart rates around 30/min between 2 AM and 5 AM, and a 5-second sinus pause followed by a short run of atrial fibrillation at a rate of 130/min at 4:30 AM.
Which of the following is the most appropriate next step in management of this patient?
A)Evaluation for alcohol abuse and dependence
B)Exercise stress testing
C)Full-night polysomnography with ECG
D)Referral for pacemaker implantation
E)Selective serotonin reuptake inhibitor
Blood pressure is 152/89 mm Hg and pulse is 78/min. BMI is 33 kg/m2. Heart sounds are normal and the lungs are clear on auscultation. The remainder of the physical examination is within normal limits.
Blood cell counts, serum chemistry studies, and thyroid function tests obtained on a previous visit are within normal limits. ECG shows sinus rhythm with nonspecific T-wave changes, and echocardiography reveals mild left atrial enlargement but is otherwise normal.
Continuous ambulatory ECG (Holter) monitoring is performed for 24 hours and shows frequent premature ventricular contractions, several episodes of bradycardia with heart rates around 30/min between 2 AM and 5 AM, and a 5-second sinus pause followed by a short run of atrial fibrillation at a rate of 130/min at 4:30 AM.
Which of the following is the most appropriate next step in management of this patient?
A)Evaluation for alcohol abuse and dependence
B)Exercise stress testing
C)Full-night polysomnography with ECG
D)Referral for pacemaker implantation
E)Selective serotonin reuptake inhibitor

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
59
A 32-year-old primigravida at 28 weeks gestation is referred from the obstetrics clinic due to shortness of breath. She is an immigrant from Mexico. Her pregnancy has thus far been uncomplicated except for nausea in the first trimester. Over the last four weeks, she has been feeling tired and becomes short of breath with activities that she was previously able to perform with ease, such as walking several blocks or climbing stairs on the subway. She denies chest pain, wheezing, cough, or nocturnal symptoms. Her other medical problems include obesity and mild intermittent asthma. Cardiac auscultation findings can be heard in the exhibit.
Which of the following is the most likely diagnosis?
A)Aortic stenosis
B)Mitral stenosis
C)Normal pregnancy
D)Peripartum cardiomyopathy
E)Ventricular septal defect
Which of the following is the most likely diagnosis?
A)Aortic stenosis
B)Mitral stenosis
C)Normal pregnancy
D)Peripartum cardiomyopathy
E)Ventricular septal defect

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
60
A 60-year-old man comes to the office due to occasional episodes of dizziness, usually when he tries to get up quickly. He had sustained an anterior wall myocardial infarction 4 months ago, and had emergent percutaneous revascularization of his proximal left anterior descending artery with placement of a stent. He has no chest pain, shortness of breath, palpitations, or syncope. He has been able to resume walking about 3 miles every day.
His home medications include aspirin, clopidogrel, rosuvastatin, carvedilol, sacubitril-valsartan, and spironolactone. Echocardiography performed 1 week ago showed a large area of dyskinesia in the anterior and anterolateral myocardial segments, with an ejection fraction of 25%. There was also mild mitral and tricuspid regurgitation present. These findings are similar to the earlier echocardiogram performed at the time of myocardial infarction.
His blood pressure is 112/62 mm Hg and pulse is 68/min. A soft, 2/6 holosystolic murmur is heard at the cardiac apex in the left lateral position. Lungs are clear to auscultation.
His ECG in the office shows sinus rhythm and Q waves in precordial leads.
Which of the following is the most appropriate next step in management?
A)30-day ECG monitoring
B)Electrophysiological study
C)Implantable cardioverter-defibrillator placement
D)No additional intervention
E)Submaximal exercise testing
His home medications include aspirin, clopidogrel, rosuvastatin, carvedilol, sacubitril-valsartan, and spironolactone. Echocardiography performed 1 week ago showed a large area of dyskinesia in the anterior and anterolateral myocardial segments, with an ejection fraction of 25%. There was also mild mitral and tricuspid regurgitation present. These findings are similar to the earlier echocardiogram performed at the time of myocardial infarction.
His blood pressure is 112/62 mm Hg and pulse is 68/min. A soft, 2/6 holosystolic murmur is heard at the cardiac apex in the left lateral position. Lungs are clear to auscultation.
His ECG in the office shows sinus rhythm and Q waves in precordial leads.
Which of the following is the most appropriate next step in management?
A)30-day ECG monitoring
B)Electrophysiological study
C)Implantable cardioverter-defibrillator placement
D)No additional intervention
E)Submaximal exercise testing

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
61
A 54-year-old man comes to the physician with chest discomfort. During the last 6 months, the patient has had left-sided chest pain radiating to the left shoulder, which is commonly provoked by exertion but also occurs at rest. The chest pain lasts a few seconds to several minutes, and he can usually "walk it off." Past medical history includes hypertension, hyperlipidemia, and peptic ulcer disease. The patient received a permanent pacemaker 6 years ago after an episode of syncope. His father also had a pacemaker. Current medications include lisinopril, amlodipine, famotidine, and rosuvastatin.
His blood pressure is 111/70 mm Hg and pulse is 67/min. Chest is clear to auscultation. No cardiac murmurs or carotid bruits are appreciated. The abdomen is nontender. Pulses are full and symmetric bilaterally.
Electrocardiogram shows normal sinus rhythm with paced ventricular complexes (atrial sensed, ventricular paced rhythm).
Which of the following is the best next step in management of this patient?
A)Coronary angiography
B)Exercise echocardiography
C)Exercise electrocardiogram (ECG) testing
D)Exercise radionuclide imaging
E)Pharmacologic radionuclide imaging
His blood pressure is 111/70 mm Hg and pulse is 67/min. Chest is clear to auscultation. No cardiac murmurs or carotid bruits are appreciated. The abdomen is nontender. Pulses are full and symmetric bilaterally.
Electrocardiogram shows normal sinus rhythm with paced ventricular complexes (atrial sensed, ventricular paced rhythm).
Which of the following is the best next step in management of this patient?
A)Coronary angiography
B)Exercise echocardiography
C)Exercise electrocardiogram (ECG) testing
D)Exercise radionuclide imaging
E)Pharmacologic radionuclide imaging

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
62
A 55-year-old man comes to the physician complaining of an episode of rectal bleeding. His past medical history includes chronic constipation for which he takes over-the-counter laxatives. He also has a history of intravenous drug use and an episode of tricuspid and mitral valve infective endocarditis 15 years ago. Since that episode, he has stopped using illicit drugs. The patient has a 20-pack-year smoking history and drinks 1-2 cans of beer daily. Family history is not significant. He is allergic to penicillin.
His vital signs are within normal limits. Physical examination shows no abnormalities. Stool is positive for occult blood.
The patient is scheduled for a colonoscopy.
Which of the following is the most appropriate next step in management?
A)Cephalexin prior to the procedure
B)Clindamycin prior to the procedure
C)Perform transthoracic echocardiogram
D)Proceed with the colonoscopy
E)Vancomycin prior to the procedure
His vital signs are within normal limits. Physical examination shows no abnormalities. Stool is positive for occult blood.
The patient is scheduled for a colonoscopy.
Which of the following is the most appropriate next step in management?
A)Cephalexin prior to the procedure
B)Clindamycin prior to the procedure
C)Perform transthoracic echocardiogram
D)Proceed with the colonoscopy
E)Vancomycin prior to the procedure

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
63
A 25-year-old woman comes to the physician with complaints of fatigue and worsening shortness of breath. She first noticed her symptoms 8 months ago. She awoke 2 days ago with palpitations and severe coughing and noticed some bright-colored blood in her sputum. She emigrated from the Philippines 2 years ago and works as a nurse at a local hospital. She has no history of smoking, illicit drug use, or unprotected sexual intercourse. She has no past medical history of childhood illnesses.
Her blood pressure is 106/62 mm Hg, and pulse is 82/min and regular. Neck veins are pulsatile with a prominent c-v wave. Lungs fields are clear with minimal rales heard at both lung bases. Heart sounds are regular with a loud first heart sound. A low-pitched mid-diastolic rumble and a snapping sound after the second heart sound are present at the cardiac apex. There is also a loud holosystolic murmur heard over the precordium that increases with inspiration.
Which of the following is the most likely diagnosis?
A)Aortic regurgitation
B)Constrictive pericarditis
C)Ebstein's anomaly
D)Mitral stenosis
E)Ventricular septal defect
Her blood pressure is 106/62 mm Hg, and pulse is 82/min and regular. Neck veins are pulsatile with a prominent c-v wave. Lungs fields are clear with minimal rales heard at both lung bases. Heart sounds are regular with a loud first heart sound. A low-pitched mid-diastolic rumble and a snapping sound after the second heart sound are present at the cardiac apex. There is also a loud holosystolic murmur heard over the precordium that increases with inspiration.
Which of the following is the most likely diagnosis?
A)Aortic regurgitation
B)Constrictive pericarditis
C)Ebstein's anomaly
D)Mitral stenosis
E)Ventricular septal defect

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
64
A 65-year-old overweight woman comes to the physician with 4 weeks of persistent dry, hacking cough that interferes with her sleep. She has minimal sputum production and no associated upper respiratory symptoms, dyspnea, fever, chills, or generalized malaise. She has never had asthma or episodes of wheezing. She does not smoke cigarettes. Her medical problems include newly diagnosed hypertension, hyperlipidemia, and osteoarthritis of the knees. Her blood pressure is currently well controlled with hydrochlorothiazide and lisinopril. In the past, she developed severe lower-extremity swelling and palpitations with amlodipine.
Her blood pressure is 130/80 mm Hg, pulse is 84/min, and respirations are 14/min. Pulse oximetry shows 95% on room air. Cardiopulmonary examination is unremarkable.
Laboratory results are as follows:

Which of the following is the best next step in managing this patient?
A)Lower the dose of lisinopril
B)Order chest x-ray
C)Order pulmonary function test
D)Stop lisinopril and start losartan
E)Stop lisinopril and start ramipril
Her blood pressure is 130/80 mm Hg, pulse is 84/min, and respirations are 14/min. Pulse oximetry shows 95% on room air. Cardiopulmonary examination is unremarkable.
Laboratory results are as follows:

Which of the following is the best next step in managing this patient?
A)Lower the dose of lisinopril
B)Order chest x-ray
C)Order pulmonary function test
D)Stop lisinopril and start losartan
E)Stop lisinopril and start ramipril

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
65
A 50-year-old woman seeks follow-up for chronic kidney disease diagnosed during routine laboratory workup before knee surgery. A 24-hour urine shows 1.5 g/day of proteinuria, and urinalysis shows a few granular casts. Her history, physical examination, and screening laboratory findings do not indicate a cause for her chronic kidney disease. A renal ultrasound reveals echogenic kidneys measuring about 9 cm bilaterally without evidence of obstructive uropathy. She takes no medications.
Her blood pressure is 152/92 mm Hg and pulse is 79/min. The physical examination is within normal limits.
The patient's most recent laboratory results are as follows:
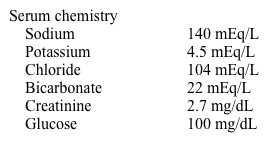
Which of the following would be the best therapeutic agent for this patient?
A)Amlodipine
B)Benazepril
C)Carvedilol
D)Clonidine
E)Hydrochlorothiazide
Her blood pressure is 152/92 mm Hg and pulse is 79/min. The physical examination is within normal limits.
The patient's most recent laboratory results are as follows:
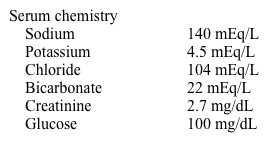
Which of the following would be the best therapeutic agent for this patient?
A)Amlodipine
B)Benazepril
C)Carvedilol
D)Clonidine
E)Hydrochlorothiazide

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
66
A 22-year-old African American man is evaluated for an abnormal ECG obtained at a health fair. He has no complaints and says that he has been healthy all his life. He runs 6-8 miles a day and plays basketball for several hours every weekend. The patient has no symptoms during physical activity. His paternal uncle suffered from diabetes mellitus and died of a heart attack at age 50. His mother had a minor stroke at age 40.
Examination shows a muscular, well-built man. His blood pressure is 132/90 mm Hg on the right arm and 137/85 mm Hg on the left. His pulse is 54/min. Lungs are clear on auscultation, he has normal first and second heart sounds, and peripheral pulses are full and symmetric.
ECG shows high voltage in precordial leads and downsloping ST-segment depression with T-wave inversion in leads V4-V6. An echocardiogram shows left ventricular hypertrophy with septal thickness of 18 mm and posterior wall thickness of 12 mm (normal ≤10 mm). There is no valvular disease, systolic anterior motion of the mitral valve, or left ventricular outflow tract gradient at rest or with Valsalva maneuver.
Which of the following is the most likely diagnosis?
A)Athlete's heart
B)Coronary artery anomaly
C)Hypertensive heart disease
D)Hypertrophic cardiomyopathy
E)Sarcoidosis
Examination shows a muscular, well-built man. His blood pressure is 132/90 mm Hg on the right arm and 137/85 mm Hg on the left. His pulse is 54/min. Lungs are clear on auscultation, he has normal first and second heart sounds, and peripheral pulses are full and symmetric.
ECG shows high voltage in precordial leads and downsloping ST-segment depression with T-wave inversion in leads V4-V6. An echocardiogram shows left ventricular hypertrophy with septal thickness of 18 mm and posterior wall thickness of 12 mm (normal ≤10 mm). There is no valvular disease, systolic anterior motion of the mitral valve, or left ventricular outflow tract gradient at rest or with Valsalva maneuver.
Which of the following is the most likely diagnosis?
A)Athlete's heart
B)Coronary artery anomaly
C)Hypertensive heart disease
D)Hypertrophic cardiomyopathy
E)Sarcoidosis

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
67
A 62-year-old man comes to the office to follow up hypertension. He has a long history of hypertension treated with amlodipine and obstructive sleep apnea requiring continuous positive airway pressure at night. The patient does not use tobacco, alcohol, or illicit drugs and has no medication allergies.
Blood pressure is 134/90 mm Hg and pulse is 78/min. BMI is 33 kg/m2. Physical examination is unremarkable.
Laboratory results are as follows:
 Liver function tests are normal.
Liver function tests are normal.
The patient is counseled on indications for lipid-lowering therapy with statin drugs. He is at greatest risk for which of the following adverse effects if he starts high-intensity atorvastatin therapy?
A)Acute liver failure
B)Hemorrhagic stroke
C)New-onset diabetes mellitus
D)New-onset hypothyroidism
E)Rhabdomyolysis
Blood pressure is 134/90 mm Hg and pulse is 78/min. BMI is 33 kg/m2. Physical examination is unremarkable.
Laboratory results are as follows:
 Liver function tests are normal.
Liver function tests are normal.The patient is counseled on indications for lipid-lowering therapy with statin drugs. He is at greatest risk for which of the following adverse effects if he starts high-intensity atorvastatin therapy?
A)Acute liver failure
B)Hemorrhagic stroke
C)New-onset diabetes mellitus
D)New-onset hypothyroidism
E)Rhabdomyolysis

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
68
A 53-year-old man comes to the office due to exertional dyspnea. He can walk only 2 blocks before becoming short of breath. The patient has no chest pain, palpitations, or syncope. He was hospitalized 8 months ago with heart failure with reduced ejection fraction and treated with diuretics. Cardiac catheterization showed nonobstructive coronary artery disease. Echocardiogram revealed left ventricle enlargement with an ejection fraction of 25%. Current medications include carvedilol, sacubitril-valsartan, furosemide, and spironolactone.
Blood pressure is 112/68 mm Hg, pulse is 62/min, and oxygen saturation is 99% on room air. Jugular venous pressure is estimated at 7 cm H2O. Breath sounds are decreased at the right lung base. The point of maximal impulse is displaced laterally. A regular heart rhythm and an S3 are heard. The liver span is 8 cm. The tip of the spleen is not palpated. There is mild edema of both ankles.
Laboratory results are as follows:
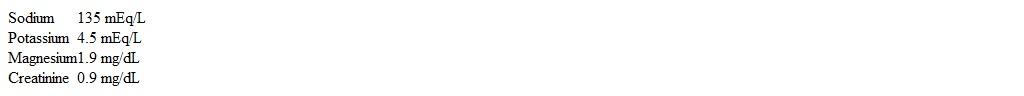 Repeat transthoracic echocardiogram is unchanged from the previous study.
Repeat transthoracic echocardiogram is unchanged from the previous study.
Which of the following ECG findings will change this patient's heart failure management?
A)Increased QTc interval
B)Precordial Q waves
C)Prolonged QRS duration
D)QRS axis shift
E)Shortened PR interval
Blood pressure is 112/68 mm Hg, pulse is 62/min, and oxygen saturation is 99% on room air. Jugular venous pressure is estimated at 7 cm H2O. Breath sounds are decreased at the right lung base. The point of maximal impulse is displaced laterally. A regular heart rhythm and an S3 are heard. The liver span is 8 cm. The tip of the spleen is not palpated. There is mild edema of both ankles.
Laboratory results are as follows:
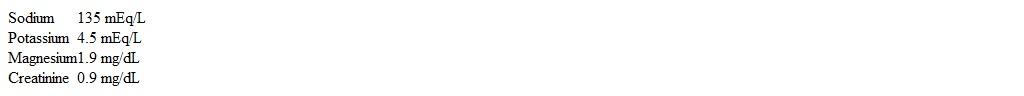 Repeat transthoracic echocardiogram is unchanged from the previous study.
Repeat transthoracic echocardiogram is unchanged from the previous study.Which of the following ECG findings will change this patient's heart failure management?
A)Increased QTc interval
B)Precordial Q waves
C)Prolonged QRS duration
D)QRS axis shift
E)Shortened PR interval

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
69
A 72-year-old woman with type 2 diabetes mellitus is brought to the emergency department with dyspnea and chest pressure that started about 6 hours earlier.
Her blood pressure is 82/62 mm Hg and pulse is 104/min. Pulse oximetry shows 92% on 15 L oxygen by face mask. She is mildly confused. Examination shows moist oral mucosa and distended neck veins in a sitting position. The apical impulse is displaced to the left with a third heart sound. Lung examination shows fine crackles one third of the way up in bilateral lung fields. Lower extremities are cold to the touch with weak peripheral pulses.
Her initial ECG shows sinus tachycardia and a new left bundle branch block.
Which of the following measures instituted immediately is most likely to improve survival in this patient?
A)Hemodynamic monitoring with pulmonary artery catheter
B)Intra-aortic balloon pump insertion
C)Milrinone infusion
D)Norepinephrine infusion
E)Percutaneous coronary intervention
Her blood pressure is 82/62 mm Hg and pulse is 104/min. Pulse oximetry shows 92% on 15 L oxygen by face mask. She is mildly confused. Examination shows moist oral mucosa and distended neck veins in a sitting position. The apical impulse is displaced to the left with a third heart sound. Lung examination shows fine crackles one third of the way up in bilateral lung fields. Lower extremities are cold to the touch with weak peripheral pulses.
Her initial ECG shows sinus tachycardia and a new left bundle branch block.
Which of the following measures instituted immediately is most likely to improve survival in this patient?
A)Hemodynamic monitoring with pulmonary artery catheter
B)Intra-aortic balloon pump insertion
C)Milrinone infusion
D)Norepinephrine infusion
E)Percutaneous coronary intervention

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
70
A 64-year-old man comes to the office for a routine follow-up. He has no current concerns. Last year, he underwent a transthoracic echocardiogram for a cardiac murmur and was diagnosed with mild calcific aortic stenosis. The mean gradient across the valve was 18 mm Hg (normal <5 mm Hg), and the estimated valve area was 1.6 cm2 (normal 3-4 cm2). The patient does not use tobacco, alcohol, or illicit drugs. He jogs and bikes 3 times a week.
Blood pressure is 136/78 mm Hg, and pulse is 77/min and regular. BMI is 29 kg/m2. A 3/6 systolic ejection-type murmur is heard at the upper sternal border radiating to the carotids. S4 is heard at the apex at end-expiration. Lungs are clear to auscultation. The remainder of the examination is unremarkable.
ECG shows normal sinus rhythm with voltage criteria for left ventricular hypertrophy and nonspecific ST segment changes.
Laboratory results are as follows:
 What is the best next step in management of this patient?
What is the best next step in management of this patient?
A)Addition of beta blocker
B)Education about antibiotic prophylaxis
C)No intervention and clinical follow-up in a year
D)Transthoracic echocardiogram
E)Treadmill exercise testing
Blood pressure is 136/78 mm Hg, and pulse is 77/min and regular. BMI is 29 kg/m2. A 3/6 systolic ejection-type murmur is heard at the upper sternal border radiating to the carotids. S4 is heard at the apex at end-expiration. Lungs are clear to auscultation. The remainder of the examination is unremarkable.
ECG shows normal sinus rhythm with voltage criteria for left ventricular hypertrophy and nonspecific ST segment changes.
Laboratory results are as follows:
 What is the best next step in management of this patient?
What is the best next step in management of this patient?A)Addition of beta blocker
B)Education about antibiotic prophylaxis
C)No intervention and clinical follow-up in a year
D)Transthoracic echocardiogram
E)Treadmill exercise testing

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
71
A 64-year-old man comes to the office with pain and swelling over the left upper chest for 7 days. He also had an episode of fever, but no cough, sore throat, abdominal pain, diarrhea, or urinary symptoms. Five months ago, the patient had a single-lead implantable cardioverter-defibrillator placed due to a sudden cardiac arrest. His other medical problems include nonischemic cardiomyopathy (ejection fraction, 20%) and chronic kidney disease.
Temperature is 36.7 (98 F), blood pressure is 109/70 mm Hg, pulse is 70/min, and respirations are 16/min. Pulse oximetry is 95% on room air. Examination shows clear lungs and normal S1 and S2. Swelling, erythema, and tenderness are present over the defibrillator generator. A small amount of discharge is seen through an erosion of the healed suture line.
Leukocytes are 11,200/mm3. Two sets of blood cultures are negative after 2 days.
Which of the following is the best next step in management of this patient?
A)Incision and drainage followed by antibiotics
B)Removal of the generator and lead followed by antibiotics
C)Removal of the generator followed by antibiotics
D)Treatment with anti-staphylococcal antibiotic for 6 weeks
Temperature is 36.7 (98 F), blood pressure is 109/70 mm Hg, pulse is 70/min, and respirations are 16/min. Pulse oximetry is 95% on room air. Examination shows clear lungs and normal S1 and S2. Swelling, erythema, and tenderness are present over the defibrillator generator. A small amount of discharge is seen through an erosion of the healed suture line.
Leukocytes are 11,200/mm3. Two sets of blood cultures are negative after 2 days.
Which of the following is the best next step in management of this patient?
A)Incision and drainage followed by antibiotics
B)Removal of the generator and lead followed by antibiotics
C)Removal of the generator followed by antibiotics
D)Treatment with anti-staphylococcal antibiotic for 6 weeks

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
72
A 67-year-old man with known coronary artery disease complains of exertional chest pain that limits his daily activities. He has long-standing angina symptoms. The patient reports that over the last month his exercise tolerance has decreased significantly and he has chest pain after walking only half a block. He takes sublingual nitroglycerin 6-7 times a day. Seven years ago he had coronary artery bypass surgery due to severe multivessel coronary artery disease with 3 venous grafts and left internal mammary artery graft to the left anterior descending artery.
Since then, he has had 2 cardiac catheterizations; the last showed occlusion of venous grafts and progressive native coronary artery disease not amenable to revascularization. His last left ventricular ejection fraction was 45%. The patient's medications include aspirin, lisinopril, atorvastatin, amlodipine, metoprolol, and nitroglycerin as needed. Two months ago, he was started on isosorbide dinitrate that he currently takes 4 times daily.
His blood pressure is 122/70 mm Hg and pulse is 55/min. No murmurs are heard on cardiac auscultation. Peripheral pulses are 2+ bilaterally. The remainder of the examination is within normal limits.
Which of the following most likely contributes to this patient's current symptoms?
A)Ischemic conditioning
B)Medication tolerance
C)Rebound angina
D)Steal phenomenon
E)Variant angina
Since then, he has had 2 cardiac catheterizations; the last showed occlusion of venous grafts and progressive native coronary artery disease not amenable to revascularization. His last left ventricular ejection fraction was 45%. The patient's medications include aspirin, lisinopril, atorvastatin, amlodipine, metoprolol, and nitroglycerin as needed. Two months ago, he was started on isosorbide dinitrate that he currently takes 4 times daily.
His blood pressure is 122/70 mm Hg and pulse is 55/min. No murmurs are heard on cardiac auscultation. Peripheral pulses are 2+ bilaterally. The remainder of the examination is within normal limits.
Which of the following most likely contributes to this patient's current symptoms?
A)Ischemic conditioning
B)Medication tolerance
C)Rebound angina
D)Steal phenomenon
E)Variant angina

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
73
A 62-year-old man with known diabetes mellitus and hyperlipidemia comes to the physician with right hip pain for the last 3 months. The pain is aching, brought on by walking (especially uphill), and goes away quickly with standing still. It is sometimes accompanied by leg weakness, causing the patient to hold on to stationary objects.
The patient's other medical problems include gallstones, hyperlipidemia, benign prostate hyperplasia, and erectile dysfunction. He takes long-acting insulin at night. His dose of simvastatin was recently increased due to an elevated LDL cholesterol level.
Which of the following physical findings is most consistent with this patient's diagnosis?
A)Decreased vibration sense at ankles
B)Femoral bruit
C)Hip pain on passive external rotation
D)Limited lumbar spine mobility
E)Muscle tenderness
The patient's other medical problems include gallstones, hyperlipidemia, benign prostate hyperplasia, and erectile dysfunction. He takes long-acting insulin at night. His dose of simvastatin was recently increased due to an elevated LDL cholesterol level.
Which of the following physical findings is most consistent with this patient's diagnosis?
A)Decreased vibration sense at ankles
B)Femoral bruit
C)Hip pain on passive external rotation
D)Limited lumbar spine mobility
E)Muscle tenderness

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
74
A 60-year-old man comes to the office for presurgical evaluation before right total knee replacement. He describes pain and limited mobility due to severe knee osteoarthritis. The patient has gained 4.5 kg (10 lb) over the last 6 months due to decreased physical activity. He has a history of coronary artery disease, hypertension, and hyperlipidemia. Current medications are low-dose aspirin, prasugrel, metoprolol, valsartan, and rosuvastatin.
A year ago, the patient underwent sirolimus-eluting stent implantation into the left anterior descending artery due to angina. Two months ago, echocardiogram showed normal left ventricular systolic function and no wall motion abnormalities.
Which of the following is the best preoperative recommendation for this patient?
A)Continue aspirin, discontinue prasugrel
B)Continue both antiplatelet medications
C)Continue prasugrel, discontinue aspirin
D)Discontinue both antiplatelet medications
E)Postpone surgery
A year ago, the patient underwent sirolimus-eluting stent implantation into the left anterior descending artery due to angina. Two months ago, echocardiogram showed normal left ventricular systolic function and no wall motion abnormalities.
Which of the following is the best preoperative recommendation for this patient?
A)Continue aspirin, discontinue prasugrel
B)Continue both antiplatelet medications
C)Continue prasugrel, discontinue aspirin
D)Discontinue both antiplatelet medications
E)Postpone surgery

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
75
A 62-year-old man comes to the physician for evaluation of chest and upper abdominal discomfort for the past 6 months. He has noted the discomfort during his daily walks and sometimes at rest, especially after heavy meals. His other medical problems include hypertension, type 2 diabetes mellitus, and gastroesophageal reflux disease. His medications include metformin, aspirin, hydrochlorothiazide, and lisinopril.
The patient's blood pressure is 142/82 mm Hg and pulse is 74/min. BMI is 33 kg/m2. His physical examination is remarkable for chronic venous stasis and 1+ swelling of both lower extremities.
The patient is referred for an exercise radionuclide stress test. After 5 minutes on the Bruce protocol, he is able to reach 85% of maximum age-predicted heart rate. His blood pressure at baseline is 148/88 mm Hg and is 142/86 mm Hg at peak exercise. He complains of discomfort in both arms and his chest during the end of exercise, which resolves 5 minutes later during the recovery period. ECG monitoring shows 2-mm horizontal ST-segment depression in leads II, aVF, and V4-V6 at peak stress with normalization at recovery. However, myocardial perfusion images show no evidence of ischemia, and ejection fraction is calculated at 65%.
Which of the following is the most appropriate next step in management?
A)Add clopidogrel and nitroglycerin as needed
B)Evaluate for noncardiac cause of chest pain
C)Prescribe proton pump inhibitor
D)Reassure and follow up in 3-6 months
E)Refer for cardiac catheterization
The patient's blood pressure is 142/82 mm Hg and pulse is 74/min. BMI is 33 kg/m2. His physical examination is remarkable for chronic venous stasis and 1+ swelling of both lower extremities.
The patient is referred for an exercise radionuclide stress test. After 5 minutes on the Bruce protocol, he is able to reach 85% of maximum age-predicted heart rate. His blood pressure at baseline is 148/88 mm Hg and is 142/86 mm Hg at peak exercise. He complains of discomfort in both arms and his chest during the end of exercise, which resolves 5 minutes later during the recovery period. ECG monitoring shows 2-mm horizontal ST-segment depression in leads II, aVF, and V4-V6 at peak stress with normalization at recovery. However, myocardial perfusion images show no evidence of ischemia, and ejection fraction is calculated at 65%.
Which of the following is the most appropriate next step in management?
A)Add clopidogrel and nitroglycerin as needed
B)Evaluate for noncardiac cause of chest pain
C)Prescribe proton pump inhibitor
D)Reassure and follow up in 3-6 months
E)Refer for cardiac catheterization

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
76
A 32-year-old white man is referred for evaluation of a murmur noted on a pre-employment physical. He has no specific complaints. He is physically active and runs 4-5 miles almost every day. His older brother died of presumed sudden cardiac arrest at age 37 years. On physical examination, there is a wide, fixed splitting of the second heart sound. A faint mid-systolic ejection murmur is heard best over the left second intercostal space. Otherwise, his physical examination is unremarkable. An echocardiogram confirms the presence of a large secundum atrial septal defect.
Which of the following is the most likely explanation for the murmur?
A)Dilatation of the main pulmonary artery
B)Increased flow through the pulmonic valve
C)Increased flow through the tricuspid valve
D)Prolapse of the anterior mitral leaflet
E)Shunt flow through the atrial septal defect
Which of the following is the most likely explanation for the murmur?
A)Dilatation of the main pulmonary artery
B)Increased flow through the pulmonic valve
C)Increased flow through the tricuspid valve
D)Prolapse of the anterior mitral leaflet
E)Shunt flow through the atrial septal defect

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
77
A 71-year-old man comes to the physician for routine evaluation. He has no symptoms and considers himself healthy. He walks several miles a day and jogs twice a week for 5 miles. The patient has no history of chest pain or syncope. Five years ago he had inguinal hernia repair without complications. His father died at age 90 of "old age" and his mother died of breast cancer. He has never smoked.
His blood pressure is 126/70 mm Hg and pulse is 72/min and regular. He has no jugular venous distension when sitting. The apical impulse is displaced to the left. A 2/6 holosystolic murmur is heard at the apex. The lungs are clear, and there is no organomegaly. The pulses are full bilaterally and there is no peripheral edema. ECG shows normal sinus rhythm with abnormal Q waves in leads V2 to V4. Transthoracic echocardiography shows left ventricular enlargement, anterior wall and apical akinesis, and left ventricular ejection fraction of 35%. There is mild mitral regurgitation. He declines coronary angiogram.
Which of the following is the best next step in management of this patient?
A)Beta blocker and an angiotensin system inhibitor
B)Beta blocker and a loop diuretic
C)Beta blocker, digoxin, and an angiotensin system inhibitor
D)Reassurance and routine follow-up
E)Salt restriction to less than 2 g per day
His blood pressure is 126/70 mm Hg and pulse is 72/min and regular. He has no jugular venous distension when sitting. The apical impulse is displaced to the left. A 2/6 holosystolic murmur is heard at the apex. The lungs are clear, and there is no organomegaly. The pulses are full bilaterally and there is no peripheral edema. ECG shows normal sinus rhythm with abnormal Q waves in leads V2 to V4. Transthoracic echocardiography shows left ventricular enlargement, anterior wall and apical akinesis, and left ventricular ejection fraction of 35%. There is mild mitral regurgitation. He declines coronary angiogram.
Which of the following is the best next step in management of this patient?
A)Beta blocker and an angiotensin system inhibitor
B)Beta blocker and a loop diuretic
C)Beta blocker, digoxin, and an angiotensin system inhibitor
D)Reassurance and routine follow-up
E)Salt restriction to less than 2 g per day

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
78
A 60-year-old man comes to the office for presurgical evaluation before right-sided total knee replacement. He has pain and limited mobility due to severe knee osteoarthritis, and has gained 4.5 kg (10 lb) over the last 6 months due to decreased physical activity. Other medical problems include coronary artery disease, hypertension, and hyperlipidemia. Four months ago, the patient underwent sirolimus-eluting stent implantation into the left anterior descending artery due to angina. Current medications are low-dose aspirin, prasugrel, metoprolol, valsartan, and rosuvastatin.
ECG shows sinus rhythm with no pathologic Q waves or ST-segment abnormalities. Echocardiogram shows normal left ventricular systolic function and no wall motion abnormalities.
Which of the following is the best recommendation for this patient before surgery?
A)Continue aspirin, discontinue prasugrel
B)Continue both antiplatelet medications
C)Continue prasugrel, discontinue aspirin
D)Hold both antiplatelet medications
E)Postpone surgery
ECG shows sinus rhythm with no pathologic Q waves or ST-segment abnormalities. Echocardiogram shows normal left ventricular systolic function and no wall motion abnormalities.
Which of the following is the best recommendation for this patient before surgery?
A)Continue aspirin, discontinue prasugrel
B)Continue both antiplatelet medications
C)Continue prasugrel, discontinue aspirin
D)Hold both antiplatelet medications
E)Postpone surgery

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
79
A 30-year-old woman comes to the physician complaining of headaches, blurry vision, and fatigue. She can walk only 3-4 blocks before becoming tired and developing cramps in her legs. She does not use alcohol or tobacco.
Her blood pressure is 188/105 mm Hg and pulse is 78/min. Funduscopic examination reveals retinal hemorrhages. A continuous murmur is heard at the left and right sides of the anterior chest. Lungs are clear. No abdominal masses are palpated. Femoral pulses are faint bilaterally.
Laboratory results are as follows:
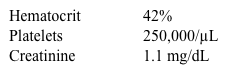
Which of the following is the most likely associated feature in this patient?
A)Cleft palate
B)Epicanthic folds
C)Short forearms and thumbs
D)Short stature
E)Spina bifida
Her blood pressure is 188/105 mm Hg and pulse is 78/min. Funduscopic examination reveals retinal hemorrhages. A continuous murmur is heard at the left and right sides of the anterior chest. Lungs are clear. No abdominal masses are palpated. Femoral pulses are faint bilaterally.
Laboratory results are as follows:
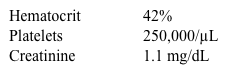
Which of the following is the most likely associated feature in this patient?
A)Cleft palate
B)Epicanthic folds
C)Short forearms and thumbs
D)Short stature
E)Spina bifida

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck
80
An 84-year-old woman comes to the office to follow up on multiple chronic medical conditions. She has intermittent dizziness and has recently fallen twice, although she was not injured. During the most recent episode, the patient was standing in the living room when she felt lightheaded and slipped backward onto a chair. She did not lose consciousness or experience involuntary movements. Medical history is notable for hypertension, type 2 diabetes mellitus, severe osteoporosis, coronary artery disease, and chronic renal disease. Current medications include hydrochlorothiazide, low-dose metformin, vitamin D, and metoprolol, and she has taken alendronate for the past 4 years.
Supine blood pressure is 129/75 mm Hg, pulse is 66/min, and respirations are 16/min. Physical examination shows a grade 2/6 midsystolic murmur at the right second intercostal area, moderately severe thoracic kyphosis, and decreased pulses bilaterally in the feet. The remainder of the examination is normal.
Laboratory results are as follows:
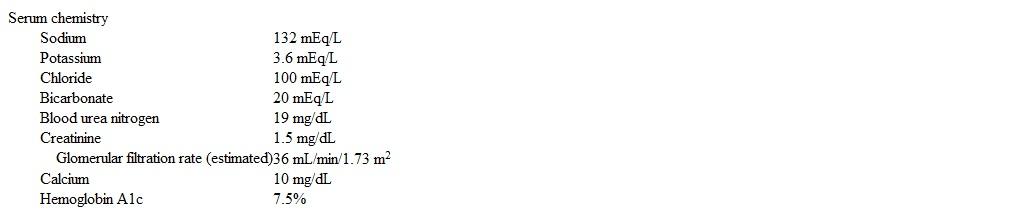 Complete blood count is within normal limits.
Complete blood count is within normal limits.
Which of the following is the most appropriate next step in management of this patient?
A)Add amlodipine
B)Add sitagliptin
C)Stop alendronate
D)Stop hydrochlorothiazide
E)Stop metformin and start glipizide
Supine blood pressure is 129/75 mm Hg, pulse is 66/min, and respirations are 16/min. Physical examination shows a grade 2/6 midsystolic murmur at the right second intercostal area, moderately severe thoracic kyphosis, and decreased pulses bilaterally in the feet. The remainder of the examination is normal.
Laboratory results are as follows:
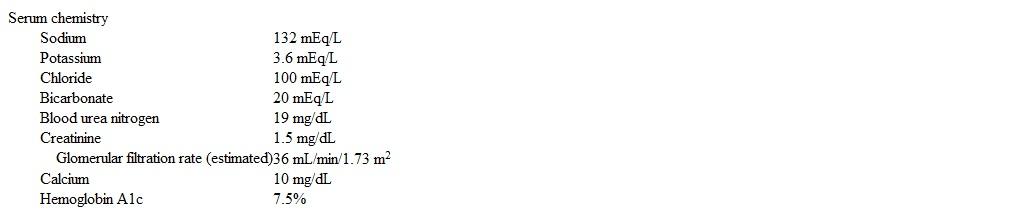 Complete blood count is within normal limits.
Complete blood count is within normal limits.Which of the following is the most appropriate next step in management of this patient?
A)Add amlodipine
B)Add sitagliptin
C)Stop alendronate
D)Stop hydrochlorothiazide
E)Stop metformin and start glipizide

Unlock Deck
Unlock for access to all 900 flashcards in this deck.
Unlock Deck
k this deck



