Deck 2: Pediatric
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question

Unlock Deck
Sign up to unlock the cards in this deck!
Unlock Deck
Unlock Deck
1/723
Play
Full screen (f)
Deck 2: Pediatric
1
A 4-month-old boy is brought to the office due to abnormal twisting movements of the limbs and torso. The patient also is not able to push up on his arms when prone. He was born at full term to a 30-year-old woman by forceps-assisted vaginal delivery. The delivery was complicated by cephalohematoma. The patient has not been evaluated since discharge at age 2 days. Vital signs are normal. Weight and length are at the 50th percentile for age. His eyes are crossed, and he does not react to sound. Dystonic extremities are noted on examination. Which of the following is the most likely explanation for this patient's current condition?
A)Autoimmune injury to basal ganglia
B)Bilirubin-induced neurotoxicity
C)MECP2 gene mutation
D)Physiologic chorea of infancy
E)Trinucleotide repeat expansion on chromosome 4p
A)Autoimmune injury to basal ganglia
B)Bilirubin-induced neurotoxicity
C)MECP2 gene mutation
D)Physiologic chorea of infancy
E)Trinucleotide repeat expansion on chromosome 4p
B
Explanation:
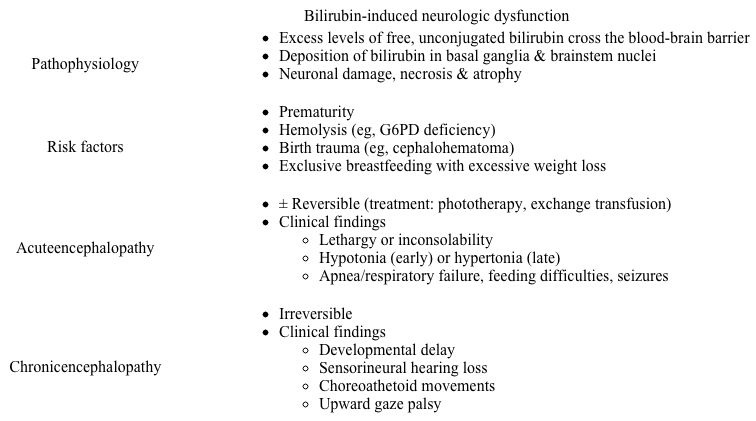
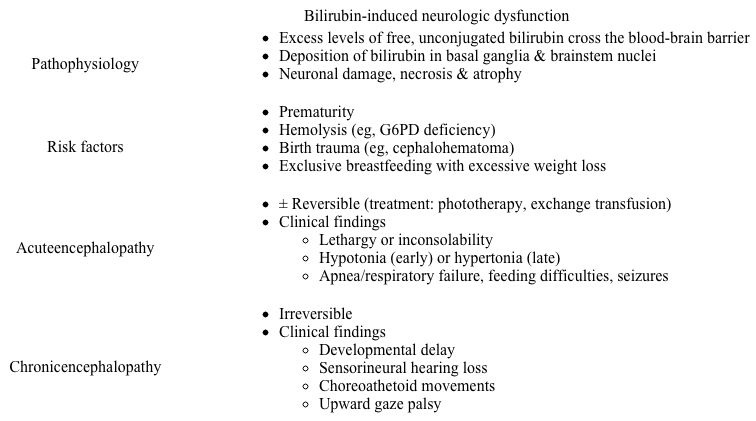 This infant who was not evaluated beyond the immediate newborn period now has dystonic movements (ie, involuntary twisting/writhing), a finding concerning for bilirubin-induced neurologic dysfunction (BIND). BIND occurs when bilirubin concentration dramatically rises (total bilirubin ≥30 mg/dL) and exceeds the binding capacity of albumin. Unbound bilirubin crosses the blood-brain barrier and deposits in the basal ganglia and brainstem nuclei (eg, oculomotor, auditory), causing neuronal damage.
This infant who was not evaluated beyond the immediate newborn period now has dystonic movements (ie, involuntary twisting/writhing), a finding concerning for bilirubin-induced neurologic dysfunction (BIND). BIND occurs when bilirubin concentration dramatically rises (total bilirubin ≥30 mg/dL) and exceeds the binding capacity of albumin. Unbound bilirubin crosses the blood-brain barrier and deposits in the basal ganglia and brainstem nuclei (eg, oculomotor, auditory), causing neuronal damage.
Although many patients have no known risk factors, the cephalohematoma this patient sustained during delivery likely led to localized red blood cell breakdown that caused unconjugated hyperbilirubinemia.
cephalohematoma
Acute BIND typically presents with lethargy; tone abnormalities; and high-pitched, inconsolable crying. However, symptoms may be subtle or overlooked.
Prolonged, unrecognized or untreated hyperbilirubinemia can lead to chronic BIND (ie, kernicterus), typically presenting after early infancy with irreversible neurologic damage. Common manifestations include hyperkinetic movements (eg, choreoathetosis, dystonia), sensorineural hearing loss, and abnormal eye movements (eg, upward gaze palsy). Developmental delay (eg, inability to push up when prone at age 4 months) is also typical.
Serial examinations and/or bilirubin monitoring in the early neonatal period, particularly in patients with risk factors, as well as early treatment of hyperbilirubinemia (eg, phototherapy) can help prevent BIND.
(Choice A) Autoimmune injury to the basal ganglia describes Sydenham chorea, a manifestation of acute rheumatic fever (ARF). This complication of an untreated Streptococcus pyogenes infection typically presents at age 5-15, not in infancy. None of the other ARF findings (eg, fever, rash, arthritis) is present in this case, and the patient's hearing loss and gaze abnormality are inconsistent with the diagnosis.
(Choice C) MECP2 gene mutation causes Rett syndrome, a disorder characterized by speech regression, abnormal gait, and loss of purposeful hand movements (eg, repetitive hand wringing). It also is a condition that affects girls, and neurologic degeneration begins after age 6 months.
(Choice D) Physiologic chorea of infancy refers to benign, chorea-like movements in normal newborns. It resolves by age 8 months. Neither hearing loss nor gaze abnormalities are seen.
(Choice E) Huntington disease, caused by a trinucleotide repeat expansion on chromosome 4p, typically presents in adulthood with chorea (ie, involuntary, jerky movements) and progressive dementia. This patient's age excludes the diagnosis.
Educational objective:
Bilirubin-induced neurologic dysfunction is due to extreme unconjugated bilirubinemia in which unbound bilirubin crosses the blood-brain barrier. Chronic disease (ie, kernicterus) results in hyperkinetic movements (eg, chorea, dystonia), sensorineural hearing loss, and gaze abnormalities.
References:
Clinicopathological spectrum of bilirubin encephalopathy/kernicterus.
(http://www.ncbi.nlm.nih.gov/pubmed/30823396)
Explanation:
 This infant who was not evaluated beyond the immediate newborn period now has dystonic movements (ie, involuntary twisting/writhing), a finding concerning for bilirubin-induced neurologic dysfunction (BIND). BIND occurs when bilirubin concentration dramatically rises (total bilirubin ≥30 mg/dL) and exceeds the binding capacity of albumin. Unbound bilirubin crosses the blood-brain barrier and deposits in the basal ganglia and brainstem nuclei (eg, oculomotor, auditory), causing neuronal damage.
This infant who was not evaluated beyond the immediate newborn period now has dystonic movements (ie, involuntary twisting/writhing), a finding concerning for bilirubin-induced neurologic dysfunction (BIND). BIND occurs when bilirubin concentration dramatically rises (total bilirubin ≥30 mg/dL) and exceeds the binding capacity of albumin. Unbound bilirubin crosses the blood-brain barrier and deposits in the basal ganglia and brainstem nuclei (eg, oculomotor, auditory), causing neuronal damage.Although many patients have no known risk factors, the cephalohematoma this patient sustained during delivery likely led to localized red blood cell breakdown that caused unconjugated hyperbilirubinemia.
cephalohematoma
Acute BIND typically presents with lethargy; tone abnormalities; and high-pitched, inconsolable crying. However, symptoms may be subtle or overlooked.
Prolonged, unrecognized or untreated hyperbilirubinemia can lead to chronic BIND (ie, kernicterus), typically presenting after early infancy with irreversible neurologic damage. Common manifestations include hyperkinetic movements (eg, choreoathetosis, dystonia), sensorineural hearing loss, and abnormal eye movements (eg, upward gaze palsy). Developmental delay (eg, inability to push up when prone at age 4 months) is also typical.
Serial examinations and/or bilirubin monitoring in the early neonatal period, particularly in patients with risk factors, as well as early treatment of hyperbilirubinemia (eg, phototherapy) can help prevent BIND.
(Choice A) Autoimmune injury to the basal ganglia describes Sydenham chorea, a manifestation of acute rheumatic fever (ARF). This complication of an untreated Streptococcus pyogenes infection typically presents at age 5-15, not in infancy. None of the other ARF findings (eg, fever, rash, arthritis) is present in this case, and the patient's hearing loss and gaze abnormality are inconsistent with the diagnosis.
(Choice C) MECP2 gene mutation causes Rett syndrome, a disorder characterized by speech regression, abnormal gait, and loss of purposeful hand movements (eg, repetitive hand wringing). It also is a condition that affects girls, and neurologic degeneration begins after age 6 months.
(Choice D) Physiologic chorea of infancy refers to benign, chorea-like movements in normal newborns. It resolves by age 8 months. Neither hearing loss nor gaze abnormalities are seen.
(Choice E) Huntington disease, caused by a trinucleotide repeat expansion on chromosome 4p, typically presents in adulthood with chorea (ie, involuntary, jerky movements) and progressive dementia. This patient's age excludes the diagnosis.
Educational objective:
Bilirubin-induced neurologic dysfunction is due to extreme unconjugated bilirubinemia in which unbound bilirubin crosses the blood-brain barrier. Chronic disease (ie, kernicterus) results in hyperkinetic movements (eg, chorea, dystonia), sensorineural hearing loss, and gaze abnormalities.
References:
Clinicopathological spectrum of bilirubin encephalopathy/kernicterus.
(http://www.ncbi.nlm.nih.gov/pubmed/30823396)
2
A 65-year-old woman comes to the office due to deteriorating memory. She used to pride herself on her sharp memory and is very concerned about its loss, saying, "Over the last 6 months I have been forgetting the most trivial things." The patient has had to delegate tasks such as household chores and cooking to her husband because of her poor memory and "cloudy thinking." "I have been feeling useless and worthless since retiring last year. Now I just watch TV all day and barely have enough energy to eat. I haven't felt like gardening in over a year-I used to love it!" Both the patient's mother and father died of complications of Alzheimer disease. She's lost 5 kg (11 lb) over the last 2 months but her physical examination is within normal limits. On testing with the Montreal Cognitive Assessment, she scores 24/30 (normal ≥26) with deficits in delayed recall and attention. Laboratory results, including thyroid function, are unremarkable. MRI of the head is normal. Which of the following is the best next step in management of this patient?
A)Reassure patient that these are expected age-related memory changes
B)Recommend memory training and vitamin E
C)Start amantadine pharmacotherapy
D)Start donepezil pharmacotherapy
E)Start escitalopram pharmacotherapy
F)Start memantine pharmacotherapy
A)Reassure patient that these are expected age-related memory changes
B)Recommend memory training and vitamin E
C)Start amantadine pharmacotherapy
D)Start donepezil pharmacotherapy
E)Start escitalopram pharmacotherapy
F)Start memantine pharmacotherapy
E
Explanation:
This patient exhibits features of major depressive disorder (eg, anhedonia, feelings of worthlessness, weight loss, low energy, impaired ability to think) accompanied by memory impairment. Her worsening depressive symptoms over the past year are notable for predating the onset of memory difficulties 6 months ago. Severe depression, especially in older adults, may present with cognitive impairment severe enough to mimic dementia, a condition known as depression-related cognitive impairment (sometimes referred to as pseudodementia). During cognitive testing, patients with this condition typically exhibit deficits in attention, concentration, memory, and executive function. They may have difficulty completing testing and frequently put forth poor effort.
major depressive disorder
Depression-related cognitive impairment is largely reversible with the treatment of the underlying depression using medications such as selective serotonin reuptake inhibitors (eg, escitalopram) and/or psychotherapy. As the patient's depression improves, cognitive impairment (and Montreal Cognitive Assessment score) should return to premorbid baseline.
(Choice A) This patient's symptoms are not explained by normal age-related memory impairment, and her depression requires definitive treatment with antidepressant medication and/or psychotherapy.
(Choice B) Memory training involves using mnemonic techniques, external cues, and organizational aids to assist patients with mild cognitive impairment. Vitamin E has limited evidence for the treatment of mild-to-moderate Alzheimer disease but has no evidence for the treatment of depression-related cognitive impairment. This patient's major depressive episode requires appropriate treatment with antidepressant medication and/or psychotherapy.
(Choice C) Amantadine is a drug that may be used in the treatment of Parkinson disease.
(Choices D and F) Cholinesterase inhibitors (eg, donepezil) and the NMDA receptor antagonist memantine are used in the treatment of dementia (eg, Alzheimer disease) but have not been shown to be helpful for depression-related cognitive impairment. This patient's cognitive symptoms should improve with treatment of her underlying depression.
Educational objective:
Depression-related cognitive impairment may be so severe in elderly patients that they appear to have dementia. Psychotherapy and/or antidepressant medications are the treatment of choice for elderly patients with depression and frequently result in reversal of cognitive deficits.
References:
Depression and cognition in the elderly.
(http://www.ncbi.nlm.nih.gov/pubmed/25581234)
Diagnosis and treatment of depression and cognitive impairment in late life.
(http://www.ncbi.nlm.nih.gov/pubmed/25655026)
Explanation:
This patient exhibits features of major depressive disorder (eg, anhedonia, feelings of worthlessness, weight loss, low energy, impaired ability to think) accompanied by memory impairment. Her worsening depressive symptoms over the past year are notable for predating the onset of memory difficulties 6 months ago. Severe depression, especially in older adults, may present with cognitive impairment severe enough to mimic dementia, a condition known as depression-related cognitive impairment (sometimes referred to as pseudodementia). During cognitive testing, patients with this condition typically exhibit deficits in attention, concentration, memory, and executive function. They may have difficulty completing testing and frequently put forth poor effort.
major depressive disorder
Depression-related cognitive impairment is largely reversible with the treatment of the underlying depression using medications such as selective serotonin reuptake inhibitors (eg, escitalopram) and/or psychotherapy. As the patient's depression improves, cognitive impairment (and Montreal Cognitive Assessment score) should return to premorbid baseline.
(Choice A) This patient's symptoms are not explained by normal age-related memory impairment, and her depression requires definitive treatment with antidepressant medication and/or psychotherapy.
(Choice B) Memory training involves using mnemonic techniques, external cues, and organizational aids to assist patients with mild cognitive impairment. Vitamin E has limited evidence for the treatment of mild-to-moderate Alzheimer disease but has no evidence for the treatment of depression-related cognitive impairment. This patient's major depressive episode requires appropriate treatment with antidepressant medication and/or psychotherapy.
(Choice C) Amantadine is a drug that may be used in the treatment of Parkinson disease.
(Choices D and F) Cholinesterase inhibitors (eg, donepezil) and the NMDA receptor antagonist memantine are used in the treatment of dementia (eg, Alzheimer disease) but have not been shown to be helpful for depression-related cognitive impairment. This patient's cognitive symptoms should improve with treatment of her underlying depression.
Educational objective:
Depression-related cognitive impairment may be so severe in elderly patients that they appear to have dementia. Psychotherapy and/or antidepressant medications are the treatment of choice for elderly patients with depression and frequently result in reversal of cognitive deficits.
References:
Depression and cognition in the elderly.
(http://www.ncbi.nlm.nih.gov/pubmed/25581234)
Diagnosis and treatment of depression and cognitive impairment in late life.
(http://www.ncbi.nlm.nih.gov/pubmed/25655026)
3
A 24-year-old woman is brought to the emergency department 30 minutes after a seizure. The patient had an uncomplicated spontaneous vaginal delivery 10 days ago and was discharged from the hospital 2 days after delivery. She has had worsening headache for the past several days, which is most severe upon awakening in the morning and is associated with vomiting. Today, she experienced a brief generalized tonic-clonic seizure that was witnessed by her husband. She has no history of seizure disorder or other medical conditions. Family history is significant for recurrent deep venous thrombosis in her mother. Temperature is 37.1 C (98.7 F), blood pressure is 105/70 mm Hg, and pulse is 90/min. On physical examination, the patient is somnolent but arouses to voice and follows instructions. Pupils are normal but there is bilateral papilledema. There is no focal weakness or sensory loss. There is no neck stiffness. A noncontrast CT scan of the head reveals no intracranial hemorrhage or mass lesions. Blood cell counts, serum electrolytes, and liver function studies are within normal limits. Urinalysis is normal. Which of the following is the best next step in management of this patient?
A)Administer thrombolytics
B)Begin magnesium sulfate
C)Obtain head MR venography
D)Order cerebral angiography
A)Administer thrombolytics
B)Begin magnesium sulfate
C)Obtain head MR venography
D)Order cerebral angiography
C
Explanation:
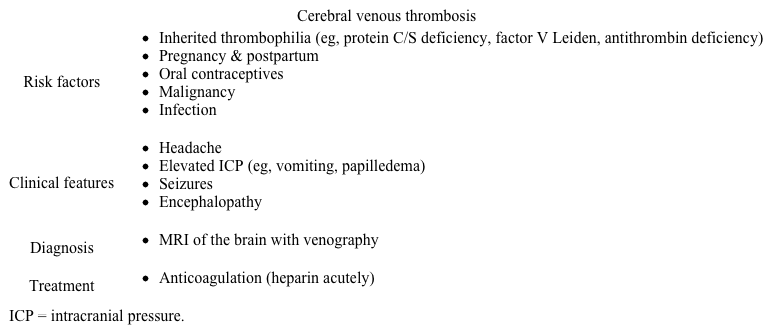
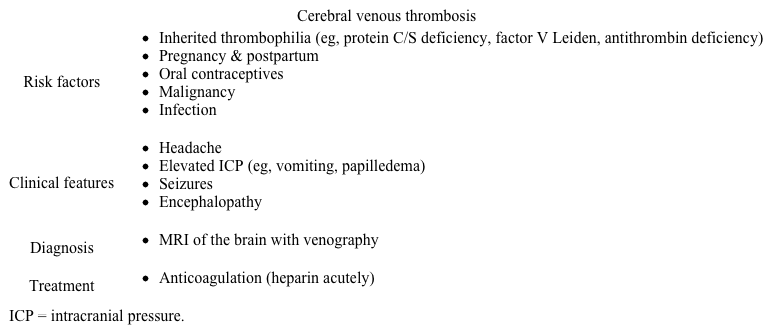 This patient most likely has a cerebral venous thrombosis (CVT), a rare, potentially life-threatening condition due to blood clot formation within the dural sinuses. Most cases are related to a prothrombotic state, including pregnancy and the postpartum period as well as inherited thrombophilias (eg, family history of recurrent deep venous thrombosis).
This patient most likely has a cerebral venous thrombosis (CVT), a rare, potentially life-threatening condition due to blood clot formation within the dural sinuses. Most cases are related to a prothrombotic state, including pregnancy and the postpartum period as well as inherited thrombophilias (eg, family history of recurrent deep venous thrombosis).
As the thrombus progressively enlarges and obstructs dural venous drainage from the brain, patients develop venous congestion, decreased cerebral perfusion, and disruption of the blood-brain barrier. In addition, patients can develop impaired cerebrospinal fluid (CSF) resorption and subsequent elevated intracranial pressure (ICP), which can present with headache exacerbated by recumbency (eg, worse in the morning), vomiting, papilledema, and seizures. As ICP increases, patients can develop ischemic (due to decreased perfusion) and/or hemorrhagic (due to thin-walled venous vessel rupture) stroke, which does not follow typical arterial patterns.
Initial evaluation of patients with seizure and suspected stroke is with a CT scan of the head, which can be normal in approximately one-third of patients with CVT. In those with high clinical suspicion and a normal head CT scan (as in this patient), the best next step is an MR venography of the brain, which can better visualize flow deficit in the venous sinuses. Treatment involves anticoagulation; the type is dependent on patient-specific factors (eg, pregnancy, breastfeeding status).
(Choice A) Thrombolytics are used in ischemic stroke but are not typically used for CVT because of concern for worsening the intracerebral hemorrhage which can occur due to rupture of blood vessels.
(Choice B) Magnesium sulfate is used to prevent seizure recurrence in patients with eclampsia. Eclampsia can occur up to 6 weeks postpartum and can present with headache, seizures, and stroke. However, this patient's normal blood pressure for pregnancy (<140/90 mm Hg) and lack of proteinuria make this diagnosis less likely.
(Choice D) Cerebral angiography of the brain can also be diagnostic of CVST. However, because it is more invasive and carries a risk of significant complications, it is typically done only if MR venography is equivocal.
Educational objective:
Cerebral venous sinus thrombosis typically presents in prothrombotic conditions (eg, postpartum) with headache, increased intracranial pressure, seizures, and stroke. Diagnosis is confirmed by visualizing a flow void on MR venography of the brain.
Explanation:
 This patient most likely has a cerebral venous thrombosis (CVT), a rare, potentially life-threatening condition due to blood clot formation within the dural sinuses. Most cases are related to a prothrombotic state, including pregnancy and the postpartum period as well as inherited thrombophilias (eg, family history of recurrent deep venous thrombosis).
This patient most likely has a cerebral venous thrombosis (CVT), a rare, potentially life-threatening condition due to blood clot formation within the dural sinuses. Most cases are related to a prothrombotic state, including pregnancy and the postpartum period as well as inherited thrombophilias (eg, family history of recurrent deep venous thrombosis).As the thrombus progressively enlarges and obstructs dural venous drainage from the brain, patients develop venous congestion, decreased cerebral perfusion, and disruption of the blood-brain barrier. In addition, patients can develop impaired cerebrospinal fluid (CSF) resorption and subsequent elevated intracranial pressure (ICP), which can present with headache exacerbated by recumbency (eg, worse in the morning), vomiting, papilledema, and seizures. As ICP increases, patients can develop ischemic (due to decreased perfusion) and/or hemorrhagic (due to thin-walled venous vessel rupture) stroke, which does not follow typical arterial patterns.
Initial evaluation of patients with seizure and suspected stroke is with a CT scan of the head, which can be normal in approximately one-third of patients with CVT. In those with high clinical suspicion and a normal head CT scan (as in this patient), the best next step is an MR venography of the brain, which can better visualize flow deficit in the venous sinuses. Treatment involves anticoagulation; the type is dependent on patient-specific factors (eg, pregnancy, breastfeeding status).
(Choice A) Thrombolytics are used in ischemic stroke but are not typically used for CVT because of concern for worsening the intracerebral hemorrhage which can occur due to rupture of blood vessels.
(Choice B) Magnesium sulfate is used to prevent seizure recurrence in patients with eclampsia. Eclampsia can occur up to 6 weeks postpartum and can present with headache, seizures, and stroke. However, this patient's normal blood pressure for pregnancy (<140/90 mm Hg) and lack of proteinuria make this diagnosis less likely.
(Choice D) Cerebral angiography of the brain can also be diagnostic of CVST. However, because it is more invasive and carries a risk of significant complications, it is typically done only if MR venography is equivocal.
Educational objective:
Cerebral venous sinus thrombosis typically presents in prothrombotic conditions (eg, postpartum) with headache, increased intracranial pressure, seizures, and stroke. Diagnosis is confirmed by visualizing a flow void on MR venography of the brain.
4
An 8-year-old girl is brought to the emergency department with lethargy and fever. The patient has had intermittent cough, fever, and headache for the past 3 weeks. She vomited before dinner last night and went to bed early. This morning, her father could not wake her up. The patient is otherwise healthy. She traveled with her family to rural Ecuador 2 months ago for a mission trip. She has no other recent travel and no known sick contacts. Temperature is 39.8 C (103.6 F). The patient is minimally responsive on examination. Funduscopy shows papilledema, and chest auscultation reveals decreased breath sounds and crackles over the right middle lobe. The results of lumbar puncture are as follows:  Which of the following organisms is the most likely cause of this patient's symptoms?
Which of the following organisms is the most likely cause of this patient's symptoms?
A)Aspergillus fumigatus
B)Enterovirus
C)Listeria monocytogenes
D)Mycobacterium tuberculosis
E)Streptococcus pneumoniae
F)Toxoplasma gondii
 Which of the following organisms is the most likely cause of this patient's symptoms?
Which of the following organisms is the most likely cause of this patient's symptoms?A)Aspergillus fumigatus
B)Enterovirus
C)Listeria monocytogenes
D)Mycobacterium tuberculosis
E)Streptococcus pneumoniae
F)Toxoplasma gondii

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
5
A 28-year-old woman comes to the office due to weakness. The patient, who is 8 weeks postpartum, reports intermittent weakness of the upper and lower extremities. She says, "My arms feel weak after carrying the baby for a few minutes, and I can't lift him until I rest for some time. Yesterday evening, I couldn't even get off of the toilet, but today, I feel fine." The patient has also had episodes of blurry vision. Her pregnancy was complicated by gestational diabetes, but she has no chronic medical conditions. The patient's only medication is a daily multivitamin. She does not use tobacco, alcohol, or illicit drugs. Blood pressure is 120/68 mm Hg and pulse is 74/min. Physical examination shows normal pupils and extraocular movements. Jugular venous pressure is not elevated, and chest auscultation reveals no abnormalities. There is no extremity edema. Deep tendon reflexes and muscle strength of the bilateral upper and lower extremities are normal. Which of the following is the most likely diagnosis?
A)Diabetic amyotrophy
B)Multiple sclerosis
C)Myasthenia gravis
D)Myotonic dystrophy
E)Polymyositis
F)Postpartum thyroiditis
A)Diabetic amyotrophy
B)Multiple sclerosis
C)Myasthenia gravis
D)Myotonic dystrophy
E)Polymyositis
F)Postpartum thyroiditis

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
6
A 37-year-old woman comes to the office due to frequent tearfulness. The patient describes herself as "a happy person" at baseline but says that "about 6 months ago, I began to have more sad days than happy days." She frequently goes a week without leaving home and has to force herself to eat and clean. The patient's father committed suicide at age 41, and her paternal grandfather is said to have died of a "mental disease" at age 49. The patient tearfully admits to thoughts of suicide but has no plans or intent. Temperature is 36.9 C (98.4 F), blood pressure is 121/77 mm Hg, pulse is 68/min, and respirations are 14/min. The patient has no subjective memory issues. She scores 25/30 on the Montreal Cognitive Assessment (normal: ≥26), losing points on measures of executive function. She appears restless during the examination, shifting frequently in her chair. The patient repeatedly raises her right arm in an abrupt, twisting motion that ends with smoothing her hair. Extraocular movement testing shows delayed initiation of voluntary saccades. Deep tendon reflexes are 3+ in both upper and lower extremities. The patient's disease is primarily associated with degeneration of which of the following neuronal cell groups?
A)Dopamine
B)Endorphin
C)GABA
D)Glutamate
E)Histamine
F)Norepinephrine
G)Serotonin
A)Dopamine
B)Endorphin
C)GABA
D)Glutamate
E)Histamine
F)Norepinephrine
G)Serotonin

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
7
An 18-year-old woman comes to the office due to recurrent headaches. In the past, the patient has had occasional headaches, especially during term exams or other stressful situations. However, over the past 3 months, she has had 4 episodes of severe headache. They are always left sided, throbbing, associated with nausea, and spontaneously resolve after 12-24 hours. The patient also reports feelings of numbness and tingling in her extremities prior to the headaches. She has no chronic medical conditions and underwent an appendectomy several years ago. The patient is sexually active with her boyfriend and began taking combined oral contraceptives 6 months ago. Vital signs are within normal limits. Physical examination, including neurological examination, shows no abnormalities. Which of the following is the best next step in management of this patient?
A)Begin selective serotonin reuptake inhibitor
B)Discontinue oral contraceptives
C)Measure cerebrospinal fluid pressure
D)Order MRI of the brain
E)Prescribe daily propranolol therapy
F)Reassure and advise nonsteroidal anti-inflammatory drugs as needed
A)Begin selective serotonin reuptake inhibitor
B)Discontinue oral contraceptives
C)Measure cerebrospinal fluid pressure
D)Order MRI of the brain
E)Prescribe daily propranolol therapy
F)Reassure and advise nonsteroidal anti-inflammatory drugs as needed

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
8
A 60-year-old man is brought to the office due to a 2-week history of involuntary muscle spasms in his arms, especially when he is startled. Over the past 2 months, the patient has experienced worsening insomnia and confusion and gotten lost in his surroundings. He has no fever, headache, or urinary symptoms. Temperature is 37.1 C (98.8 F), blood pressure is 130/76 mm Hg, and pulse is 82/min. The patient is alert but poorly groomed. Examination is notable for frequent irregular jerks of the upper and lower extremities, increased muscle tone, brisk deep tendon reflexes, and bilateral extensor plantar responses. On cognitive testing, the patient recalls 0 of 3 delayed recall items and is unable to draw a clock. A noncontrast head CT scan is normal. Electroencephalography reveals periodic sharp-wave complexes. Which of the following is the most likely outcome for this patient?
A)Death within a year regardless of therapy
B)Rapid symptomatic improvement with pharmacotherapy
C)Rapid symptomatic improvement with surgery
D)Slow symptomatic progression despite pharmacotherapy
E)Slow symptomatic resolution with pharmacotherapy
A)Death within a year regardless of therapy
B)Rapid symptomatic improvement with pharmacotherapy
C)Rapid symptomatic improvement with surgery
D)Slow symptomatic progression despite pharmacotherapy
E)Slow symptomatic resolution with pharmacotherapy

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
9
An 11-year-old girl is brought to the emergency department for visual disturbances. Two hours ago, the patient saw flashing lights followed by spots of vision loss. These symptoms fully resolved within 30 minutes. Since then, a bifrontal, throbbing headache and nausea have developed. The patient has had no fever, eye pain, or head trauma. She has had two similar headaches in the last 6 months. Temperature is 37.2 C (99 F), blood pressure is 102/68 mm Hg, and pulse is 88/min. On examination, the patient is alert and appears in moderate discomfort with her eyes closed. Extraocular movements are intact. Funduscopic examination is normal, and pupils are equal and reactive to light, but the patient is uncomfortable during assessment due to the light. Cardiovascular, respiratory, abdominal, and neurologic examinations are normal. Which of the following is the best next step in management of this patient?
A)CT scan of the brain
B)Intraocular pressure measurement
C)Lumbar puncture
D)Nonsteroidal anti-inflammatory drug only
E)Visual field testing
A)CT scan of the brain
B)Intraocular pressure measurement
C)Lumbar puncture
D)Nonsteroidal anti-inflammatory drug only
E)Visual field testing

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
10
A 67-year-old retired college professor comes to the office for evaluation of memory loss. The patient has had intermittent episodes of misplacing objects and forgetting appointments. He also reports difficulty concentrating. The patient performs most activities of daily living independently. He has a history of well-controlled hypertension. Family history is significant for dementia in his mother. Vital signs are within normal limits. Mini-Mental State Examination is administered to screen for cognitive impairment. Which of the following factors may limit validity of the screening tool in this patient?
A)Early attention span impairment
B)Family history of dementia
C)Higher level of education
D)Patient's age
E)Preserved activities of daily living
A)Early attention span impairment
B)Family history of dementia
C)Higher level of education
D)Patient's age
E)Preserved activities of daily living

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
11
A 6-month-old girl is brought to the physician for evaluation of irritability and listlessness. Her parents are concerned that the child cannot sit or roll even though she was able to do so several weeks before. The child was previously healthy except for 2 prior respiratory infections. On examination, the patient is hypotonic with hepatosplenomegaly and a protuberant abdomen. She has a bright red macula on ophthalmologic examination along with cervical lymphadenopathy. All deep-tendon reflexes are diminished. Which of the following is the most likely cause of this child's developmental regression?
A)β-hexosaminidase A deficiency
B)Galactocerebrosidase deficiency
C)Glucocerebrosidase deficiency
D)Lysosomal hydrolase deficiency
E)Sphingomyelinase deficiency
A)β-hexosaminidase A deficiency
B)Galactocerebrosidase deficiency
C)Glucocerebrosidase deficiency
D)Lysosomal hydrolase deficiency
E)Sphingomyelinase deficiency

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
12
A 63-year-old man is brought to the office by his daughter due to recurrent falls. According to his daughter, the patient has lost his balance and fallen several times over the past 6 months. He has not sustained serious injuries. She has also noticed some "shaking" of his right hand that is most apparent at rest. The patient has lived alone since his wife died 5 years ago and still shops, cooks, and cleans independently. Blood pressure is 141/68 mm Hg and pulse is 72/min. Neurologic examination shows mild rigidity of the limb muscles that is most prominent on the right side with a slow, shuffling gait. The patient is prescribed medication for his symptoms but returns to the office 4 weeks later reporting "disturbing visions of strangers creeping around corners of his apartment." On examination, he is alert and scores 27/30 on the Montreal Cognitive Assessment (normal: ≥26). Which of the following is the most likely explanation for this patient's new symptoms?
A)COMT inhibitor pharmacotherapy
B)Dementia with Lewy bodies
C)Dopamine agonist pharmacotherapy
D)Frontotemporal dementia
E)MAO-B inhibitor pharmacotherapy
A)COMT inhibitor pharmacotherapy
B)Dementia with Lewy bodies
C)Dopamine agonist pharmacotherapy
D)Frontotemporal dementia
E)MAO-B inhibitor pharmacotherapy

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
13
A 7-year-old boy is brought to the office due to urinary dribbling for the past 2 months. Symptoms occur during the day as well as overnight. Review of systems is positive for chronic constipation. He has no other chronic medical problems and takes no medications. Temperature is 37.2 C (99 F), blood pressure is 100/60 mm Hg, pulse is 80/min, and respirations are 16/min. Growth parameters are normal. Physical examination shows a tuft of hair above the gluteal cleft and is otherwise normal. Urinalysis is normal. Which is the most appropriate next step in management of this patient?
A)Abdominal ultrasound
B)Abdominal x-ray
C)Measurement of 24-hour urine volume
D)MRI of the spine
E)Reassurance and laxatives
A)Abdominal ultrasound
B)Abdominal x-ray
C)Measurement of 24-hour urine volume
D)MRI of the spine
E)Reassurance and laxatives

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
14
A 5-year-old boy is brought to the office by his parents due to behavioral difficulties. The patient just started kindergarten and has had difficulty staying focused on tasks and switching between activities. The teachers say that he is disruptive and often flaps and waves his hands. He was previously in a small preschool classroom with one-on-one teaching and was able to complete most activities with help. The patient's developmental history is notable for speaking his first word at age 19 months and walking at age 20 months. His mother also had learning difficulties, but she was able to graduate from high school with tutoring. Height and weight are at the 50th percentile, and head circumference is at the 90th percentile. Examination shows a prominent forehead and chin. Mild hypotonia and joint hypermobility are present in bilateral lower extremities. Which of the following is the most likely prognosis for this patient's condition?
A)Early death from respiratory muscle weakness
B)Increased morbidity and mortality from aortic root disease
C)Increased risk for dementia and early death
D)Normal life expectancy
E)Shorter life expectancy from progressive brain deceleration
A)Early death from respiratory muscle weakness
B)Increased morbidity and mortality from aortic root disease
C)Increased risk for dementia and early death
D)Normal life expectancy
E)Shorter life expectancy from progressive brain deceleration

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
15
A 38-year-old woman with multiple sclerosis comes to the office due to insomnia for the past several weeks. The patient also reports episodes of an uncomfortable "tingly" sensation in her legs associated with an urge to stretch her legs or move around. The symptoms are worse when she is lying in bed at night or when watching television or working at her computer. The patient began taking over-the-counter antihistamines to help her sleep but states she wakes up a few hours later with worsening symptoms. She feels exhausted and foggy-headed during the day. The patient is taking a stable-dose disease-modifying treatment for multiple sclerosis, and her most recent exacerbation was 2 years ago. She has no other medical conditions. Physical examination shows mildly increased lower extremity reflexes but normal muscle strength and sensations. Which of the following is the most appropriate pharmacotherapy for this patient's current symptoms?
A)Baclofen
B)Clonazepam
C)Duloxetine
D)Fluoxetine
E)Pramipexole
A)Baclofen
B)Clonazepam
C)Duloxetine
D)Fluoxetine
E)Pramipexole

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
16
A 66-year-old woman is brought to the emergency department by her son due to increasing confusion, loss of mobility, and behavioral changes. The patient cries out for no apparent reason and recently exclaimed that "a lion was sleeping in the backyard." She often sees cats in her room when none are present. She has had memory loss and frequently gets lost in her neighborhood. The patient is afebrile; blood pressure is 136/72 mm Hg, pulse is 98/min, and respirations are 16/min. On physical examination, she is alert but disoriented and quite agitated. Physical examination shows increased muscle tone, normal reflexes, and coarse resting tremors in the extremities. Which of the following is most closely associated with this patient's current condition?
A)Concurrent atherosclerotic cardiovascular disease
B)Increased sensitivity to antipsychotic drugs
C)Predisposition to respiratory muscle weakness
D)Predominant atrophy of frontotemporal lobes
E)Rapid response to high-volume lumbar puncture
F)Vertical supranuclear gaze palsy
A)Concurrent atherosclerotic cardiovascular disease
B)Increased sensitivity to antipsychotic drugs
C)Predisposition to respiratory muscle weakness
D)Predominant atrophy of frontotemporal lobes
E)Rapid response to high-volume lumbar puncture
F)Vertical supranuclear gaze palsy

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
17
An 18-year-old man is evaluated due to worsening headaches. For the last several months, the patient has had intermittent, dull, occipital headaches, which are often brought on by physical activity, cough, or straining. The pain is usually accompanied by nausea and dizziness, and the symptoms spontaneously resolve after several minutes. There is no history of fever, chills, photophobia, vision disturbances, or focal weakness or numbness. He has no prior medical conditions and takes no medications. Vital signs are normal. Physical examination, including neurologic examination, shows no abnormalities. MRI of the head is shown in the image below: 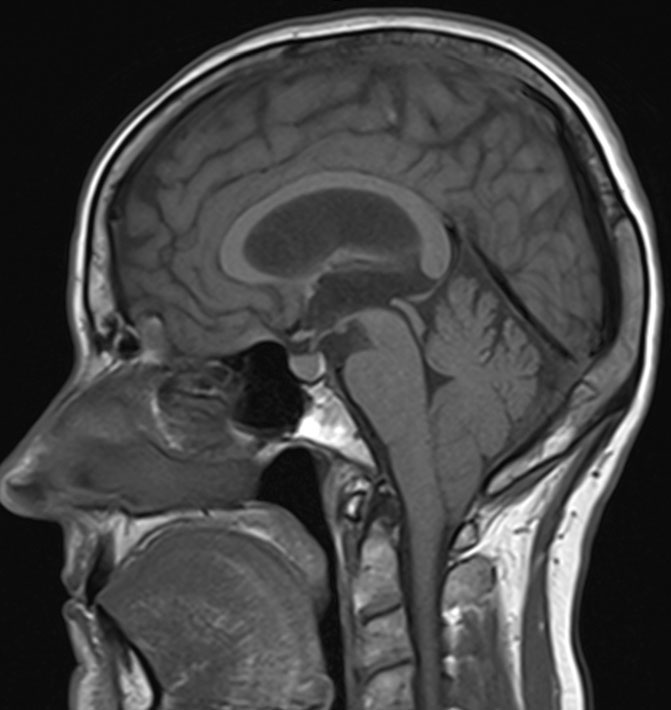 This patient is at greatest risk for which of the following in association with his current condition?
This patient is at greatest risk for which of the following in association with his current condition?
A)Cardiac rhabdomyoma
B)Optic neuritis
C)Parathyroid adenoma
D)Syringomyelia
E)Vestibular schwannoma
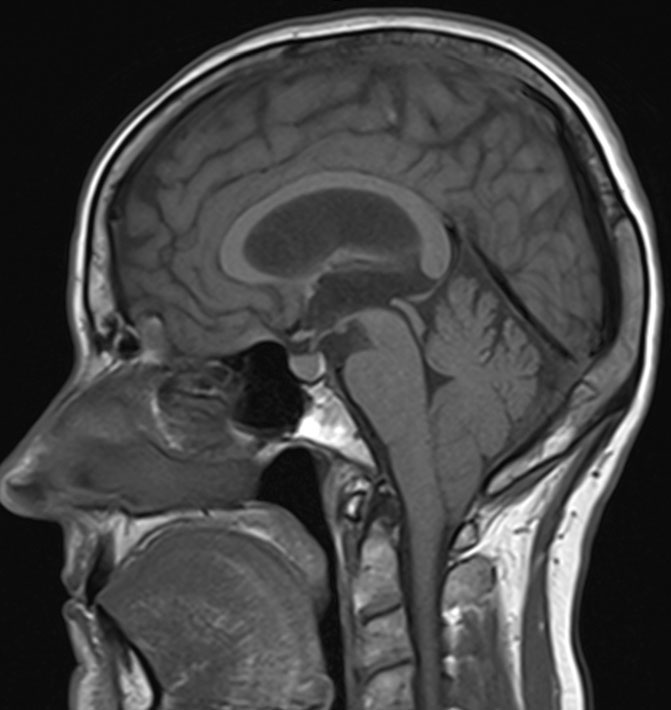 This patient is at greatest risk for which of the following in association with his current condition?
This patient is at greatest risk for which of the following in association with his current condition?A)Cardiac rhabdomyoma
B)Optic neuritis
C)Parathyroid adenoma
D)Syringomyelia
E)Vestibular schwannoma

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
18
A 52-year-old man is evaluated for ongoing cognitive difficulties. For the past 2 months, he has been sleeping 12-16 hours daily, much more than he usually does. When he is awake, he is withdrawn and less socially engaged than normal. During this time, the patient has had trouble driving, sideswiping cars on the right side of the road more than once. He also has had several falls, which he attributes to feeling off-balance. Vital signs are normal. The patient scores 22/30 (normal: ≥26) on the Montreal Cognitive Assessment. A partial right homonymous hemianopsia is noted. Motor and reflex examinations are normal with intact vibratory sensation. He exhibits dysdiadochokinesia and dysmetria on testing of his upper and lower extremities along with a wide-based gait. CT scan of the head is normal. Real-time quaking-induced conversion testing of his cerebrospinal fluid is positive. This patient will most likely develop which of the following?
A)Cogwheel rigidity
B)Flaccid paralysis
C)Multiple cranial neuropathies
D)Myoclonus
E)Peripheral neuropathy
A)Cogwheel rigidity
B)Flaccid paralysis
C)Multiple cranial neuropathies
D)Myoclonus
E)Peripheral neuropathy

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
19
A 14-year-old boy is brought to the office due to lower back and buttock pain for 3 months. The pain is diffuse across the lower back and buttocks, worsens with activity, and resolves with rest. It occasionally radiates down the legs. There is no history of trauma. Vital signs are normal. Examination shows a subcutaneous lipoma over the lower back, mild scoliosis, and weak ankle dorsiflexion. Deep tendon reflexes are 1+ in the lower extremities and 2+ in the upper extremities. The lower extremities are thin and weak. What is the most likely diagnosis in this patient?
A)Ankylosing spondylitis
B)Becker muscular dystrophy
C)Guillain-Barré syndrome
D)Herniated disc
E)Tethered spinal cord
A)Ankylosing spondylitis
B)Becker muscular dystrophy
C)Guillain-Barré syndrome
D)Herniated disc
E)Tethered spinal cord

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
20
A 48-year-old woman with diabetes mellitus comes to the office for a routine follow-up. The patient reports difficulty falling asleep and feeling exhausted and sleepy during the day over the past several weeks. On further questioning, she describes vague discomfort in her legs between the knees and ankles that is worse at night. The patient often gets out of bed to move around, which transiently improves the symptoms. She has a history of gestational diabetes and was diagnosed with type 2 diabetes mellitus 3 years ago for which she takes metformin. Her most recent hemoglobin A1c level was 7.6%. Blood pressure is 126/68 mm Hg and pulse is 76/min. BMI is 32 kg/m2. Lower extremity examination shows scattered dilated superficial veins but no skin ulceration. Sensation to light touch and vibration is normal in the toes. Ankle and knee reflexes are normal bilaterally. Which of the following is the best next step in evaluation of this patient?
A)Arterial ultrasonography
B)Nerve conduction studies
C)No additional testing
D)Overnight polysomnography
E)Serum iron studies
F)Venous ultrasonography
A)Arterial ultrasonography
B)Nerve conduction studies
C)No additional testing
D)Overnight polysomnography
E)Serum iron studies
F)Venous ultrasonography

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
21
A 2-year-old girl is brought to the clinic due to irritability for 2 weeks. She has also had intermittent fevers and poor appetite. The patient has had no cough, rhinorrhea, vomiting, or diarrhea. She has no chronic medical conditions and takes no medications. Her parents have a history of cold sores but have had no recent outbreaks. The family recently went camping but has not traveled internationally. Temperature is 36.7 C (98 F), blood pressure is 90/50 mm Hg, pulse is 104/min, and respirations are 22/min. On examination, the patient is tired-appearing and pale. The right upper eyelid is drooping and the right pupil is constricted. When the patient cries, only the left side of the face appears flushed. Cardiopulmonary examination is unremarkable. The abdomen is soft, nontender, and nondistended with no palpable masses. She has no dysmetria when reaching for objects and has full strength in all extremities. MRI reveals a cervical paravertebral mass. Which of the following is the most likely diagnosis?
A)Herpes simplex virus infection
B)Lyme disease
C)Medulloblastoma
D)Neuroblastoma
E)Pheochromocytoma
F)Pilocytic astrocytoma
A)Herpes simplex virus infection
B)Lyme disease
C)Medulloblastoma
D)Neuroblastoma
E)Pheochromocytoma
F)Pilocytic astrocytoma

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
22
A 3-year-old girl is brought to the emergency department for sudden onset of weakness. She was well until this morning, when she woke up and was unable to climb out of bed. Her mother lifted her up, but the child was unable to bear weight on her right leg. She could not grasp her mother's hand to stand up. The patient has had no recent fevers or upper respiratory symptoms. She was adopted from Nigeria 6 months ago, and family history is unknown. The child has had no hospitalizations or illnesses since her adoption. Her developmental milestones have been appropriate for age. Temperature is 37.2 C (99 F), pulse is 140/min, and respirations are 18/min. The patient is awake and alert but has difficulty articulating. Her head is normocephalic and atraumatic. Pupils are 2 mm and react to light and accommodation. Tympanic membranes and pharynx are clear. Cardiovascular examination demonstrates tachycardia but normal S1 and S2 without murmurs. Lungs are clear on auscultation. There is significant weakness, hypotonia, and hyperreflexia of the right arm and leg. Neuroimaging studies are pending. Which of the following additional tests is most likely to reveal an underlying abnormality in this patient?
A)Cerebrospinal fluid culture
B)Echocardiography
C)Electroencephalography
D)Hemoglobin electrophoresis
E)Muscle biopsy
F)Serum ammonia
A)Cerebrospinal fluid culture
B)Echocardiography
C)Electroencephalography
D)Hemoglobin electrophoresis
E)Muscle biopsy
F)Serum ammonia

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
23
A 14-year-old girl is brought to the office for evaluation of hand tremors. A week ago, the patient began experiencing a fluttering sensation, followed by involuntary shaking of her right hand. The shaking resolved spontaneously after an hour but has recurred several times since and also involved the left hand. The tremor occurs at rest or during activities and can be interrupted only by either grasping an object or clenching the hand. Vital signs are within normal limits. On physical examination, the patient has a flat affect. At rest, low-frequency tremors of both hands are present. Cranial nerve examination, motor strength, and deep tendon reflexes are normal. The tremors cease during the examination, but at the end, a bilateral coarse tremor can be observed. Which of the following is the most likely diagnosis?
A)Cerebellar tremor
B)Essential tremor
C)Functional tremor
D)Orthostatic tremor
E)Physiologic tremor
A)Cerebellar tremor
B)Essential tremor
C)Functional tremor
D)Orthostatic tremor
E)Physiologic tremor

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
24
A 65-year-old woman is brought to the office by her daughter due to forgetfulness and bizarre behavior. She recently began living with her daughter, who has noticed that the patient frequently misplaces items, forgets the purpose of an errand, and asks the same questions repeatedly. The patient had a left anterior cerebral artery embolic stroke 4 months ago. Her right leg weakness has slightly improved with physical rehabilitation at a nursing facility, but she still has to use a walker for ambulation. Her daughter states that prior to the stroke, the patient was living on her own and was "very social, outgoing, and full of life." Now, she is completely withdrawn and has no interest in day-to-day activities. She has also become suspicious of her daughter and is hoarding things. Other medical history includes hypertension and atrial fibrillation. On physical examination, the patient has a flat affect, normal speech, and right lower extremity weakness. Mental status examination shows short-term memory loss. Mini-Mental State Examination score is 22/30 and Clock-Drawing reveals executive cognitive dysfunction. Which of the following is the most likely cause of this patient's memory impairment?
A)Adjustment disorder
B)Alzheimer disease
C)Frontotemporal dementia
D)Poststroke depression
E)Vascular dementia
A)Adjustment disorder
B)Alzheimer disease
C)Frontotemporal dementia
D)Poststroke depression
E)Vascular dementia

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
25
A 60-year-old man is brought to the emergency department after he was found unresponsive at the bottom of a stairwell. Upon arrival, the patient is hemodynamically stable but has a Glasgow coma score of 7. There are no other obvious injuries. CT scan of the head reveals no skull fractures or large hematoma. The patient is intubated for airway protection. His mentation does not improve over the next several hours, and diffuse axonal injury is suspected. Which of the following neuroimaging findings is most suggestive of this patient's diagnosis?
A)Downward displacement of cerebellar tonsils
B)Generalized decrease in cerebral volume
C)Hyperdense blood in the basal cisterns
D)Lateral shift in the midline structures
E)Punctate hemorrhages in the white matter
A)Downward displacement of cerebellar tonsils
B)Generalized decrease in cerebral volume
C)Hyperdense blood in the basal cisterns
D)Lateral shift in the midline structures
E)Punctate hemorrhages in the white matter

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
26
An 18-month-old girl is brought to the emergency department after having a seizure in day care. The staff reports that "she suddenly fell down and started shaking," but they also note that the patient has seemed quieter and has repeatedly pulled at her hair over the past month. The patient's mother says, "My daughter used to say 'mama' and 'papa' and babble away but has begun to talk less in the past few months. She's also become more needy, wanting me to feed her rather than using a spoon herself." Medical history is significant for 3 ear infections in the past year and another seizure thought to have been febrile in origin. Family history is significant for early-onset Alzheimer disease in the patient's paternal grandfather and retinoblastoma in a paternal cousin. The patient is afebrile, and other vital signs are normal. On physical examination, the patient makes eye contact with the physician but speaks no words. She is noted to have a lurching gait. Which of the following would most likely establish a diagnosis in this patient?
A)DNA analysis
B)Enzyme analysis
C)MRI of the brain
D)Ophthalmologic evaluation
E)Serum amino acids
A)DNA analysis
B)Enzyme analysis
C)MRI of the brain
D)Ophthalmologic evaluation
E)Serum amino acids

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
27
A 24-year-old man comes to the office due to vision disturbances. The patient has a history of ankylosing spondylitis and experienced severe pain and redness of the eyes a month ago. Evaluation at that time showed acute anterior uveitis and prednisolone eye drops were prescribed, which the patient still uses. The eye symptoms resolved within a week of treatment, but over the past several days the patient has had blurry vision and has needed more light to read. He has also experienced glare while driving at night. The patient has no other medical conditions, and his only other prescribed medication is naproxen as needed. Vital signs are within normal limits. Ocular examination shows nonerythematous conjunctiva, clear corneas, and no hypopyon or opacities of the lenses. Funduscopic examination is normal. The remainder of the physical examination, including neurologic examination, shows no abnormalities. Which of the following is the most appropriate next step in management of this patient?
A)Fluorescein eye stain
B)Lumbar puncture
C)MRI of the brain
D)No further intervention
E)Tonometry
A)Fluorescein eye stain
B)Lumbar puncture
C)MRI of the brain
D)No further intervention
E)Tonometry

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
28
A 62-year-old man is brought to the emergency department after losing consciousness at church 30 minutes earlier. The patient was attending a service with his wife when he suddenly became unresponsive. He was noted to have brief jerking movements of the arms. The patient was helped to the floor and became responsive and was back at his baseline mental status after about 2 minutes. In the emergency department, the patient is awake and alert, and he has mild tongue pain. The patient had a similar episode 3 weeks ago; while sitting on the toilet, he became disoriented and then found himself lying on the bathroom floor. He had no lightheadedness or chest pain prior to these events. Medical history includes hypertension, myocardial infarction, and stroke with no residual neurologic deficit. Vital signs are within normal limits, and there are no orthostatic changes. A small, nonbleeding laceration is present on the lateral border of the tongue. The lungs are clear on auscultation, and heart sounds are normal. Neurologic examination reveals normal cranial nerves; there is no focal weakness or sensory loss. Which of the following findings in this patient are most indicative of epileptic seizure compared to syncope?
A)Abnormal extremity movements
B)Accompanying tongue biting
C)Episodic nature of the symptoms
D)Patient position at onset
E)Transition time to return to baseline
A)Abnormal extremity movements
B)Accompanying tongue biting
C)Episodic nature of the symptoms
D)Patient position at onset
E)Transition time to return to baseline

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
29
A 38-year-old, right-handed woman is brought to the emergency department after a brief seizure witnessed by her husband. The patient has never before had a seizure but has had headaches for several weeks. Her husband says that she has acted strangely for several months. The patient used to be quite social, but lately, she is not motivated to participate in any social activities and has lost interest in everyday activities. She will not talk unless directly spoken to and has impaired memory. The patient has no significant medical or psychiatric history. There is no family history of neurologic disorders. Temperature is 36 C (96.8 F), blood pressure is 130/78 mm Hg, and pulse is 86/min. On examination, the patient is somnolent but wakes to voice and follows commands. The pupils are equal and reactive. Funduscopy reveals bilateral papilledema. Bilateral upper and lower extremity muscle strength is normal. Neuroimaging is most likely to reveal which of the following findings in this patient?
A)Frontotemporal lobe atrophy
B)Ischemic infarction of the brainstem
C)Right parietal lobe lesion
D)Sclerosis of the mesial temporal lobe
E)Solitary mass in the frontal lobe
A)Frontotemporal lobe atrophy
B)Ischemic infarction of the brainstem
C)Right parietal lobe lesion
D)Sclerosis of the mesial temporal lobe
E)Solitary mass in the frontal lobe

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
30
A 3-year-old boy with DiGeorge syndrome is brought to the emergency department after a 5-minute, generalized tonic-clonic seizure. For the past week, the patient has been increasingly tired and has had severe morning headaches, which have not been relieved by acetaminophen or ibuprofen. He has been dragging his right leg for several days while walking. His appetite has decreased, and he has been vomiting after waking up in the morning. The patient's family recently emigrated from a developing country to obtain care for his unrepaired tetralogy of Fallot. The patient has speech delay and a history of recurrent pneumonias and sinus infections. Temperature is 38.3 C (101 F). Physical examination shows a tired-appearing child with dysmorphic facial features. The right lower extremity exhibits decreased strength and the ankle deep tendon reflex is hyperreflexic; the left lower extremity is normal. There is no truncal ataxia. Which of the following is the most likely cause of this patient's symptoms?
A)Bacterial meningitis
B)Brain abscess
C)Hypocalcemia
D)Hypoglycemia
E)Hyponatremia
F)Medulloblastoma
G)Thromboembolic stroke
A)Bacterial meningitis
B)Brain abscess
C)Hypocalcemia
D)Hypoglycemia
E)Hyponatremia
F)Medulloblastoma
G)Thromboembolic stroke

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
31
A 13-year-old girl is brought to the emergency department due to a head injury. The patient was climbing a tree when she fell and injured the right side of her head. She briefly lost consciousness after the injury. On arrival, the patient is awake and reports pain over the right frontal area but has no focal neurologic deficits. CT scan of the head reveals a right frontotemporal epidural hematoma. Neurosurgery is consulted for craniotomy. While waiting for the surgery, the patient becomes somnolent and develops left lower extremity weakness. Bilateral pupillary responses are normal. Which of the following best explains this patient's worsening neurologic status?
A)Diffuse axonal injury
B)Subarachnoid hemorrhage
C)Subfalcine herniation
D)Tonsillar herniation
E)Uncal herniation
A)Diffuse axonal injury
B)Subarachnoid hemorrhage
C)Subfalcine herniation
D)Tonsillar herniation
E)Uncal herniation

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
32
A 5-year-old boy is brought to the office by his parents for evaluation of "clumsiness." The patient's fine and gross motor development have been normal at prior visits, but he now frequently runs into doorways or corners of furniture while walking around the house. He has also begun drinking large amounts of water and urinating "all the time." Temperature is 37 C (98.6 F), blood pressure is 95/65 mm Hg, and pulse is 130/min. Physical examination shows dry mucous membranes and loss of peripheral visual fields. Laboratory results are as follows:  CT scan of the brain (exhibit)
CT scan of the brain (exhibit)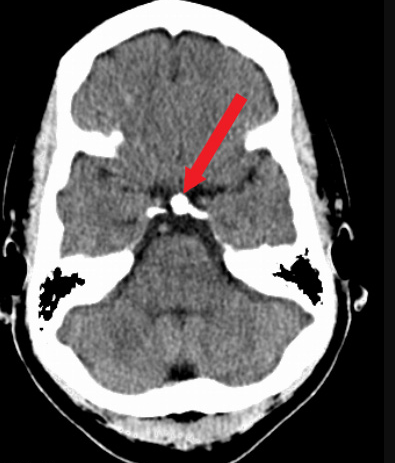 reveals an abnormality. Which of the following is the most likely diagnosis?
reveals an abnormality. Which of the following is the most likely diagnosis?
A)Craniopharyngioma
B)Medulloblastoma
C)Parasagittal meningioma
D)Pituitary adenoma
E)Rathke cleft cyst
 CT scan of the brain (exhibit)
CT scan of the brain (exhibit)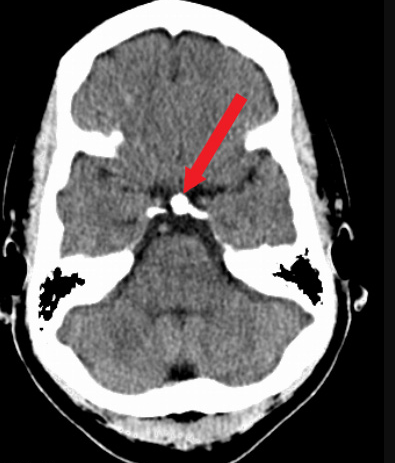 reveals an abnormality. Which of the following is the most likely diagnosis?
reveals an abnormality. Which of the following is the most likely diagnosis?A)Craniopharyngioma
B)Medulloblastoma
C)Parasagittal meningioma
D)Pituitary adenoma
E)Rathke cleft cyst

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
33
An 18-year-old man is brought to the emergency department following a generalized tonic-clonic seizure. He developed full body jerking at home this morning, which lasted approximately 1 minute. The episode occurred just before the patient was about to visit the clinic for evaluation of a worsening headache for the past 2 days. His parents say that he has also seemed clumsy over the same period, including tripping a few times yesterday. He has no history of seizures and was previously healthy except for seasonal allergies managed with over-the-counter medications. Temperature is 38.9 C (102 F), blood pressure is 130/80 mm Hg, and pulse is 92/min. The patient is awake but oriented only to person. Pupillary examination is unremarkable. The patient has bilateral hyperreflexia in the upper and lower extremities. MRI of the brain is shown below: 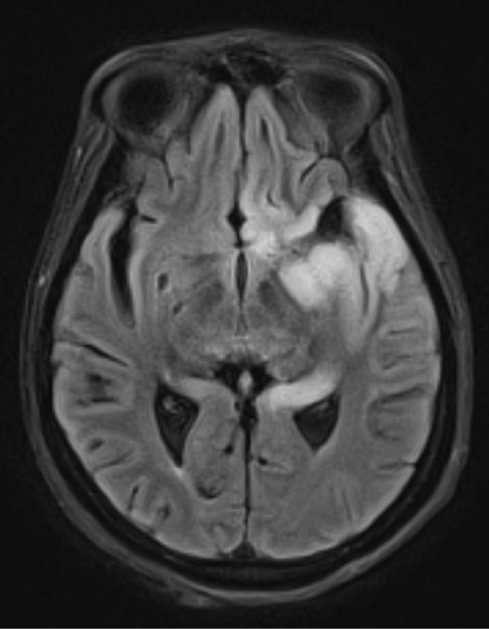 Which of the following is the most likely diagnosis for this patient?
Which of the following is the most likely diagnosis for this patient?
A)Drug-induced encephalopathy
B)Herpes simplex virus encephalitis
C)Medulloblastoma
D)Reye syndrome
E)Subacute sclerosing panencephalitis
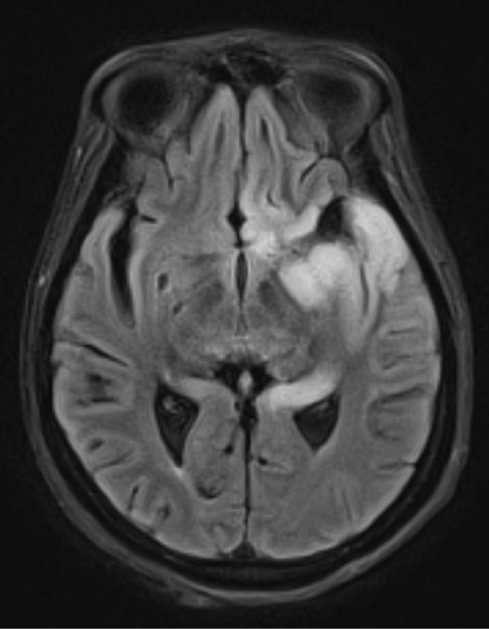 Which of the following is the most likely diagnosis for this patient?
Which of the following is the most likely diagnosis for this patient?A)Drug-induced encephalopathy
B)Herpes simplex virus encephalitis
C)Medulloblastoma
D)Reye syndrome
E)Subacute sclerosing panencephalitis

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
34
A 54-year-old man comes to the office due to right shoulder and arm pain. His symptoms began 3 days ago after playing golf for several hours. The patient states that his right arm feels weak, especially when lifting objects. He has no prior medical conditions and takes no medications. Physical examination shows spasm of the cervical paraspinal muscles. There is mild weakness of right elbow flexion, and the biceps reflex is decreased on the right. The pain improves when the patient is instructed to lift the right arm above the head and rest the hand on the top of his head. Which of the following is the most likely diagnosis?
A)Cervical muscle strain
B)Cervical radiculopathy
C)Rotator cuff muscle tear
D)Shoulder joint capsulitis
E)Thoracic outlet syndrome
A)Cervical muscle strain
B)Cervical radiculopathy
C)Rotator cuff muscle tear
D)Shoulder joint capsulitis
E)Thoracic outlet syndrome

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
35
A 69-year-old man is brought to the office by his wife due to recent changes in behavior. Despite years of managing the family's finances, over the previous 12 months the patient has failed to pay a number of important bills. He has become more withdrawn and no longer enjoys social gatherings. When he does socialize now, he is often irritable and offensive. The patient used to smoke a quarter pack of cigarettes a day but has increased to a pack a day over the previous 12 months. He also now insists on eating the same thing for breakfast every morning and gets very upset if a different meal is prepared. The patient denies having any problems and seems indifferent to his wife's concern. Medical history includes hypertension and type 2 diabetes mellitus. There is a family history of Alzheimer disease. Temperature is 36.7 C (98 F), blood pressure is 144/86 mm Hg, pulse is 62/min, and respirations are 14/min. The patient scores a 24 out of 30 on the Montreal Cognitive Assessment (normal ≥26). Which of the following is the most likely diagnosis in this patient?
A)Alzheimer disease
B)Creutzfeldt-Jakob disease
C)Dementia with Lewy bodies
D)Frontotemporal dementia
E)Mild cognitive impairment
F)Vascular dementia
A)Alzheimer disease
B)Creutzfeldt-Jakob disease
C)Dementia with Lewy bodies
D)Frontotemporal dementia
E)Mild cognitive impairment
F)Vascular dementia

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
36
A 30-year-old man is brought to the emergency department due to a worsening headache. The patient has had episodic right-sided headaches over the past 6 months. Thirty minutes ago, he began experiencing a right temporal headache while at rest, which gradually worsened to severe pain over the next several minutes. He also had nausea and an episode of vomiting. The patient is now somnolent and difficult to rouse. He has no other medical conditions and had a normal medical evaluation a year ago for military enlistment. Temperature is 37 C (98.6 F), blood pressure is 150/90 mm Hg, pulse is 64/min, and respirations are 14/min. The patient withdraws all extremities to painful stimuli, but left-sided deep tendon reflexes are increased. There is no neck rigidity. Which of the following is the most likely underlying cause of this patient's current condition?
A)Arteriovenous malformation
B)Carotid artery atheroma
C)Cerebral amyloid angiopathy
D)Dural venous sinus thrombosis
E)Hypertensive vasculopathy
F)Paroxysmal cardiac arrhythmia
A)Arteriovenous malformation
B)Carotid artery atheroma
C)Cerebral amyloid angiopathy
D)Dural venous sinus thrombosis
E)Hypertensive vasculopathy
F)Paroxysmal cardiac arrhythmia

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
37
A 22-year-old woman comes to the office due to recurrent syncopal episodes. The first episode occurred about a year ago when her roommate died by suicide. Since then, she has had several similar episodes provoked by strong emotion. The episodes are preceded by lightheadedness, weakness, and blurred vision; last about 3 minutes; and end with rapid recovery of consciousness. The patient has had no significant injuries related to syncope except once when she had superficial bruises. Medical history is insignificant. She takes no medications and does not use alcohol or illicit drugs. Blood pressure is 110/70 mm Hg while supine and 108/70 mm Hg while standing. Physical examination findings are within normal limits. A recent ECG was normal. Which of the following is the best next step in management of this patient?
A)24-hour (Holter) monitoring
B)Carotid sinus massage
C)Counterpressure maneuver education
D)Low-dose beta blocker therapy
E)Transthoracic echocardiography
A)24-hour (Holter) monitoring
B)Carotid sinus massage
C)Counterpressure maneuver education
D)Low-dose beta blocker therapy
E)Transthoracic echocardiography

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
38
A 45-year-old woman comes to the office due to tremor in her hands. She has had an on-and-off tremor for several years, especially when she becomes stressed; however, over the past 6 weeks, the tremor has persisted and become more severe. The patient has no other symptoms. Medical history is significant for generalized anxiety disorder, for which she has been taking sertraline for 2 months. The patient does not drink alcohol. There is no family history of tremor or neurologic conditions. Temperature is 36.8 C (98.2 F), blood pressure is 130/84 mm Hg, pulse is 82/min, and respirations are 16/min. Physical examination shows a high-frequency tremor of both hands that is prominent with finger-to-nose testing. The tremor is not relieved with distraction. The remainder of the examination is normal. Complete blood count, serum chemistry profile, and serum TSH are normal. What is the most likely diagnosis?
A)Cerebellar tremor
B)Dystonic tremor
C)Enhanced physiologic tremor
D)Functional (psychogenic) tremor
E)Parkinson disease
A)Cerebellar tremor
B)Dystonic tremor
C)Enhanced physiologic tremor
D)Functional (psychogenic) tremor
E)Parkinson disease

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
39
A 36-year-old previously healthy man comes to the office due to neck pain. Two days ago, the patient was lifting weights when he suddenly experienced neck and upper back pain. He has had constant dull pain and intermittent sharp pain with neck movements that radiates to his left hand. He also reports a tingling sensation in the left hand but has had no weakness or bladder or bowel dysfunction. Vital signs are within normal limits. Physical examination shows cervical paraspinal muscle spasm. There is mildly decreased sensation to pinprick in the left fourth and fifth digits. There are no other sensory deficits and no upper or lower extremity muscle weakness is present. Deep tendon reflexes are normal throughout. Which of the following is the most appropriate next step in management of this patient?
A)Cervical spine x-ray
B)Epidural corticosteroid injection
C)MRI of the cervical spine
D)Provocative activity avoidance and NSAIDs
E)Urgent neurosurgical evaluation
A)Cervical spine x-ray
B)Epidural corticosteroid injection
C)MRI of the cervical spine
D)Provocative activity avoidance and NSAIDs
E)Urgent neurosurgical evaluation

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
40
A 3-year-old, previously healthy girl is brought to the emergency department due to difficulty swallowing. The patient has had fever, chills, malaise, myalgias, and sore throat for a week. Today, she is refusing to drink fluids and spits out any liquids given to her. The patient has a history of small puncture wounds on her left forearm that the family noticed 2 months prior. It is unclear how the wounds occurred, but the site was cleaned and dressed and has since healed completely. Temperature is 40 C (104 F), blood pressure is 90/60 mm Hg, pulse is 144/min, and respirations are 34/min. Examination shows an agitated, disoriented girl with copious drool and facial grimacing who frequently spits saliva. There is numbness surrounding a small, healed scar on the left forearm. The neck is supple with full range of motion. Which of the following is the most likely diagnosis?
A)Herpes simplex virus encephalitis
B)Rabies
C)Tetanus
D)West Nile virus
E)Wound botulism
A)Herpes simplex virus encephalitis
B)Rabies
C)Tetanus
D)West Nile virus
E)Wound botulism

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
41
A 62-year-old woman comes to the emergency department feeling "dizzy." While at a grocery store today, the patient was looking up at a high shelf when she suddenly experienced a spinning sensation accompanied by nausea. She closed her eyes and sat down in the aisle, and the symptoms resolved after about a minute. The patient has had no headache, earache, tinnitus, or hearing impairment. The symptoms recurred 30 minutes later when she bent down to get into her car. Currently, she feels well and has no symptoms. Medical history is significant for hypertension, hyperlipidemia, and type 2 diabetes mellitus. She previously smoked a pack of cigarettes a day but quit 10 years ago. Which of the following is most likely to reveal the underlying cause of this patient's symptoms?
A)Comprehensive audiogram
B)MRA of the vertebrobasilar arteries
C)MRI of the internal auditory canals
D)Orthostatic blood pressure measurement
E)Provocative head positioning maneuvers
A)Comprehensive audiogram
B)MRA of the vertebrobasilar arteries
C)MRI of the internal auditory canals
D)Orthostatic blood pressure measurement
E)Provocative head positioning maneuvers

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
42
A 65-year-old man is brought to the emergency department after being involved in a motor vehicle collision. He lost consciousness briefly on impacting the airbag. Since regaining consciousness, the patient has had numbness, tingling, and marked weakness in both upper extremities but has been able to move his lower extremities normally. Medical history includes osteoarthritis and cervical spondylosis. Blood pressure is 132/74 mm Hg, pulse is 94/min, and respirations are 14/min. Plain x-rays of the cervical spine show no abnormalities except those consistent with mild degenerative arthritis. Which of the following is the most likely diagnosis?
A)Anterior cord syndrome
B)Brown-Séquard syndrome
C)Central cord syndrome
D)Cerebral contusion
E)Posterior cord syndrome
A)Anterior cord syndrome
B)Brown-Séquard syndrome
C)Central cord syndrome
D)Cerebral contusion
E)Posterior cord syndrome

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
43
A 74-year-old woman is brought to the emergency department due to worsening weakness and gait unsteadiness. The patient has a history of ischemic stroke causing right-sided weakness and uses a cane to ambulate. Over the past several days, she has been feeling weak and unsteady, and this morning she fell while getting out of bed. She did not lose consciousness and has had no headache, vomiting, or vision loss. The patient recently has had dysuria and urinary urgency, which have improved after taking trimethoprim-sulfamethoxazole. Other medical conditions include hypertension, type 2 diabetes mellitus, and seizure disorder controlled with phenytoin. Temperature is 37.1 C (98.8 F), blood pressure is 140/86 mm Hg, and pulse is 84/min. Pupils are equal and briskly reactive, and extraocular movements are intact. There is bilateral nystagmus on lateral gaze. Muscle strength is diffusely decreased but more pronounced in the right extremities. Deep tendon reflexes are increased throughout. Dysmetria is present on finger-nose testing, and the gait is wide-based. Which of the following is the most likely cause of this patient's current condition?
A)Epidural abscess
B)Folate deficiency
C)Medication toxicity
D)Septic encephalopathy
E)Subdural hematoma
A)Epidural abscess
B)Folate deficiency
C)Medication toxicity
D)Septic encephalopathy
E)Subdural hematoma

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
44
A 56-year-old woman is evaluated for a monthlong history of intermittent weakness of the right foot and a 3-month history of progressive left arm weakness. The patient has no dysphagia, dysarthria, sensory loss, or bowel or bladder impairment. Other medical conditions include type 2 diabetes mellitus, hypercholesterolemia, and hypertension. She takes metformin, atorvastatin, and lisinopril. Temperature is 36.9 C (98.4 F), blood pressure is 130/78 mm Hg, pulse is 80/min, and respirations are 14/min. Neurologic examination reveals normal speech, language, and mental status. Moderate weakness and atrophy of the distal muscles in the right leg and left arm is noted. Fasciculations are present in the right leg. Deep tendon reflexes are brisk in the upper and lower limbs. Sensory examination shows no abnormalities. Laboratory results are as follows:  Which of the following would be most helpful in treating this patient's current symptoms?
Which of the following would be most helpful in treating this patient's current symptoms?
A)Intensive blood glucose control
B)Interferon beta
C)Levothyroxine
D)Prednisone
E)Riluzole
F)Statin discontinuation
 Which of the following would be most helpful in treating this patient's current symptoms?
Which of the following would be most helpful in treating this patient's current symptoms?A)Intensive blood glucose control
B)Interferon beta
C)Levothyroxine
D)Prednisone
E)Riluzole
F)Statin discontinuation

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
45
A 6-year-old girl is brought to the clinic by her parents after multiple falls while running in the past few months. Over the past month, the patient has also had intermittent headaches, with increased frequency in the past 2 weeks. The headaches are worse in the morning and have occasionally been accompanied by nausea and vomiting. Examination shows a tired-appearing young girl. The patient walks with a wide-based gait and has difficulty with heel-to-toe walking. Eye examination reveals bilateral abducens nerve palsies and papilledema. The remainder of the cranial nerve examination is normal. Strength is 5/5 in bilateral upper and lower extremities. Sensation is intact, and reflexes are 2+ bilaterally. Babinski testing reveals plantar flexion of the toes. Which of the following is most likely responsible for this patient's symptoms?
A)Acoustic neuroma
B)Craniopharyngioma
C)Glioblastoma
D)Medulloblastoma
E)Meningioma
F)Pinealoma
A)Acoustic neuroma
B)Craniopharyngioma
C)Glioblastoma
D)Medulloblastoma
E)Meningioma
F)Pinealoma

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
46
A 74-year-old man comes to the emergency department due to 2 weeks of progressive leg weakness and difficulty standing and walking. He has also had increasing urinary hesitancy and dribbling of urine. The patient has had low back pain for several months, but the pain has recently worsened and begun radiating to his legs. He was diagnosed with metastatic squamous cell lung cancer a year ago and received chemotherapy initially, but the patient stopped treatment due to side effects. He also has a history of hypertension and chronic obstructive pulmonary disease. Lower extremity examination shows normal bulk and tone but decreased strength of major muscle groups bilaterally. Knee reflexes are decreased on both sides. There are patchy areas of sensory loss in the bilateral lower extremities. Digital rectal examination shows loss of sensation in the perianal skin, decreased anal sphincter tone, and mildly enlarged prostate. A lesion at which of the following sites is most likely responsible for this patient's symptoms?
A)Cauda equina nerve roots
B)Cerebral cortex
C)Cervical spinal cord
D)Conus medullaris
E)Lumbar spinal cord
F)Peripheral nerve fibers
G)Thoracic spinal cord
A)Cauda equina nerve roots
B)Cerebral cortex
C)Cervical spinal cord
D)Conus medullaris
E)Lumbar spinal cord
F)Peripheral nerve fibers
G)Thoracic spinal cord

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
47
A 69-year-old man is evaluated shortly after undergoing elective surgical repair of a descending thoracic aortic aneurysm. He has weakness in both lower extremities and urinary retention, which were not present before the procedure. The surgery was complicated by significant blood loss requiring multiple transfusions. The patient has a history of osteoarthritis, hypertension, hyperlipidemia, type 2 diabetes mellitus, and coronary artery disease. He also has 70% stenosis of his right carotid artery. Neurologic examination shows flaccid paralysis and loss of pain sensation in the lower extremities; vibratory sensation is intact. Upper extremity examination reveals no abnormalities. Which of the following is the most likely cause of this patient's neurologic dysfunction?
A)Cervical spondylotic myelopathy
B)Epidural hematoma compressing the spinal cord
C)Intraoperative cortical stroke
D)Lumbar plexopathy
E)Spinal cord infarction
A)Cervical spondylotic myelopathy
B)Epidural hematoma compressing the spinal cord
C)Intraoperative cortical stroke
D)Lumbar plexopathy
E)Spinal cord infarction

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
48
A 23-year-old man is found unconscious at the scene of a motor vehicle collision with an obvious left leg deformity and a large laceration of the left temporal scalp. As the patient is being rolled onto a backboard, he regains consciousness. He recalls no details of the collision but reports severe left leg pain, headache, and some shortness of breath. Blood pressure is 94/60 mm Hg, pulse is 120/min, and respirations are 18/min. Peripheral intravenous access is obtained, and 1 L of intravenous fluids is administered. On the way to the hospital, the patient develops progressive weakness on the right side and becomes obtunded. On arrival, blood pressure is 160/90 mm Hg, pulse is 50/min, and respirations are 10/min. Which of the following nerves is most likely to be compromised in this patient?
A)Accessory
B)Facial
C)Glossopharyngeal
D)Oculomotor
E)Vestibulocochlear
A)Accessory
B)Facial
C)Glossopharyngeal
D)Oculomotor
E)Vestibulocochlear

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
49
A 3-month-old full-term boy is brought to the emergency department for refusal to feed. The infant has been exclusively breastfed since birth but has not been latching onto the nipple. He has been urinating normally and usually stools 3 or 4 times a day, but his last bowel movement was several days ago. He was previously able to hold his head up on his own but his head now seems floppy. The patient's family recently moved to California and has been enjoying stroller walks in their newly built neighborhood. Other than daily vitamin D supplementation, the infant has never ingested food, even honey. Vital signs are normal. Examination shows bilateral ptosis, sluggish pupillary reaction to light, copious drool, weak suck and gag reflexes, and head lag. The extremities are flaccid and in extension. What is the most likely mechanism of this patient's illness?
A)Ascending demyelinating polyneuropathy
B)Autoantibodies against acetylcholine receptors
C)Bacterial infection of the meninges
D)Degeneration of the anterior horn cells in the spinal cord
E)Ingestion of Clostridium difficile spores
F)Ingestion of Clostridium botulinum spores
G)Ingestion of preformed Clostridium botulinum toxin
A)Ascending demyelinating polyneuropathy
B)Autoantibodies against acetylcholine receptors
C)Bacterial infection of the meninges
D)Degeneration of the anterior horn cells in the spinal cord
E)Ingestion of Clostridium difficile spores
F)Ingestion of Clostridium botulinum spores
G)Ingestion of preformed Clostridium botulinum toxin

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
50
A 45-year-old woman comes to the office to discuss her facial asymmetry. For the past 6 weeks, the right side of her face has been progressively weakening. The patient notices there are fewer wrinkles on the right side of her forehead than on the left, and the fold in front of her cheek seems less deep. Sometimes she has "spasms" of the right side of her face, and her right eye feels "gritty, like there is sand in it." The patient has no chronic medical conditions and takes no medications. Vital signs are within normal limits. On examination, the ears are clear with no lesions. She is unable to hear a finger rub on the right side. Extraocular movements are intact; there is edema and erythema of the conjunctiva on the right, and normal conjunctiva on the left. Pupils are equal and reactive to light. There is asymmetry between the left and right sides of the face at rest. When asked to move her face, there is a little movement of right-sided parts of the face, including the forehead. There is incomplete eye closure of the right eye; the left eye closes fully. Which of the following is the most appropriate next step in diagnosis?
A)CT angiography of the head
B)HIV testing
C)Lumbar puncture
D)MRI of the head
E)No additional testing needed
A)CT angiography of the head
B)HIV testing
C)Lumbar puncture
D)MRI of the head
E)No additional testing needed

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
51
A 71-year-old man is brought to the office by his daughter due to a change in behavior over the past year. He began having memory problems several years ago and frequently forgot his grandchildren's names. Also, the patient often had difficulty finding words. Several times recently, he was found roaming his apartment building because he was lost. The patient insists that there is nothing wrong with him and jokingly makes excuses for the symptoms his daughter is reporting. He has never used alcohol or illicit drugs. Blood pressure is 155/85 mm Hg, pulse is 90/min, and respirations are 15/min. Plantar reflexes are downgoing bilaterally. The remainder of the neurologic examination is within normal limits. Montreal Cognitive Assessment score is 15 on a scale of 30 (normal: ≥26). Laboratory results are as follows:  Which of the following abnormalities is most likely to be seen on this patient's MRI?
Which of the following abnormalities is most likely to be seen on this patient's MRI?
A)Diffuse cortical and subcortical infarctions
B)Enlarged lateral ventricles without cortical atrophy
C)Frontal lobe atrophy
D)Parietal lobe atrophy
E)Temporal lobe atrophy
 Which of the following abnormalities is most likely to be seen on this patient's MRI?
Which of the following abnormalities is most likely to be seen on this patient's MRI?A)Diffuse cortical and subcortical infarctions
B)Enlarged lateral ventricles without cortical atrophy
C)Frontal lobe atrophy
D)Parietal lobe atrophy
E)Temporal lobe atrophy

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
52
A 28-year-old woman comes to the emergency department due to left-sided headache and neck pain after a fall while skiing the day prior. She took ibuprofen and rested but the symptoms persisted, and today, she also had transient leg weakness. The patient has no prior medical conditions. She occasionally drinks alcohol but does not use tobacco or illicit drugs. Family history is significant for stroke in her father. Temperature is 37.2 C (99 F), blood pressure is 134/86 mm Hg, and pulse is 90/min. Physical examination shows mild ptosis and miosis of the left eye. There is no excessive lacrimation or rhinorrhea. Funduscopic examination is normal. No carotid bruit is present. Heart and lung sounds are normal. Neurological examination shows normal motor strength, deep tendon reflexes, and sensation in bilateral upper and lower extremities. Which of the following is the most likely cause of this patient's current condition?
A)Arterial dissection
B)Cluster headache
C)Diffuse axonal injury
D)Intracranial aneurysm
E)Migraine with brainstem aura
A)Arterial dissection
B)Cluster headache
C)Diffuse axonal injury
D)Intracranial aneurysm
E)Migraine with brainstem aura

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
53
A 9-year-old boy is brought to the emergency department after having a seizure at school. His teacher says he suddenly fell to the ground with sustained flexion of the arms and extension of the legs, followed by clonic movements of his whole body for 5 minutes. The patient appeared sleepy after the episode, but his behavior is now at baseline. His parents arrive shortly after and note that the boy has been increasingly tired and irritable over the last few months, and his school performance has declined this semester. The patient has no medical issues and takes no medications. Physical examination shows decreased muscle strength on the left side of the body, with brisk deep-tendon reflexes in the left arm and leg. Visual field examination is normal. MRI of the brain reveals a space-occupying lesion in the right parietal lobe. Which of the following is most likely responsible for this patient's symptoms?
A)Craniopharyngioma
B)Ependymoma
C)Glioblastoma
D)Low-grade astrocytoma
E)Medulloblastoma
F)Neuroblastoma
A)Craniopharyngioma
B)Ependymoma
C)Glioblastoma
D)Low-grade astrocytoma
E)Medulloblastoma
F)Neuroblastoma

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
54
A 58-year-old man is brought to the emergency department after a witnessed tonic-clonic seizure. The patient was at work when he suddenly collapsed and convulsed for approximately a minute. His coworker says that the patient was confused immediately afterward; however, he is now awake and cooperative. He has been having headaches for the past several weeks and has never before had a seizure. He has no prior medical problems and takes no medications. The patient is a former smoker with a 45-pack-year history. He occasionally drinks alcohol but does not use illicit drugs. The patient has lived most of his life in Texas and has never traveled outside of the country. Temperature is 36.7 C (98.1 F), blood pressure is 122/70 mm Hg, and pulse is 77/min. Cardiopulmonary auscultation is normal, and no masses are present on abdominal examination. Cranial nerves are intact, and there is no muscle weakness or sensory loss. MRI of the brain reveals several discrete, circumscribed lesions at the junction of the gray and white matter with surrounding edema. Rapid HIV testing is negative. Which of the following is the most likely cause of this patient's seizure?
A)Cerebral toxoplasmosis
B)Glioblastoma multiforme
C)Lacunar infarctions
D)Metastatic lung cancer
E)Multiple sclerosis
F)Neurocysticercosis
G)Primary central nervous system lymphoma
A)Cerebral toxoplasmosis
B)Glioblastoma multiforme
C)Lacunar infarctions
D)Metastatic lung cancer
E)Multiple sclerosis
F)Neurocysticercosis
G)Primary central nervous system lymphoma

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
55
A 10-year-old boy is brought to the clinic due to headache, vomiting, and visual disturbances. The patient has had 2 weeks of persistent headache; he was given over-the-counter analgesics but had no relief. He has also had daily episodes of nonbloody, nonbilious emesis. Neurologic examination shows bilateral retraction of the upper eyelids and limitation of upward gaze with a preference for downward gaze. Pupils react sluggishly to light but respond appropriately to accommodation. Strength, sensation, and deep tendon reflexes are normal. Gait is normal. Plantar reflexes are downgoing bilaterally. Which of the following lesions is most likely responsible for this patient's symptoms?
A)Craniopharyngioma
B)Medulloblastoma
C)Neuroblastoma
D)Pinealoma
E)Retinoblastoma
A)Craniopharyngioma
B)Medulloblastoma
C)Neuroblastoma
D)Pinealoma
E)Retinoblastoma

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
56
A 40-year-old man comes to the office due to coughing while drinking. Over the past 2 months, the patient has been coughing when he drinks water because it "goes down the wrong pipe." On occasion, water will come out of his nose when drinking. Also, his speech sounds slurred and nasal. The patient has no medical conditions and takes no medications. On examination, there are no mucosal lesions in the oral cavity or oropharynx. Palate elevation is sluggish on the right side. The tongue appears thin and there are fasciculations. When the physician taps on the chin while the mouth is slightly open, the jaw jerks forward briskly. Which of the following is the most appropriate next step to establish a diagnosis in this patient?
A)Acetylcholine receptor antibody
B)Cervical spine x-ray
C)Electromyography
D)Muscle biopsy
E)Serum creatine kinase level
F)Serum toxin assay
A)Acetylcholine receptor antibody
B)Cervical spine x-ray
C)Electromyography
D)Muscle biopsy
E)Serum creatine kinase level
F)Serum toxin assay

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
57
A 46-year-old man is being evaluated for a gait disorder. He was referred by social workers due to frequent falls. His symptoms began gradually about a year ago and have become progressively worse. The patient's history is notable for alcohol use disorder, and he is currently experiencing homelessness, with sporadic stays in a nearby shelter. On examination, he has a broad-based, unsteady gait. A single tap on his patellar tendon elicits persistent, slow, back-and-forth swinging of the leg. Nystagmus and truncal ataxia are also present. Which of the following additional findings would most likely be seen in this patient?
A)Babinski sign
B)Bradykinesia
C)"Clasp knife" spasticity
D)Goiter
E)Hearing loss
F)Postural tremor
A)Babinski sign
B)Bradykinesia
C)"Clasp knife" spasticity
D)Goiter
E)Hearing loss
F)Postural tremor

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
58
A 23-year-old man comes to the physician complaining of worsening headache over the past week. He is "under a lot of stress at school" and having trouble sleeping because the headache is constant. Two weeks ago, he had an insect bite on his right cheek and now both of his eyes are swollen. He also has lost his appetite and vomited twice today. His temperature is 38.3° C (101° F), blood pressure is 130/90 mm Hg, pulse is 104/min, and respirations are 20/min. Examination shows erythema and swelling of the right cheek and bilateral eyelid edema, right greater than left. Bilateral extraocular movements are restricted. The bilateral forehead and mid-face are extremely tender to light palpation. Which of the following is the most likely diagnosis?
A)Acute angle-closure glaucoma
B)Brain abscess
C)Cluster headache
D)Cavernous sinus thrombosis
E)Migraine with visual aura
F)Periorbital cellulitis
A)Acute angle-closure glaucoma
B)Brain abscess
C)Cluster headache
D)Cavernous sinus thrombosis
E)Migraine with visual aura
F)Periorbital cellulitis

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
59
A 65-year-old man comes to the office due to unsteady gait and frequent falls over the past 2 months. His left side feels "weak," which makes it difficult to maintain balance when walking or standing. He has also had headaches and nausea, which are worse in the mornings before he has had coffee. The patient has a history of hypertension and type 2 diabetes mellitus, and he had a myocardial infarction 5 years ago. He takes insulin for diabetes mellitus but does not routinely monitor his blood glucose. The patient is a former smoker and does not use alcohol or illicit drugs. Blood pressure is 130/80 mm Hg and pulse is 76/min. Ambulation results in the patient swaying to the left and using the wall to brace himself. There is increased resistance to passive flexion of the left upper and lower extremity. Which of the following is the most likely cause of his current condition?
A)Brain tumor
B)Diabetic polyneuropathy
C)Hemiplegic migraine
D)Lacunar infarction
E)Neuroglycopenia
F)Normal-pressure hydrocephalus
G)Parkinson disease
H)Tabes dorsalis
I)Vitamin B12 deficiency
A)Brain tumor
B)Diabetic polyneuropathy
C)Hemiplegic migraine
D)Lacunar infarction
E)Neuroglycopenia
F)Normal-pressure hydrocephalus
G)Parkinson disease
H)Tabes dorsalis
I)Vitamin B12 deficiency

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
60
A 45-year-old white male presents with a 4-month history of headaches. The headache is generalized, dull, constant, and worsened by bending, coughing and sneezing. It is unresponsive to simple analgesics, and associated with nausea and vomiting. His wife says he has been acting strangely for the last few months, and she has noted a personality change. The neurological examination is non-focal. Fundoscopy reveals papilledema. His CT scan is shown below. 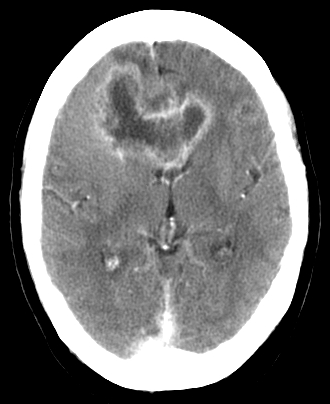 Which of the following is the most likely diagnosis?
Which of the following is the most likely diagnosis?
A)Brain abscess
B)Metastatic brain tumor
C)Glioblastoma multiforme
D)Low-grade astrocytoma
E)Cerebral infarction
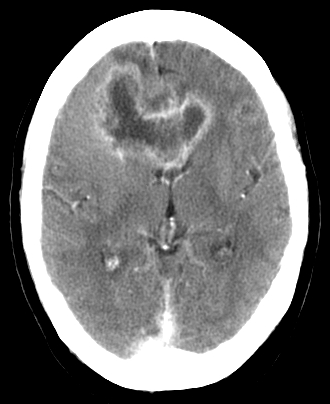 Which of the following is the most likely diagnosis?
Which of the following is the most likely diagnosis?A)Brain abscess
B)Metastatic brain tumor
C)Glioblastoma multiforme
D)Low-grade astrocytoma
E)Cerebral infarction

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
61
A 29-year-old man comes to the emergency department due to lower extremity weakness. The patient has not been feeling well over the past several days and has had worsening back pain. When he woke up this morning, he noticed weakness in both legs and had to have a friend help him walk to the car. The patient has a history of HIV, which was acquired via shared needles, but does not take antiretroviral therapy consistently. The patient still uses injection drugs occasionally but no longer shares needles. Temperature is 38 C (100.4 F), blood pressure is 116/68 mm Hg, and pulse is 98/min. The lungs are clear on auscultation, and heart sounds are normal with no murmurs. Abdominal examination shows a distended bladder. The back is tender to palpation over the lower thoracic region. Neurological examination reveals 3/5 bilateral lower extremity muscle strength with upgoing bilateral plantar reflexes. Skin examination shows scattered folliculitis and no lower extremity edema. Which of the following is the most likely cause of this patient's weakness?
A)Bacterial invasion of the epidural space
B)Immune-mediated peripheral nerve injury
C)Segmental spinal cord inflammation
D)Spondylosis-associated cord compression
E)Viral infection of the motor neurons
A)Bacterial invasion of the epidural space
B)Immune-mediated peripheral nerve injury
C)Segmental spinal cord inflammation
D)Spondylosis-associated cord compression
E)Viral infection of the motor neurons

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
62
A 4-year-old boy with sickle cell disease is brought to the emergency department by his parents due to a progressive headache and drowsiness. While coming down the stairs, the patient slipped and fell from a height of 1.5 m (5 ft), hitting his head on the tile floor. He lay on the ground for several seconds but got up and continued walking and talking normally. The patient initially had only mild pain at the injury site. A few minutes later, he developed a progressive headache and vomiting before becoming somnolent. The patient has been hospitalized multiples times for vasoocclusive crises. He takes hydroxyurea and penicillin daily. Blood pressure is 140/86 mm Hg and pulse is 66/min. The patient is sleepy and requires painful stimuli to remain awake. On neurologic examination, the left pupil is 3 mm with normal pupillary reflex, but the right pupil is 8 mm and unreactive to light. Which of the following is the most likely cause of this patient's acute decompensation?
A)Cerebral contusion
B)Epidural hematoma
C)Ischemic stroke
D)Subarachnoid hemorrhage
E)Subdural hematoma
A)Cerebral contusion
B)Epidural hematoma
C)Ischemic stroke
D)Subarachnoid hemorrhage
E)Subdural hematoma

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
63
An 86-year-old woman is brought to the emergency department due to progressive confusion and lethargy for the past several hours. The patient has a history of Alzheimer dementia, and her family reports that she has been gradually declining in mental and physical capacity for the last 6 months. She also has had several falls and requires assistance with daily activities. Other medical conditions include hypertension and osteoarthritis. Temperature is 38 C (100.4 F), blood pressure is 170/100 mm Hg, and pulse is 70/min. On physical examination, the patient is somnolent but arousable. She withdraws from painful stimuli applied to her right side but not to her left. Noncontrast CT scan of the head is shown in the image below:  Which of the following is the most likely underlying cause of this patient's current condition?
Which of the following is the most likely underlying cause of this patient's current condition?
A)Amyloid angiopathy
B)Arteriovenous malformation rupture
C)Bridging vein tear
D)Meningeal artery tear
E)Saccular aneurysm rupture
 Which of the following is the most likely underlying cause of this patient's current condition?
Which of the following is the most likely underlying cause of this patient's current condition?A)Amyloid angiopathy
B)Arteriovenous malformation rupture
C)Bridging vein tear
D)Meningeal artery tear
E)Saccular aneurysm rupture

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
64
A 57-year-old man comes to the office due to several months of progressive difficulty walking. Lately, weakness and stiffness in both legs has made it difficult to ambulate without support. The patient also has numbness and tingling in his arms and legs. His medical history includes hypertension and hyperlipidemia. The patient has smoked a pack of cigarettes daily for 30 years and has used injection drugs in the past. He has had several sexual partners. Temperature is 36.6 C (97.9 F), blood pressure is 140/90 mm Hg, and pulse is 78/min. Physical examination shows normal mental status and cranial nerves. There is mild weakness and atrophy of the upper arm muscles with decreased triceps reflex. Bilateral lower extremity strength is 4/5. Vibratory and pain sensation is decreased in both the hands and legs. Babinski sign is upgoing bilaterally. Further evaluation of this patient is most likely to reveal which of the following?
A)Advanced spondylosis of the cervical spine on radiography
B)Elevated protein level with normal cell count on cerebrospinal fluid analysis
C)Epidural fluid collection near the cervical spine on MRI
D)Frontoparietal parasagittal meningioma of the brain on MRI
E)Intramedullary cavity of the cervical spine on MRI
A)Advanced spondylosis of the cervical spine on radiography
B)Elevated protein level with normal cell count on cerebrospinal fluid analysis
C)Epidural fluid collection near the cervical spine on MRI
D)Frontoparietal parasagittal meningioma of the brain on MRI
E)Intramedullary cavity of the cervical spine on MRI

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
65
A 11-year-old girl is brought to the office due to a 2-day history of rapid-onset, abnormal movements of the body. The abnormal movements began bilaterally in the upper limbs, followed by the trunk and then lower extremities. As a result, the patient has had difficulty performing daily activities such as bathing and eating. However, she has no abnormal movements during sleep. Vital signs are normal. Examination shows a restless child with irregular, jerky movements involving the entire body and generalized hypotonia. Mental status examination, cranial nerves, and sensations are normal. Which of the following is the best next step in diagnosis?
A)Antistreptolysin O titer
B)Cerebrospinal fluid analysis
C)Psychiatric assessment
D)Serum calcium measurement
E)Serum ferritin level
F)Serum TSH measurement
A)Antistreptolysin O titer
B)Cerebrospinal fluid analysis
C)Psychiatric assessment
D)Serum calcium measurement
E)Serum ferritin level
F)Serum TSH measurement

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
66
A 26-year-old woman comes to the office due to eye problems. One week ago while driving, her eyes closed spontaneously after she looked at the headlights of an oncoming car. She briefly could not open her eyes and had to stop driving until the symptoms gradually improved over several minutes. Since then, she has had 3 similar episodes brought on by bright light exposure. The patient has had no fever, eye pain or discharge, blurry or double vision, headaches, or extremity weakness or numbness. She has a history of asymptomatic sarcoidosis and takes no medications. Vital signs are within normal limits. On physical examination, there is no facial asymmetry. Frequent blinking of the eyes is noted, and shining light in the eyes to assess pupillary response causes involuntary tonic closure of the eyelids bilaterally. The remainder of the examination is normal. Which of the following is the most likely diagnosis?
A)Acute uveitis
B)Focal dystonia
C)Myasthenia gravis
D)Myotonic dystrophy
E)Trigeminal neuralgia
A)Acute uveitis
B)Focal dystonia
C)Myasthenia gravis
D)Myotonic dystrophy
E)Trigeminal neuralgia

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
67
A 67-year-old man is brought to the emergency department due to right-sided weakness, numbness, and slurred speech. The patient was in his usual state of health last night but awoke this morning with these symptoms. He has a history of hypertension, hyperlipidemia, type 2 diabetes mellitus, and peripheral arterial disease. The patient does not drink alcohol regularly but has a 45-pack-year history. Physical examination shows an awake and alert patient with right-sided weakness, hemisensory loss, homonymous hemianopsia, and aphasia. CT scan of the head reveals a large left hemispheric infarction due to an occluded middle cerebral artery. The patient is hospitalized but is not treated with fibrinolytic therapy or mechanical thrombectomy due to ineligibility. Forty-eight hours later, he becomes obtunded. Temperature is 38.3 C (100.9 F), blood pressure is 154/86 mm Hg, and pulse is 64/min. Physical examination now shows complete right hemiplegia and deviation of the eyes to the left. Which of the following is the best next step in management of this patient?
A)Blood cultures and empiric antibiotics
B)Intravenous hypertonic saline and observation
C)Intravenous mannitol and observation
D)MRI of the head
E)Repeat CT scan of the head
A)Blood cultures and empiric antibiotics
B)Intravenous hypertonic saline and observation
C)Intravenous mannitol and observation
D)MRI of the head
E)Repeat CT scan of the head

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
68
A 68-year-old woman is admitted to the hospital due to a femoral neck fracture after a traumatic fall. The fracture is repaired, and her pain is treated with as-needed opioid medications. Over the course of her hospitalization, the patient develops nocturnal disorientation and mild agitation. Her husband says she is not like this at home. During morning rounds, the patient is pleasant and answers questions appropriately. Her condition resolves over the next few days, and she is discharged to the rehabilitation facility on day 7. Because of this patient's mental status changes, she is at increased risk for which of the following?
A)Acute mania
B)Cognitive decline
C)Depression with psychotic features
D)Nonconvulsive epilepsy
E)Opioid dependence
A)Acute mania
B)Cognitive decline
C)Depression with psychotic features
D)Nonconvulsive epilepsy
E)Opioid dependence

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
69
A 12-year-old boy is brought to the emergency department by his parents as "he cannot walk anymore." The patient has had a pins-and-needles sensation and weakness in both feet for the past few days. This morning, he could not stand or move his legs and has bilateral thigh pain. Two weeks ago, the patient had a febrile diarrheal illness that resolved on its own. He has had no headaches, nausea, vomiting, or recurrent diarrhea. He and his family are vegetarians, and they recently visited a petting zoo. The patient has no significant past medical history, and vaccinations are up to date. On arrival, temperature is 36.7 C (98.1 F), blood pressure is 150/90 mm Hg, pulse is 92/min, and respirations are 16/min; pulse oximetry is 99% on room air. Physical examination shows symmetric flaccid paralysis of the lower extremities and absent ankle and patellar deep tendon reflexes. Sensation is intact to light touch in both legs. The upper extremities are weak and hyporeflexic. There is no photophobia or nuchal rigidity. Which of the following structures is primarily impaired in this patient's condition?
A)Anterior horn cells
B)Dorsal and lateral spinal columns
C)Muscle fibers
D)Neuromuscular junction
E)Peripheral nerve fibers
A)Anterior horn cells
B)Dorsal and lateral spinal columns
C)Muscle fibers
D)Neuromuscular junction
E)Peripheral nerve fibers

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
70
A 34-year-old man comes to the emergency department due to progressive leg weakness for the past several days. He also reports a tingling sensation in the toes and mild low back pain. Three weeks ago, the patient was evaluated for flulike illness, oral ulcer, and lymphadenopathy and was diagnosed with HIV infection. He has not started antiretroviral therapy yet while waiting for drug resistance testing results. Temperature is 37 C (98.6 F), blood pressure is 120/70 mm Hg, and pulse is 72/min. Lower extremity examination shows marked muscle weakness and loss of deep tendon reflexes bilaterally. Touch, pain, and vibration sensations are intact. Upper extremity examination shows no abnormality. There is no focal back tenderness and no signs of meningeal irritation are present. Which of the following would be most helpful in revealing the cause of this patient's weakness?
A)Cerebrospinal fluid PCR
B)CT scan of the head
C)Nerve conduction studies
D)Toxoplasma serology
E)Tuberculin skin testing
A)Cerebrospinal fluid PCR
B)CT scan of the head
C)Nerve conduction studies
D)Toxoplasma serology
E)Tuberculin skin testing

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
71
A 58-year-old woman comes to the emergency department due to several hours of severe left-sided headache, nausea, and vomiting. She also has blurred vision and sees halos around lights. The patient has a history of hand tremors for which she recently started taking a new medication. She previously smoked, but does not use alcohol or illicit drugs. Temperature is 37 C (98.6 F), blood pressure is 150/90 mm Hg, and pulse is 96/min. The patient is in severe distress. Physical examination reveals left eye circum-corneal injection with a dilated and sluggish pupil. Visual acuity is decreased in the left eye. She has resting hand tremors and increased resistance to passive movements of the extremities. Which of the following medications is most likely causing her current symptoms?
A)Entacapone
B)Levodopa/carbidopa
C)Pramipexole
D)Propranolol
E)Selegiline
F)Trihexyphenidyl
A)Entacapone
B)Levodopa/carbidopa
C)Pramipexole
D)Propranolol
E)Selegiline
F)Trihexyphenidyl

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
72
A 16-year-old previously healthy boy is brought to the emergency department 30 minutes after a head injury. He was playing football when he had a helmet-to-helmet impact with another player. The patient was dazed and disoriented for several minutes after the incident but did not lose consciousness. He stumbled and fell after getting up. The patient is now awake and alert and reports mild headache but no nausea, vision changes, or other subjective neurologic deficits. Vital signs are within normal limits. On physical examination, he appears tired. There is no obvious head deformity. The pupils are equal and reactive, and there is no facial droop. Bilateral upper and lower extremity muscle strength, deep tendon reflexes, and sensation are normal. Which of the following is the most likely cause of this patient's symptoms?
A)Disruption of white matter tracts
B)Fracture of bone at the base of the skull
C)Neuronal functional disturbance
D)Rupture of the middle meningeal artery
E)Tearing of the bridging veins
A)Disruption of white matter tracts
B)Fracture of bone at the base of the skull
C)Neuronal functional disturbance
D)Rupture of the middle meningeal artery
E)Tearing of the bridging veins

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
73
A 42-year-old previously healthy woman comes to the office due to worsening double vision and gait unsteadiness. She states she had cramping abdominal pain and diarrhea 2 weeks ago after an outdoor picnic, which spontaneously resolved after 3 days. The double vision began 4 days ago and is persistent and progressive. The patient has also been stumbling while walking due to incoordination. She has had no fever, headache, neck pain, photophobia, or bowel or bladder dysfunction. The patient does not use tobacco, alcohol, or illicit drugs. Vital signs are within normal limits. On physical examination, she is fully alert and oriented with normal memory, speech, and language comprehension. There is mild ptosis of the right eye with weakness of the medial and upward gaze. Left eye movements are normal. Bilateral lower-extremity weakness with loss of deep tendon reflexes is present. There is dysmetria on heel-to-shin testing on both sides. Bilateral upper-extremity muscle strength, reflexes, and coordination are normal. Sensation to touch and pinprick is normal throughout. The remainder of the examination shows no abnormalities. Which of the following is the most likely cause of this patient's current condition?
A)Botulinum toxin ingestion
B)Dietary thiamine deficiency
C)Immune-mediated nerve injury
D)Neuroinvasive virus infection
E)Vertebrobasilar artery occlusion
A)Botulinum toxin ingestion
B)Dietary thiamine deficiency
C)Immune-mediated nerve injury
D)Neuroinvasive virus infection
E)Vertebrobasilar artery occlusion

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
74
A 38-year-old woman comes to the emergency department due to 2 hours of left leg weakness and numbness. Over the last 3 months, the patient has had several similar episodes in which her left foot tingles and becomes numb and her entire left foot becomes limp, causing her to trip. The symptoms resolve spontaneously within a few hours. Her right leg has never displayed similar symptoms. The patient has no significant medical history but does have a family history of multiple sclerosis. She does not use tobacco, alcohol, or illicit drugs. The patient has experienced major psychosocial stress after losing her job 6 months ago, but this has tempered somewhat since she joined a meditation group. Vital signs are within normal limits. Physical examination shows diminished pinprick sensation over the dorsum of the left foot and weakness of the left big toe on extension. The patient is able to walk on her left toes but not on her left heel. Which of the following is the most likely cause of this patient's current symptoms?
A)Myoneural junction dysfunction
B)Peripheral nerve compression
C)Primary psychiatric disorder
D)Spinal artery atherothrombosis
E)Spinal nerve root entrapment
F)Subcortical white matter demyelination
G)Transient frontoparietal ischemia
A)Myoneural junction dysfunction
B)Peripheral nerve compression
C)Primary psychiatric disorder
D)Spinal artery atherothrombosis
E)Spinal nerve root entrapment
F)Subcortical white matter demyelination
G)Transient frontoparietal ischemia

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
75
A 52-year-old man comes to the office due to upper extremity weakness and pain in his shoulders and upper back since shoveling snow 3 weeks ago. His left arm also has started to feel heavy, and he has difficulty dressing and undressing because he lacks the strength to pull clothes over his head. The patient has not had similar symptoms before and recalls no other trauma to the area. He has a history of hypertension and hypothyroidism. Vital signs are within normal limits. Physical examination of the shoulder joints shows no deformity, and passive range of motion is full with no pain. There is moderate weakness of left shoulder abduction, but strength in the other muscle groups is normal. Decreased sensation to light touch and pinprick is present on the left lateral forearm. The remainder of the examination shows no abnormalities. Which of the following is the most appropriate next step in evaluation of this patient's symptoms?
A)CT scan of the brain
B)MRI of the cervical spine
C)MRI of the shoulder joint
D)Nerve conduction studies
E)TSH and creatine kinase levels
A)CT scan of the brain
B)MRI of the cervical spine
C)MRI of the shoulder joint
D)Nerve conduction studies
E)TSH and creatine kinase levels

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
76
A 14-year-old girl is brought to the emergency department due to progressive weakness in the lower limbs for 3 weeks. Her parents first noticed clumsiness, which has progressed to difficulty walking over the last week. The patient had a fever, cough, and congestion about 1 month ago and has otherwise been well. She has a history of high plantar arches requiring orthotics and mild scoliosis. The patient takes no medication and has no allergies. Her parents and 2 older siblings are healthy. Vital signs are normal. On examination, she has a wide-based gait and has difficulty maintaining balance without assistance. Strength is 2/5 in the lower extremities and 5/5 in the upper extremities. There is decreased vibratory and position sense in the lower extremities. MRI shows cervical spinal cord atrophy. When discussing the most likely diagnosis with the patient's parents, which of the following statements is most accurate?
A)A predisposition to malignancy is typical of this progressive disease.
B)Anti-viral therapy will reduce symptoms.
C)Genetic testing is recommended to confirm the diagnosis.
D)This chronic condition typically stabilizes with disease-modifying therapies.
E)This is a nonprogressive condition that usually improves with supportive care.
A)A predisposition to malignancy is typical of this progressive disease.
B)Anti-viral therapy will reduce symptoms.
C)Genetic testing is recommended to confirm the diagnosis.
D)This chronic condition typically stabilizes with disease-modifying therapies.
E)This is a nonprogressive condition that usually improves with supportive care.

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
77
A 45-year-old, previously healthy man comes to the office due to worsening extremity weakness and numbness. Three months ago, the patient began experiencing numbness and weakness in both feet that made it difficult to climb stairs or stand up from a seated position. Two weeks later, he noticed weakness of his grip strength bilaterally but had no difficulty lifting his arms. The muscle weakness has been slowly progressing, and the patient now has difficulty buttoning his clothes, turning doorknobs, and walking on a level surface. He does not use tobacco or illicit drugs and drinks alcohol occasionally. Vital signs are within normal limits. Physical examination shows weakness of the small muscles of the hands and the hip girdle muscles bilaterally. Deep tendon reflexes are diffusely diminished, and there is loss of vibration and position sensation in the toes bilaterally. Which of the following findings is most likely to be associated with this patient's current symptoms?
A)Autoantibodies against voltage-gated calcium channel
B)Decreased peripheral nerve conduction velocity
C)Demyelinating plaques in the brain and spinal cord
D)Increased serum methylmalonic acid level
E)Inflammatory infiltrates and necrosis of myofibers
A)Autoantibodies against voltage-gated calcium channel
B)Decreased peripheral nerve conduction velocity
C)Demyelinating plaques in the brain and spinal cord
D)Increased serum methylmalonic acid level
E)Inflammatory infiltrates and necrosis of myofibers

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
78
A 2-month-old boy is brought to the emergency department by ambulance after a seizure. His mother says that he rolled off the bed last night while his older sister was changing his clothes and that he cried for a few minutes but fed well last night. Today, the patient had a tonic-clonic seizure that lasted 4 minutes after his morning feeding. He has been otherwise healthy. The patient was born at 31 weeks gestation, and his postnatal course was complicated by respiratory distress and hypoxia requiring intubation for several days. Height and weight are at the 50th percentile; head circumference is at the 98th percentile. Temperature is 36.7 C (98 F), blood pressure is 90/50 mm Hg, and pulse is 144/min. Physical examination shows a limp infant who withdraws from painful stimuli. The anterior fontanelle is full and tense. Funduscopy reveals bilateral papilledema and retinal hemorrhages. The abdomen is soft with no hepatosplenomegaly. Which of the following is the most likely etiology of this patient's seizure?
A)Cerebrospinal fluid obstruction
B)Electrolyte abnormality
C)Hypoxic encephalopathy
D)Meningeal inflammation
E)Subdural venous shearing
F)Thromboembolism formation
A)Cerebrospinal fluid obstruction
B)Electrolyte abnormality
C)Hypoxic encephalopathy
D)Meningeal inflammation
E)Subdural venous shearing
F)Thromboembolism formation

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
79
A 7-year-old girl is brought to clinic due to a diffuse headache. She first developed pain while working on a math assignment today. The headache was exacerbated by the sound of her classmates yelling at recess. She was permitted to lie down in a dark, quiet room, which helped. The patient had just returned to school today after a vacation, during which she hit her head on the passenger door when her mother's car collided with another car. The patient did not lose consciousness and was taken to the emergency department, where head imaging was normal. Since the incident, she has been more irritable at times. Vitals signs are normal. The patient has a normal affect and can easily recall details of the accident. Examination shows return of headache when asked to move her eyes left and right rapidly between 2 points held a short distance away. Neurologic examination is otherwise normal. Which of the following is the most likely cause of this patient's symptoms?
A)Acute stress disorder
B)Concussion
C)Migraine headache
D)Perilymphatic fistula
E)Tension headache
A)Acute stress disorder
B)Concussion
C)Migraine headache
D)Perilymphatic fistula
E)Tension headache

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck
80
A 50-year-old woman is brought to the emergency department after suddenly experiencing right upper and lower extremity weakness while jogging on a treadmill. Her weakness gradually worsened over the next hour, and she had severe headache, nausea, and vomiting. The patient has a history of chronic hypertension but stopped taking antihypertensives several months ago. She does not use tobacco but drinks 1 or 2 glasses of wine on weekends. Blood pressure is 230/112 mm Hg and pulse is 76/min and regular. On physical examination, the patient is stuporous and responds to painful stimuli only. There is right hemiplegia, right hemisensory loss, and leftward deviation of the eyes. Which of the following is the most likely diagnosis?
A)Cerebellar hemorrhage
B)Cortical ischemic infarction
C)Medullary ischemic infarction
D)Putaminal hemorrhage
E)Subarachnoid hemorrhage
A)Cerebellar hemorrhage
B)Cortical ischemic infarction
C)Medullary ischemic infarction
D)Putaminal hemorrhage
E)Subarachnoid hemorrhage

Unlock Deck
Unlock for access to all 723 flashcards in this deck.
Unlock Deck
k this deck



