Deck 3: Psychiatry
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question

Unlock Deck
Sign up to unlock the cards in this deck!
Unlock Deck
Unlock Deck
1/336
Play
Full screen (f)
Deck 3: Psychiatry
1
A 27-year-old man comes to the office for postdischarge follow-up of a recent psychiatric hospitalization for a depressive episode with suicidal ideation. The patient's depressive episode remitted with intensive inpatient psychotherapy and the initiation of a new medication regimen 1 month ago. The patient has been home for a week and is feeling well. He has a history of migraine headaches, bipolar disorder, and tobacco use disorder. Family history is significant for major depressive disorder in his father. Temperature is 37.5 C (99.5 F), blood pressure is 110/75 mm Hg, pulse is 72/min, and respirations are 14/min. Examination is significant for a maculopapular rash over the patient's left scapula. The patient is unaware of the rash, and discharge paperwork from the previous week does not document any rash. Which of the following medications is the most likely cause of this patient's condition?
A)Escitalopram
B)Haloperidol
C)Lamotrigine
D)Lurasidone
E)Olanzapine
F)Quetiapine
G)Sertraline
A)Escitalopram
B)Haloperidol
C)Lamotrigine
D)Lurasidone
E)Olanzapine
F)Quetiapine
G)Sertraline
C
Explanation:
The anticonvulsant lamotrigine is used as a mood stabilizer in bipolar disorder and is often used specifically to target bipolar depression. One of the most significant side effects of lamotrigine is a drug rash, a mild form of which occurs in up to 10% of those treated. The more severe mucocutaneous rashes of Stevens-Johnson syndrome (<10% body surface area skin detachment) and toxic epidermal necrolysis (>30% detachment) occur at a rate of 0.1% (10%-30% detachment is known as Stevens-Johnson syndrome/toxic epidermal necrolysis overlap).
Because of the challenge of predicting the eventual severity of lamotrigine-induced rash at the outset, lamotrigine should be discontinued at the first sign of rash and substituted with another agent. Most cases of lamotrigine-induced rash develop within the first 2 months of therapy. Risk of rash is greater in children and appears to be higher when coprescribed with valproate or when the dose is increased rapidly.
(Choices A and G) Antidepressants such as the selective serotonin reuptake inhibitors escitalopram and sertraline should be used with caution in bipolar depression, given the limited evidence of benefit and the risk of mood-switching from depression to mania. Neither escitalopram nor sertraline is associated with a significant risk of rash.
(Choices B, D, E, and F) Haloperidol, lurasidone, olanzapine, and quetiapine are all antipsychotic medications that may be used in the treatment of bipolar disorder; however, none are associated with a clinically significant risk of rash.
Educational objective:
A mild rash may develop in up to 10% of those treated with lamotrigine, whereas life-threatening Stevens-Johnson syndrome or toxic epidermal necrolysis may occur in 0.1%. Any occurrence of rash during the treatment of lamotrigine requires immediate discontinuation of the drug.
References:
Risk of a lamotrigine-related skin rash: current meta-analysis and postmarketing cohort analysis.
(http://www.ncbi.nlm.nih.gov/pubmed/25645637)
Management of adverse effects of mood stabilizers.
(http://www.ncbi.nlm.nih.gov/pubmed/26084665)
Explanation:
The anticonvulsant lamotrigine is used as a mood stabilizer in bipolar disorder and is often used specifically to target bipolar depression. One of the most significant side effects of lamotrigine is a drug rash, a mild form of which occurs in up to 10% of those treated. The more severe mucocutaneous rashes of Stevens-Johnson syndrome (<10% body surface area skin detachment) and toxic epidermal necrolysis (>30% detachment) occur at a rate of 0.1% (10%-30% detachment is known as Stevens-Johnson syndrome/toxic epidermal necrolysis overlap).
Because of the challenge of predicting the eventual severity of lamotrigine-induced rash at the outset, lamotrigine should be discontinued at the first sign of rash and substituted with another agent. Most cases of lamotrigine-induced rash develop within the first 2 months of therapy. Risk of rash is greater in children and appears to be higher when coprescribed with valproate or when the dose is increased rapidly.
(Choices A and G) Antidepressants such as the selective serotonin reuptake inhibitors escitalopram and sertraline should be used with caution in bipolar depression, given the limited evidence of benefit and the risk of mood-switching from depression to mania. Neither escitalopram nor sertraline is associated with a significant risk of rash.
(Choices B, D, E, and F) Haloperidol, lurasidone, olanzapine, and quetiapine are all antipsychotic medications that may be used in the treatment of bipolar disorder; however, none are associated with a clinically significant risk of rash.
Educational objective:
A mild rash may develop in up to 10% of those treated with lamotrigine, whereas life-threatening Stevens-Johnson syndrome or toxic epidermal necrolysis may occur in 0.1%. Any occurrence of rash during the treatment of lamotrigine requires immediate discontinuation of the drug.
References:
Risk of a lamotrigine-related skin rash: current meta-analysis and postmarketing cohort analysis.
(http://www.ncbi.nlm.nih.gov/pubmed/25645637)
Management of adverse effects of mood stabilizers.
(http://www.ncbi.nlm.nih.gov/pubmed/26084665)
2
A 39-year-old woman is hospitalized for appendicitis and undergoes an appendectomy on hospital day 1. The patient has an uncomplicated postoperative course until the morning of hospital day 3, when she suddenly becomes acutely agitated. She tries to get out of bed and shouts, "Get your hands off me! God is watching!" when the nurses try to redirect her back into bed. The patient has a history of schizophrenia, hypertension, multiple substance use disorders, and homelessness. Medical records indicate that she was treated for a heroin and cocaine overdose last year and has had multiple admissions related to her substance use. Temperature is 39 C (102.2 F), blood pressure is 171/95 mm Hg, pulse is 102/min, and respirations are 18/min. The patient is oriented only to person. She is diaphoretic, but the remainder of the examination is limited due to agitation. Which of the following is the most likely cause of this patient's condition?
A)Abdominal compartment syndrome
B)Acute schizophrenia exacerbation
C)Alcohol withdrawal
D)Cocaine intoxication
E)Malignant hyperthermia
F)Opioid withdrawal
G)Postoperative encephalopathy
H)Pulmonary embolism
A)Abdominal compartment syndrome
B)Acute schizophrenia exacerbation
C)Alcohol withdrawal
D)Cocaine intoxication
E)Malignant hyperthermia
F)Opioid withdrawal
G)Postoperative encephalopathy
H)Pulmonary embolism
C
Explanation:
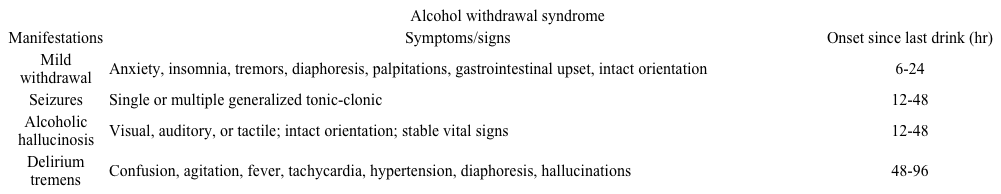 This patient's delayed onset (>48 hours) of severe delirium, elevated vital signs (eg, hyperthermia, hypertension, tachycardia), and diaphoresis in the setting of known multiple substance use disorders is consistent with a diagnosis of delirium tremens (DT). DT is a late complication of alcohol withdrawal that may affect up to 5% of patients who experience an initial milder withdrawal syndrome. DT does not present before 48 hours after the last drink, but symptoms may take as long as 96 hours to be seen. These symptoms may persist for up to 5 days and are associated with a mortality rate of up to 5%.
This patient's delayed onset (>48 hours) of severe delirium, elevated vital signs (eg, hyperthermia, hypertension, tachycardia), and diaphoresis in the setting of known multiple substance use disorders is consistent with a diagnosis of delirium tremens (DT). DT is a late complication of alcohol withdrawal that may affect up to 5% of patients who experience an initial milder withdrawal syndrome. DT does not present before 48 hours after the last drink, but symptoms may take as long as 96 hours to be seen. These symptoms may persist for up to 5 days and are associated with a mortality rate of up to 5%.
Treatment of DT is similar to milder forms of alcohol withdrawal in that benzodiazepines (eg, lorazepam, diazepam) are the pharmacologic treatment of choice; however, the treatment of DT invariably requires intensive care unit-level supportive management.
(Choice A) Abdominal compartment syndrome presents with wide-ranging organ dysfunction (eg, decreased cardiac output, increased intracranial pressure, renal impairment) in patients with increased intra-abdominal pressure secondary to large-volume resuscitation, burns, or other abdominal conditions (eg, ascites, liver transplantation).
(Choice B) Patients with an exacerbation of schizophrenia are typically not disoriented. This patient's agitation and bizarre statements may be influenced by the psychopathology of schizophrenia, but her disorientation, elevated vital signs, and overall clinical picture are better explained by DT.
(Choice D) Cocaine intoxication may present with euphoria; autonomic hyperactivity (eg, tachycardia, hypertension); and, at higher doses, psychosis. This patient's delirium, timing of symptom onset, and overall clinical picture are more consistent with alcohol withdrawal.
(Choice E) Malignant hyperthermia is characterized by rigidity, rhabdomyolysis, hyperthermia, and tachycardia immediately following the administration of succinylcholine or a volatile inhaled anesthetic (eg, halothane, sevoflurane) in susceptible individuals (susceptibility is inherited in an autosomal dominant pattern).
(Choice F) The timing of opioid withdrawal depends on the half-life of the specific opioid being used (eg, heroin withdrawal begins approximately 12 hours after last use) and consists of gastrointestinal distress, myalgias, rhinorrhea, diaphoresis, and mild elevations of heart rate and blood pressure. The onset of symptoms after 48 hours, delirium, and severity of this patient's elevated vital signs are more consistent with alcohol withdrawal and DT.
(Choice G) Postoperative encephalopathy is most commonly associated with cardiac surgery and presents with delirium and/or seizures in the immediate postoperative period.
(Choice H) Pulmonary embolism may present in the postoperative period with dyspnea and chest pain.
Educational objective:
Delirium tremens is a late manifestation of alcohol withdrawal that is characterized by delirium, hyperthermia, hypertension, and tachycardia 48-96 hours after the last drink. Delirium tremens is associated with a mortality rate of 5% and requires aggressive intensive care unit-level supportive management in addition to benzodiazepine therapy.
References:
Identification and management of alcohol withdrawal syndrome.
(http://www.ncbi.nlm.nih.gov/pubmed/25666543)
Alcohol withdrawal delirium-diagnosis, course and treatment.
(http://www.ncbi.nlm.nih.gov/pubmed/24399242)
The emergency medicine management of severe alcohol withdrawal.
(http://www.ncbi.nlm.nih.gov/pubmed/28188055)
Explanation:
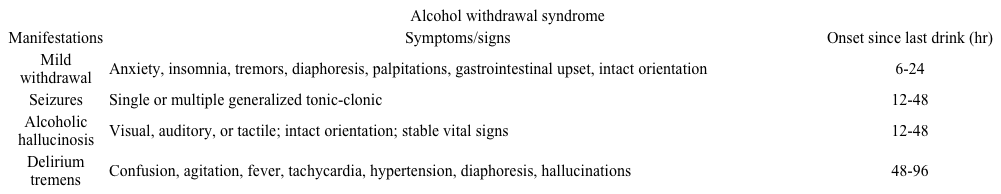 This patient's delayed onset (>48 hours) of severe delirium, elevated vital signs (eg, hyperthermia, hypertension, tachycardia), and diaphoresis in the setting of known multiple substance use disorders is consistent with a diagnosis of delirium tremens (DT). DT is a late complication of alcohol withdrawal that may affect up to 5% of patients who experience an initial milder withdrawal syndrome. DT does not present before 48 hours after the last drink, but symptoms may take as long as 96 hours to be seen. These symptoms may persist for up to 5 days and are associated with a mortality rate of up to 5%.
This patient's delayed onset (>48 hours) of severe delirium, elevated vital signs (eg, hyperthermia, hypertension, tachycardia), and diaphoresis in the setting of known multiple substance use disorders is consistent with a diagnosis of delirium tremens (DT). DT is a late complication of alcohol withdrawal that may affect up to 5% of patients who experience an initial milder withdrawal syndrome. DT does not present before 48 hours after the last drink, but symptoms may take as long as 96 hours to be seen. These symptoms may persist for up to 5 days and are associated with a mortality rate of up to 5%.Treatment of DT is similar to milder forms of alcohol withdrawal in that benzodiazepines (eg, lorazepam, diazepam) are the pharmacologic treatment of choice; however, the treatment of DT invariably requires intensive care unit-level supportive management.
(Choice A) Abdominal compartment syndrome presents with wide-ranging organ dysfunction (eg, decreased cardiac output, increased intracranial pressure, renal impairment) in patients with increased intra-abdominal pressure secondary to large-volume resuscitation, burns, or other abdominal conditions (eg, ascites, liver transplantation).
(Choice B) Patients with an exacerbation of schizophrenia are typically not disoriented. This patient's agitation and bizarre statements may be influenced by the psychopathology of schizophrenia, but her disorientation, elevated vital signs, and overall clinical picture are better explained by DT.
(Choice D) Cocaine intoxication may present with euphoria; autonomic hyperactivity (eg, tachycardia, hypertension); and, at higher doses, psychosis. This patient's delirium, timing of symptom onset, and overall clinical picture are more consistent with alcohol withdrawal.
(Choice E) Malignant hyperthermia is characterized by rigidity, rhabdomyolysis, hyperthermia, and tachycardia immediately following the administration of succinylcholine or a volatile inhaled anesthetic (eg, halothane, sevoflurane) in susceptible individuals (susceptibility is inherited in an autosomal dominant pattern).
(Choice F) The timing of opioid withdrawal depends on the half-life of the specific opioid being used (eg, heroin withdrawal begins approximately 12 hours after last use) and consists of gastrointestinal distress, myalgias, rhinorrhea, diaphoresis, and mild elevations of heart rate and blood pressure. The onset of symptoms after 48 hours, delirium, and severity of this patient's elevated vital signs are more consistent with alcohol withdrawal and DT.
(Choice G) Postoperative encephalopathy is most commonly associated with cardiac surgery and presents with delirium and/or seizures in the immediate postoperative period.
(Choice H) Pulmonary embolism may present in the postoperative period with dyspnea and chest pain.
Educational objective:
Delirium tremens is a late manifestation of alcohol withdrawal that is characterized by delirium, hyperthermia, hypertension, and tachycardia 48-96 hours after the last drink. Delirium tremens is associated with a mortality rate of 5% and requires aggressive intensive care unit-level supportive management in addition to benzodiazepine therapy.
References:
Identification and management of alcohol withdrawal syndrome.
(http://www.ncbi.nlm.nih.gov/pubmed/25666543)
Alcohol withdrawal delirium-diagnosis, course and treatment.
(http://www.ncbi.nlm.nih.gov/pubmed/24399242)
The emergency medicine management of severe alcohol withdrawal.
(http://www.ncbi.nlm.nih.gov/pubmed/28188055)
3
A 57-year-old woman comes to the office with intermittent headaches, shoulder and neck pain, fatigue, and insomnia. The headaches sometimes interfere with the patient's ability to concentrate at work. The symptoms are not new but have worsened over the past 8 months due to the stress of starting a new job and placing her elderly mother in an assisted living facility. The patient lies awake at night worrying about her mother, her own health problems, and the finances of her 2 adult children, who are having difficulty supporting themselves. During the day, she is tired due to poor sleep and worries about her job performance. The patient has a history of hypertension, irritable bowel syndrome, and tension headaches. She drinks 1 or 2 glasses of wine before bedtime a few times per week to help her relax and fall asleep. Temperature is 36.7 C (98 F), blood pressure is 130/80 mm Hg, pulse is 88/min, and respirations are 16/min. Examination shows sweaty palms and mild, diffuse abdominal tenderness; no other abnormalities are noted. Complete blood count, chemistry panel, TSH, urinalysis, and ECG are normal. Which of the following is the most appropriate next step in management of this patient?
A)Begin clonazepam and supportive psychotherapy
B)Begin escitalopram and recommend cognitive-behavioral therapy
C)Obtain noncontrast CT scan of the head and neck
D)Obtain urinary fractionated catecholamines and metanephrines
E)Obtain urinary porphobilinogens
F)Reassure the patient that serious medical illness has been ruled out
G)Schedule monthly visits to monitor symptoms
A)Begin clonazepam and supportive psychotherapy
B)Begin escitalopram and recommend cognitive-behavioral therapy
C)Obtain noncontrast CT scan of the head and neck
D)Obtain urinary fractionated catecholamines and metanephrines
E)Obtain urinary porphobilinogens
F)Reassure the patient that serious medical illness has been ruled out
G)Schedule monthly visits to monitor symptoms
B
Explanation:
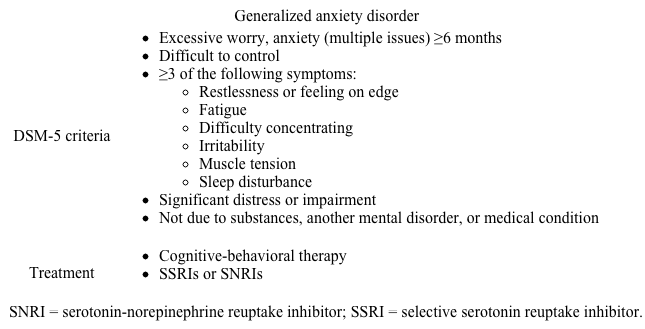 This patient's pain, insomnia, fatigue, and poor concentration are consistent with generalized anxiety disorder (GAD). Although excessive worry about multiple issues is the key symptom in GAD, patients frequently come to their primary care provider with somatic symptoms, including fatigue and physical symptoms related to muscular tension (eg, headaches; neck, shoulder, and back pain). Other physical manifestations of anxiety commonly seen in GAD include trembling, sweating, and gastrointestinal symptoms.
This patient's pain, insomnia, fatigue, and poor concentration are consistent with generalized anxiety disorder (GAD). Although excessive worry about multiple issues is the key symptom in GAD, patients frequently come to their primary care provider with somatic symptoms, including fatigue and physical symptoms related to muscular tension (eg, headaches; neck, shoulder, and back pain). Other physical manifestations of anxiety commonly seen in GAD include trembling, sweating, and gastrointestinal symptoms.
GAD typically has a lifelong, chronic course, with symptom severity increasing during periods of stress, as in this patient. GAD is effectively treated with a serotonergic antidepressant, cognitive-behavioral therapy (CBT), or a combination of the two.
(Choice A) Benzodiazepines are generally reserved for patients whose GAD symptoms persist despite treatment with a serotonergic antidepressant. These drugs are also less preferred in patients who have used alcohol to self-medicate. Supportive psychotherapy can be helpful but is not as effective as CBT.
(Choice C) An imaging study would be low yield in this patient, who has a known history of tension headaches, a common physical manifestation of GAD, and no focal neurological signs on examination.
(Choice D) Pheochromocytoma may cause anxiety. However, it is a rare disease that typically presents with paroxysmal symptoms and would not explain this patient's chronic anxiety about multiple issues.
(Choice E) Acute intermittent porphyria can result in autonomic arousal (eg, tachycardia, hypertension, sweating) as well as anxiety, but these symptoms tend to occur in acute attacks accompanied by neuropathy (eg, weakness, numbness) and severe abdominal pain.
(Choices F and G) Reassurance that serious medical illness has been ruled out and regularly scheduled visits are appropriate interventions for patients with somatic symptom disorder. In contrast to the generalized worries seen in GAD, patients with somatic symptom disorder have anxiety that specifically revolves around their somatic symptoms with the fear that they have a serious medical illness. This patient's somatic symptoms are a manifestation of GAD and should improve with effective treatment.
Educational objective:
Generalized anxiety disorder is characterized by excessive and persistent worry about multiple issues. Patients frequently come to their primary care provider with insomnia, fatigue, and physical symptoms related to muscular tension.
References:
Diagnosis and management of generalized anxiety disorder and panic disorder in adults.
(http://www.ncbi.nlm.nih.gov/pubmed/25955736)
The network structure of major depressive disorder, generalized anxiety disorder and somatic symptomatology.
(http://www.ncbi.nlm.nih.gov/pubmed/27523095)
Explanation:
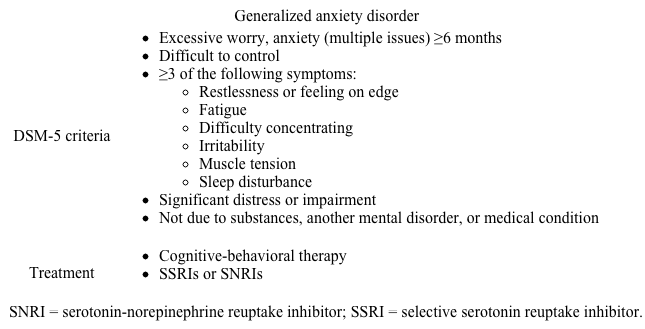 This patient's pain, insomnia, fatigue, and poor concentration are consistent with generalized anxiety disorder (GAD). Although excessive worry about multiple issues is the key symptom in GAD, patients frequently come to their primary care provider with somatic symptoms, including fatigue and physical symptoms related to muscular tension (eg, headaches; neck, shoulder, and back pain). Other physical manifestations of anxiety commonly seen in GAD include trembling, sweating, and gastrointestinal symptoms.
This patient's pain, insomnia, fatigue, and poor concentration are consistent with generalized anxiety disorder (GAD). Although excessive worry about multiple issues is the key symptom in GAD, patients frequently come to their primary care provider with somatic symptoms, including fatigue and physical symptoms related to muscular tension (eg, headaches; neck, shoulder, and back pain). Other physical manifestations of anxiety commonly seen in GAD include trembling, sweating, and gastrointestinal symptoms.GAD typically has a lifelong, chronic course, with symptom severity increasing during periods of stress, as in this patient. GAD is effectively treated with a serotonergic antidepressant, cognitive-behavioral therapy (CBT), or a combination of the two.
(Choice A) Benzodiazepines are generally reserved for patients whose GAD symptoms persist despite treatment with a serotonergic antidepressant. These drugs are also less preferred in patients who have used alcohol to self-medicate. Supportive psychotherapy can be helpful but is not as effective as CBT.
(Choice C) An imaging study would be low yield in this patient, who has a known history of tension headaches, a common physical manifestation of GAD, and no focal neurological signs on examination.
(Choice D) Pheochromocytoma may cause anxiety. However, it is a rare disease that typically presents with paroxysmal symptoms and would not explain this patient's chronic anxiety about multiple issues.
(Choice E) Acute intermittent porphyria can result in autonomic arousal (eg, tachycardia, hypertension, sweating) as well as anxiety, but these symptoms tend to occur in acute attacks accompanied by neuropathy (eg, weakness, numbness) and severe abdominal pain.
(Choices F and G) Reassurance that serious medical illness has been ruled out and regularly scheduled visits are appropriate interventions for patients with somatic symptom disorder. In contrast to the generalized worries seen in GAD, patients with somatic symptom disorder have anxiety that specifically revolves around their somatic symptoms with the fear that they have a serious medical illness. This patient's somatic symptoms are a manifestation of GAD and should improve with effective treatment.
Educational objective:
Generalized anxiety disorder is characterized by excessive and persistent worry about multiple issues. Patients frequently come to their primary care provider with insomnia, fatigue, and physical symptoms related to muscular tension.
References:
Diagnosis and management of generalized anxiety disorder and panic disorder in adults.
(http://www.ncbi.nlm.nih.gov/pubmed/25955736)
The network structure of major depressive disorder, generalized anxiety disorder and somatic symptomatology.
(http://www.ncbi.nlm.nih.gov/pubmed/27523095)
4
A 76-year-old man is brought to the office by his daughter due to disruptive behavior. Last night he behaved normally, took his regular medications, and retired to his bedroom shortly after dinner. When the patient emerged an hour later, he was agitated, irritable, and confused. When asked what was wrong, he became belligerent and seemed unable to recognize some family members. The daughter describes similar episodes over the past 3 evenings. Although the patient seems calmer and less confused this morning, the daughter worries that he will have another episode. His medical history is significant for essential hypertension, benign prostatic hyperplasia, mild neurocognitive disorder, insomnia, and a recent increase in anxiety related to stock market losses. Medications include terazosin and alprazolam. A thorough physical examination is unremarkable, with no focal neurologic findings. Laboratory evaluation, including complete blood count and serum electrolytes, is normal. Which of the following is the most appropriate next step in management of this patient?
A)Increase dose of alprazolam
B)Order CT scan of the brain
C)Prescribe donepezil
D)Prescribe quetiapine as needed
E)Taper and discontinue alprazolam
F)Taper and discontinue terazosin
A)Increase dose of alprazolam
B)Order CT scan of the brain
C)Prescribe donepezil
D)Prescribe quetiapine as needed
E)Taper and discontinue alprazolam
F)Taper and discontinue terazosin

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
5
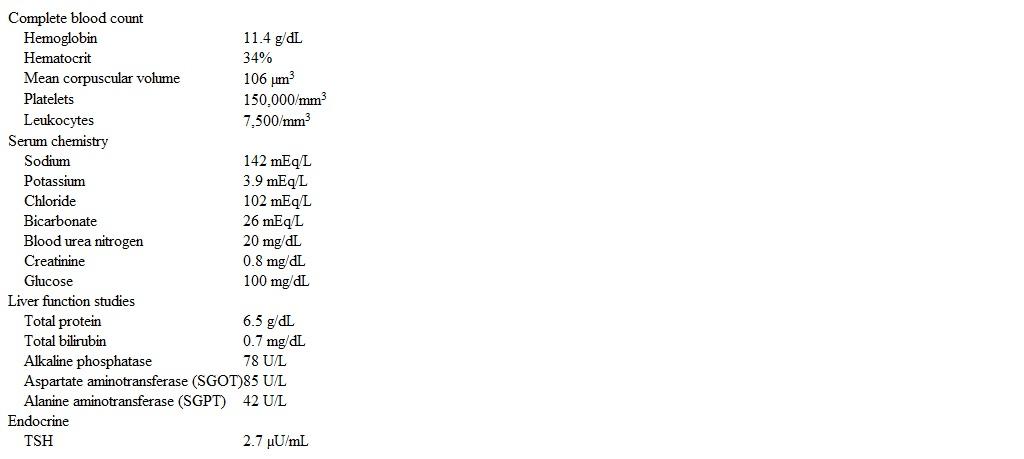
A 55-year-old woman comes to the office due to insomnia and fatigue that began shortly after her divorce was finalized a year ago. The patient used to sleep 7-8 hours without difficulty; however, over the past year she has had increasing difficulty falling asleep and started drinking 2-3 glasses of wine before bedtime to help. Despite falling asleep more quickly, she has recently started to regularly wake up around 3:00 AM. Her symptoms have progressively worsened and she now lies awake for several hours in the middle of the night, thinking and worrying about her future, but she rarely experiences anxiety during the day. She reports mild difficulty with concentration and no change in appetite. The patient experiences occasional brief sadness and loneliness. She has recently started showing up late for work and has stopped attending her weekly exercise class. Medical history includes hypothyroidism, treated with levothyroxine, and gastroesophageal reflux disease, diagnosed 3 months ago and treated with ranitidine. Temperature is 37.2 C (99 F), blood pressure is 140/90 mm Hg, pulse is 90/min, and respirations are 12/min. Physical examination shows a mild tremor but no other abnormalities. Laboratory results are as follows: 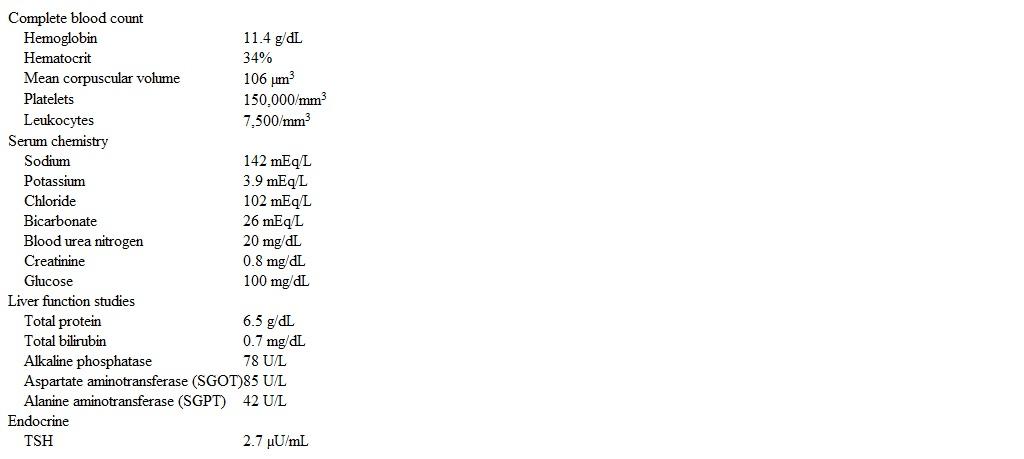 Which of the following is the most likely diagnosis in this patient?
Which of the following is the most likely diagnosis in this patient?
A)Adjustment disorder
B)Alcohol use disorder
C)Anxiety disorder due to another medical condition
D)Generalized anxiety disorder
E)Insomnia disorder
F)Persistent depressive disorder (dysthymia)
 Which of the following is the most likely diagnosis in this patient?
Which of the following is the most likely diagnosis in this patient?A)Adjustment disorder
B)Alcohol use disorder
C)Anxiety disorder due to another medical condition
D)Generalized anxiety disorder
E)Insomnia disorder
F)Persistent depressive disorder (dysthymia)

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
6
A 56-year-old woman comes to the office for a routine health maintenance evaluation. The patient is physically well but reports feeling upset that she had to place her 79-year-old father in a nursing home. She says, "I've cared for him since he developed Alzheimer disease 5 years ago, but I couldn't manage him at home anymore." The patient's medical conditions include hypertension and type 2 diabetes mellitus. She underwent menopause at age 51. She does not use tobacco or alcohol and takes yoga classes 3 times a week. Blood pressure is 140/85 mm Hg and pulse is 77/min. BMI is 32 kg/m2. Physical examination is unremarkable. The patient expresses concern about developing Alzheimer disease like her father and asks if there is anything to do. Which of the following is the most appropriate response to the patient?
A)"Although Alzheimer disease cannot be prevented, family history is only a risk factor if your father had the early-onset form of the disease."
B)"Although family history is a risk factor, taking supplements like vitamin E can help reduce your risk."
C)"I imagine it was difficult to watch your father decline, but there is nothing anyone can do to prevent Alzheimer disease from developing."
D)"I understand your concern and suggest getting an APOE genetic test to determine if you are at risk for Alzheimer disease."
E)"While family history is a risk factor for developing Alzheimer disease, getting good control of your medical conditions now can help reduce your risk."
A)"Although Alzheimer disease cannot be prevented, family history is only a risk factor if your father had the early-onset form of the disease."
B)"Although family history is a risk factor, taking supplements like vitamin E can help reduce your risk."
C)"I imagine it was difficult to watch your father decline, but there is nothing anyone can do to prevent Alzheimer disease from developing."
D)"I understand your concern and suggest getting an APOE genetic test to determine if you are at risk for Alzheimer disease."
E)"While family history is a risk factor for developing Alzheimer disease, getting good control of your medical conditions now can help reduce your risk."

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
7
A 73-year-old woman is seen in the hospital following emergent left transmetatarsal amputation. The patient has a history of chronic, nonhealing foot ulcers due to poorly controlled diabetes mellitus and peripheral artery disease and was admitted 2 days ago with wet gangrene and cellulitis. At the time of admission, she had fever, hypotension, and altered mental status, and consent for amputation was provided by her son who is her designated surrogate decision maker. Following surgery, the patient has been stabilized with intravenous antibiotics, opioid pain medications, and appropriate thromboembolism prophylaxis. When the vascular surgeon explains his recommendation for left lower extremity angiography and possible revascularization to prevent further amputation, the patient refuses the procedures. She says, "I'm too old for another operation. I didn't want surgery the first time, and I don't want it now." Which of the following is the most appropriate next step in management of this patient?
A)Ask the patient's son for consent to perform the procedure
B)Assess the patient for depressive symptoms
C)Check to see if the patient has a living will
D)Determine if the patient has capacity to refuse the procedure
E)Document the patient's refusal and do not perform the procedure
F)Obtain two-physician consent to perform the procedure
A)Ask the patient's son for consent to perform the procedure
B)Assess the patient for depressive symptoms
C)Check to see if the patient has a living will
D)Determine if the patient has capacity to refuse the procedure
E)Document the patient's refusal and do not perform the procedure
F)Obtain two-physician consent to perform the procedure

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
8
A 59-year-old woman comes to the office to follow up for chronic back pain caused by a motor vehicle collision. A month ago, the patient was given scheduled-dose oral morphine. Her pain level has decreased from 8 to 3 on a scale of 0-10, and pain no longer interferes with activities of daily living. There has been no drowsiness, constipation, or nausea. Other medications include naproxen, acetaminophen, and a lidocaine patch as needed. Temperature is 37 C (98.6 F), blood pressure is 114/76 mm Hg, pulse is 64/min, and respirations are 12/min. On examination, the back has greater range of motion than it did during the last visit. Which of the following would be most helpful in the early detection of prescription opioid misuse in this patient?
A)Assessing back range of motion at each visit
B)Assessing pain level at each visit
C)Monitoring vital signs at each visit
D)Obtaining a scheduled urine drug screening at each visit
E)Querying the prescription drug monitoring database at each visit
A)Assessing back range of motion at each visit
B)Assessing pain level at each visit
C)Monitoring vital signs at each visit
D)Obtaining a scheduled urine drug screening at each visit
E)Querying the prescription drug monitoring database at each visit

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
9
A 19-year-old woman comes to the university health center due to "feeling cold all the time." She wears sweaters despite the warm weather and sleeps with multiple blankets at night. The patient also states that she has had difficulty losing weight and wonders if a thyroid problem could be causing her symptoms. She says, "I go to the gym at least 5 times a week, but I feel like I'm stuck at the same weight. I've even cut bread from my diet because it was making me constipated." Menarche was at age 12, and the patient's last menstrual period was 2 months ago. Family history is significant for Graves disease in her mother and Sjögren syndrome in her maternal grandmother. Temperature is 36.2 C (97.2 F), blood pressure is 80/50 mm Hg, pulse is 38/min, and respirations are 16/min. BMI is 15 kg/m2. The patient is alert and cooperative but appears tired. Laboratory results are as follows:  Oral electrolyte supplements are administered. Which of the following is the best next step in management?
Oral electrolyte supplements are administered. Which of the following is the best next step in management?
A)Administer fluoxetine
B)Administer levothyroxine
C)Administer low-dose olanzapine
D)Admit to hospital
E)Refer for cognitive-behavioral therapy, with follow-up in 2 weeks
F)Refer for nutritional rehabilitation, with follow-up in 2 weeks
 Oral electrolyte supplements are administered. Which of the following is the best next step in management?
Oral electrolyte supplements are administered. Which of the following is the best next step in management?A)Administer fluoxetine
B)Administer levothyroxine
C)Administer low-dose olanzapine
D)Admit to hospital
E)Refer for cognitive-behavioral therapy, with follow-up in 2 weeks
F)Refer for nutritional rehabilitation, with follow-up in 2 weeks

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
10
A 32-year-old man comes to the office due to erectile dysfunction and decreased libido for the past month. The patient has never experienced these symptoms before and finds them to be very upsetting. He has no problems with urination. The patient has a history of schizophrenia and was discharged from a psychiatric hospital 3 months ago on risperidone. He has no current delusions, and his auditory hallucinations have decreased in frequency and intensity. His thoughts are well organized. Review of systems is negative except for a recent 3-kg (6.6-lb) weight gain. Physical examination shows bilateral breast enlargement. Which of the following is the most likely mechanism responsible for this patient's decreased libido?
A)Decreased dopamine activity in the mesolimbic pathway
B)Decreased dopamine activity in the nigrostriatal pathway
C)Decreased dopamine activity in the tuberoinfundibular pathway
D)Increased dopamine activity in the mesolimbic pathway
E)Increased dopamine activity in the nigrostriatal pathway
F)Increased dopamine activity in the tuberoinfundibular pathway
A)Decreased dopamine activity in the mesolimbic pathway
B)Decreased dopamine activity in the nigrostriatal pathway
C)Decreased dopamine activity in the tuberoinfundibular pathway
D)Increased dopamine activity in the mesolimbic pathway
E)Increased dopamine activity in the nigrostriatal pathway
F)Increased dopamine activity in the tuberoinfundibular pathway

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
11
A 40-year-old man with a history of hypertension comes to the office for a checkup. The patient has been under a lot of stress due to work issues and marital problems. He says, "My wife is always criticizing me, and we fight a lot. Last weekend, she was angry that I didn't make it to my daughter's basketball game. I wanted to go but was too tired because I had stayed out late with friends the night before. A man has to relax sometimes." The patient consumes 5 or 6 alcoholic drinks a night and more on weekends. He says that he never gets intoxicated as he is a "big guy with a high tolerance." Blood pressure is 170/90 mm Hg. Physical examination is normal. Laboratory evaluation indicates persistent mild elevation of liver function tests. The physician previously explained that the patient's hypertension is worsened by alcohol use and that the abnormal liver tests are likely due to alcohol use, but the patient remains unconcerned. Which of the following responses is most appropriate for initiating a discussion of the patient's alcohol use?
A)"Although you enjoy drinking, do you think it may have played a role in missing your daughter's game?"
B)"Continuing to drink these amounts of alcohol will likely result in liver damage."
C)"I am concerned that it will be difficult to control your blood pressure if you don't decrease your drinking."
D)"I am concerned that you are in denial about your alcohol use."
E)"I recommend trying to reduce your drinking with a long-term goal of complete abstinence."
F)"Is your wife upset that you are drinking too much?"
G)"Would you consider attending an Alcoholics Anonymous meeting?"
A)"Although you enjoy drinking, do you think it may have played a role in missing your daughter's game?"
B)"Continuing to drink these amounts of alcohol will likely result in liver damage."
C)"I am concerned that it will be difficult to control your blood pressure if you don't decrease your drinking."
D)"I am concerned that you are in denial about your alcohol use."
E)"I recommend trying to reduce your drinking with a long-term goal of complete abstinence."
F)"Is your wife upset that you are drinking too much?"
G)"Would you consider attending an Alcoholics Anonymous meeting?"

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
12
A 22-year-old man comes to the office due to fatigue, poor appetite, and weakness. The patient recently emigrated from India and has few social supports. He feels tired throughout the day despite sleeping 8-9 hours every night. He is worried about his new job and thinks that his coworkers don't like him. The patient reports no significant medical history but is very worried that he is losing semen when he urinates. Temperature is 36.7 C (98 F), blood pressure is 110/78 mm Hg, pulse is 62/min, and respirations are 14/min. BMI is 24 kg/m2. Physical examination is unremarkable. The patient is alert and oriented. His thought process is organized, linear, and coherent. He does not appear to be responding to internal stimuli. Which of the following would be the most appropriate initial response to the patient's concerns?
A)Do you ever hear voices when you're alone?
B)Do you think you might be depressed?
C)Have you lost your ability to enjoy your usual interests?
D)I can reassure you that you're not losing semen when you urinate.
E)What do you think is causing your illness?
F)Your physical examination is reassuring, but it may be helpful to meet with a counselor.
A)Do you ever hear voices when you're alone?
B)Do you think you might be depressed?
C)Have you lost your ability to enjoy your usual interests?
D)I can reassure you that you're not losing semen when you urinate.
E)What do you think is causing your illness?
F)Your physical examination is reassuring, but it may be helpful to meet with a counselor.

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
13
A 30-year-old man comes to the office due to chronic fatigue. When he is not working, the patient is often at home sleeping; he estimates that he sleeps approximately 12 hours a day. He has felt down since being passed over for a promotion last month and copes by overeating. The patient says he has never had a lot of energy and can remember only a few times since high school when he felt happy-a month he spent with his grandparents in Florida and a brief period when he felt really good after starting his first job. He has worked as a computer programmer since graduating from college. The patient socializes with friends but avoids dating due to his weight, saying, "I just know I will be rejected because I'm fat." Apart from obesity, the patient has no other medical conditions. He smokes marijuana 3 times a week, which he began doing in his mid-20s, to "help me relax and feel better about myself." He also drinks 4 cups of coffee before going to work on weekdays, which he says helps with his energy level. There is a family history of bipolar disorder in a maternal uncle. Vital signs and physical examination are unremarkable. Which of the following is the most likely diagnosis?
A)Adjustment disorder with depressed mood
B)Bipolar II disorder
C)Chronic fatigue syndrome
D)Cyclothymic disorder
E)Hypothyroidism
F)Persistent depressive disorder (dysthymia)
G)Substance-induced depressive disorder
A)Adjustment disorder with depressed mood
B)Bipolar II disorder
C)Chronic fatigue syndrome
D)Cyclothymic disorder
E)Hypothyroidism
F)Persistent depressive disorder (dysthymia)
G)Substance-induced depressive disorder

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
14
An 18-year-old woman comes to the office due to difficulty sleeping and fatigue. The patient started attending college 2 months ago and lives alone in an apartment near campus. For the past month, she has been increasingly anxious at night and thinks that someone is going to break into her home despite living on the eighth floor in a safe neighborhood. The patient makes sure to check that the front and balcony doors are secure every night and locks her bedroom door before going to bed. She wakes up multiple times a night when her air conditioner turns on or when she hears street noises and often has difficulty falling back asleep. The patient struggles to stay awake during class and is worried that her lack of sleep is beginning to affect her grades. She feels tense when walking alone on campus and spends time with friends only during the day. Vital signs are within normal limits. Physical examination shows no abnormalities. She appears anxious and reports that her mood has been okay. Which of the following is the most likely diagnosis?
A)Acute stress disorder
B)Adjustment disorder
C)Generalized anxiety disorder
D)Obsessive-compulsive disorder
E)Paranoid personality disorder
A)Acute stress disorder
B)Adjustment disorder
C)Generalized anxiety disorder
D)Obsessive-compulsive disorder
E)Paranoid personality disorder

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
15
An 80-year-old retired engineer is brought to the office by his son due to behavioral changes. The patient believes that his son is after his money and is trying to kick him out of the house to get all of his property. His son reports the patient has been more forgetful over the last few years. Medical history is nonsignificant. Vital signs are within normal limits. On physical examination, the patient is oriented to person and place only and is unable to cooperate with much of the cognitive examination. He has very poor short-term recall. He is unable to name the current American president and states, "I don't care to follow politics anymore." The remainder of the neurologic examination is unremarkable. Which of the following is the most likely diagnosis?
A)Alzheimer disease
B)Dementia with Lewy bodies
C)Frontotemporal dementia
D)Pseudodementia
E)Vascular dementia
A)Alzheimer disease
B)Dementia with Lewy bodies
C)Frontotemporal dementia
D)Pseudodementia
E)Vascular dementia

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
16
A 74-year-old man comes to the office for a scheduled follow-up after hospitalization for a myocardial infarction 4 weeks ago. The patient has had no new cardiac symptoms and has adhered to his outpatient medication regimen. When asked how he has been, he says, "I just don't feel like my old self." The patient's usual routine has been "disrupted" since he was discharged; he is not meeting with friends and has not been able to read the newspaper all the way through. He naps on his couch during the day and wakes up earlier than he wants to in the morning. The patient's medical history includes diet-controlled diabetes mellitus, hypertension, and obesity. Medications include aspirin, metoprolol, atorvastatin, lisinopril, and sublingual nitroglycerin as needed. Vital signs are within normal limits. Physical examination is unremarkable except for moderate obesity. He reports low mood and appears slowed and subdued. The patient declines psychotherapy. Which of the following is the most appropriate pharmacotherapy?
A)Citalopram
B)Desipramine
C)Mirtazapine
D)Phenelzine
E)Sertraline
F)Trazodone
G)Venlafaxine
A)Citalopram
B)Desipramine
C)Mirtazapine
D)Phenelzine
E)Sertraline
F)Trazodone
G)Venlafaxine

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
17
A 67-year-old man comes to the office with his wife due to increasing difficulty performing his job over the past year. He has become more irritable at work and has gotten into arguments with his boss for the first time in 20 years. His office has become increasingly cluttered as he refuses to throw things out, and he has forgotten to submit numerous recent assignments. His wife describes him as withdrawn, emotionally detached, and "not the man I married." She says, "Recently, he wants to eat the same meal every day and has lost interest in golf, which used to be one of his favorite pastimes." The patient has a history of hypertension and hyperlipidemia. He has a 30-pack-year smoking history. The patient scores 25/30 on the Montreal Cognitive Assessment (normal: ≥26). The remainder of the physical examination is normal. Which of the following is the most likely diagnosis in this patient?
A)Alzheimer disease
B)Dementia with Lewy bodies
C)Frontotemporal dementia
D)Hoarding disorder
E)Major depressive disorder
F)Vascular dementia
A)Alzheimer disease
B)Dementia with Lewy bodies
C)Frontotemporal dementia
D)Hoarding disorder
E)Major depressive disorder
F)Vascular dementia

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
18
A 76-year-old woman comes to the office for a routine checkup. Her medical history is significant for hypertension, type 2 diabetes mellitus, and hypothyroidism that are treated with oral agents. The patient had a stroke a year ago and has mild residual weakness in the right arm. Otherwise, she has no physical symptoms but is concerned about becoming more forgetful, especially because her mother died of Alzheimer disease. She says, "Sometimes I can't remember people's names, and occasionally during conversations, I can't seem to find the right word." The patient is widowed and lives alone. She drives herself to the grocery store weekly and manages her own finances. She describes her mood as "just okay," misses her husband, and regrets that she lives far from her children and grandchildren. The patient plays cards with her close friends regularly and is looking forward to a trip to visit her family. Her appetite is good, but she falls asleep earlier in the evening than before, awakening earlier in the morning and having less energy during the day. Blood pressure is 135/76 mm Hg and pulse is 65/min. Finger-stick glucose is 94 mg/dL and TSH is 2.4 µU/mL. She scores 26/30 on the Montreal Cognitive Assessment. Which of the following is the most likely diagnosis in this patient?
A)Alzheimer disease
B)Depression-related cognitive impairment
C)Hypothyroid-induced cognitive impairment
D)Mild cognitive impairment
E)Normal aging
F)Vascular dementia
A)Alzheimer disease
B)Depression-related cognitive impairment
C)Hypothyroid-induced cognitive impairment
D)Mild cognitive impairment
E)Normal aging
F)Vascular dementia

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
19
A 26-year-old man is brought to the emergency department by police after he was found disoriented and wandering on the street. No medical history is available. The patient is agitated and violent but calms down after several doses of lorazepam and haloperidol. Physical examination reveals confusion and bilateral horizontal nystagmus but no other focal neurologic findings. There are abrasions on the lower extremities. Urine drug screen is positive for phencyclidine. The patient is hospitalized for observation. Several hours later, his agitation and confusion have improved, but he reports difficulty with his vision. Temperature is 37.1 C (98.8 F), blood pressure is 134/84 mm Hg, pulse is 88/min, and respirations are 16/min. On examination, both eyes are deviated superiorly, and extraocular movement is restricted. There is rigidity of the neck and upper extremities. Noncontrast CT scan of the head shows no intracranial hemorrhage. Which of the following is most appropriate pharmacotherapy for this patient's current condition?
A)Acyclovir
B)Benztropine
C)Dantrolene
D)Fosphenytoin
E)Tetanus immunoglobulin
A)Acyclovir
B)Benztropine
C)Dantrolene
D)Fosphenytoin
E)Tetanus immunoglobulin

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
20
A 73-year-old man comes to the office due to increasing forgetfulness over the past 6 months. He says, "My mind used to be quite sharp, but now I can't even concentrate to read a book or newspaper. I'm afraid I'm developing dementia like my father." The patient reports he has been losing sleep and has little energy and motivation. He recently took a leave of absence from work because he could no longer concentrate on details and complete his paperwork. His medical history includes hypertension, hypercholesterolemia, diabetes, benign prostatic hyperplasia, and transient ischemic attack. Family history is significant for hypertension and diabetes (mother) and Alzheimer disease (father). The patient does not smoke and drinks wine only occasionally. Vital signs are unremarkable, and physical examination is normal except for slowed speech and movements. The patient declines to perform a serial sevens assessment and says, "I just can't do it." CT scan of the head is normal. Which of the following is the most likely cause of this patient's cognitive impairment?
A)Alzheimer disease
B)Dementia with Lewy bodies
C)Major depressive disorder
D)Normal aging
E)Parkinson disease
F)Vascular dementia
A)Alzheimer disease
B)Dementia with Lewy bodies
C)Major depressive disorder
D)Normal aging
E)Parkinson disease
F)Vascular dementia

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
21
A 76-year-old man is brought to the office by his wife for follow-up of recent behavioral changes. The patient has been much more withdrawn than usual over the past 6 months and often appears sad. He stopped driving a year earlier after getting lost several times in his own neighborhood. He now needs help with grocery shopping, meal preparation, and finances. His wife says, "He has good days and bad days. Sometimes he's almost like his old self; other times, he seems confused." She reports that while the patient sleeps, he frequently seems to act out his dreams and has kicked her on occasion. Medical history includes hypertension and hypercholesterolemia. Temperature is 37.3 C (99.1 F), blood pressure is 137/78 mm Hg, pulse is 78/min, and respirations are 14/min. On neurologic examination, there is bilateral resistance to passive movement of the upper extremities, and the patient walks with an unsteady gait. Montreal cognitive assessment score is 21/30 (normal: ≥26). The remainder of the examination shows no abnormalities. Which of the following is the most likely diagnosis in this patient?
A)Alzheimer disease
B)Creutzfeldt-Jakob disease
C)Dementia with Lewy bodies
D)Depression-related cognitive impairment (pseudodementia)
E)Frontotemporal dementia
F)Normal-pressure hydrocephalus
G)Vascular dementia
A)Alzheimer disease
B)Creutzfeldt-Jakob disease
C)Dementia with Lewy bodies
D)Depression-related cognitive impairment (pseudodementia)
E)Frontotemporal dementia
F)Normal-pressure hydrocephalus
G)Vascular dementia

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
22
An 80-year-old woman is brought to the office by her husband due to behavioral disturbances. The patient has a history of Alzheimer disease. For the past month, she has been wandering the house at night, looking for a pet cat that died 10 years ago. The patient has also been excessively agitated and hits her husband when he tries to assist her. She has had no other symptoms. Environmental and behavioral interventions have been unsuccessful. Medical history also includes hypertension. Medications include amlodipine and donepezil. There have been no recent changes in medications. Vital signs are within normal limits, and physical examination shows no new abnormalities. Blood cell counts, serum electrolytes, and urinalysis are normal. Caregiver education is provided, and nightly risperidone is started after discussing medication options. A week later, the husband reports that the patient is less aggressive, but her restlessness and wandering have worsened. Now, she cannot sit still, even for a few minutes. Which of the following is the most appropriate next step in management of this patient?
A)Add memantine therapy
B)Advise nursing home placement
C)Discontinue risperidone
D)Increase the dose of risperidone
E)Switch risperidone to lorazepam
A)Add memantine therapy
B)Advise nursing home placement
C)Discontinue risperidone
D)Increase the dose of risperidone
E)Switch risperidone to lorazepam

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
23
A 71-year-old man comes to the office due to "strange visions." He lives alone and has not seen a doctor in 30 years. The patient says, "I started seeing children playing in my yard in the evenings about 2 months ago. What's weird is that my closest neighbors are 2 miles away, and I rarely have anyone visit." He says that this was not too disturbing; however, about a month ago, he started seeing animals scampering throughout his house despite not owning any pets, which caused more alarm. The patient is not forgetful and still drives, goes grocery shopping, prepares meals, and takes care of chores around the house. He says his energy is "not what it used to be," and he has lost his balance a few times but has not fallen. The patient also states that he does not like to socialize but adds that he has "always been like that." He is unaware of any medical diagnoses. Temperature is 37.1 C (98.8 F), blood pressure is 138/89 mm Hg, pulse is 78/min, and respirations are 14/min. The patient scores 29 of 30 (normal: ≥26) on the Montreal Cognitive Assessment. Gait is steady but slow. He has a tremor at rest that is most prominent in the right hand. Reflexes are 3+ on the right and 2+ on the left, and there is resistance to passive movement in all limbs that is worse on the right. Which of the following is the most likely diagnosis in this patient?
A)Brief psychotic disorder
B)Delirium
C)Dementia with Lewy bodies
D)Major depressive disorder with psychotic features
E)Parkinson disease
F)Schizotypal personality disorder
A)Brief psychotic disorder
B)Delirium
C)Dementia with Lewy bodies
D)Major depressive disorder with psychotic features
E)Parkinson disease
F)Schizotypal personality disorder

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
24
A 23-year-old primigravida at 32 weeks gestation is brought to the emergency department by her mother due to a seizure that occurred 30 minutes ago. The mother states her daughter was eating lunch at a restaurant and "suddenly started shaking her arms and legs." During the 45-second episode, the patient's head moved from side to side and her eyes fluttered. The patient has no chronic medical conditions, and her pregnancy has been uncomplicated. Temperature is 37.4 C (99.3 F), blood pressure is 128/84 mm Hg, and pulse is 82/min. The patient is alert and fully oriented. Cardiopulmonary examination is normal. Neurologic examination demonstrates no abnormalities. When the abdomen is palpated, the patient states she is not feeling well and suddenly starts to have rhythmic, asynchronous movements of the upper and lower extremities. The jaw is clenched, and the patient does not respond to questions or follow commands. The episode resolves within 1 minute and the patient is alert and oriented. Repeat blood pressure is 116/74 mm Hg. Fetal heart rate tracing has a baseline of 150/min, moderate variability, and no decelerations. Complete blood count, basic metabolic panel, and urinalysis show no abnormalities. Urine drug screen is negative. Which of the following is the best next step in management of this patient?
A)24-hour urine protein collection
B)Carbamazepine
C)Emergency cesarean delivery
D)Immediate induction of labor
E)Magnesium sulfate
F)Video electroencephalogram
A)24-hour urine protein collection
B)Carbamazepine
C)Emergency cesarean delivery
D)Immediate induction of labor
E)Magnesium sulfate
F)Video electroencephalogram

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
25
An 85-year-old man comes to the office accompanied by his daughter due to "memory problems." The patient is a retired accountant who lives alone and had been managing his finances and housework until a month ago. He says, "I've had to ask my daughter to shop for me and help around the house. I kept forgetting to turn off the stove and could have easily burned down the house." The patient has been more tired than usual and sleeps through his favorite television shows. He previously maintained a rose garden but now feels "it's not worth the effort." The patient's daughter says, "He was due for a medication refill last week but still has a few pills left because he sometimes forgets to take them." Medical history includes hypothyroidism, hypertension, hypercholesterolemia, and a transient ischemic attack 2 years ago. Temperature is 37.2 C (99 F), blood pressure is 141/87 mm Hg, pulse is 76/min, and respirations are 14/min. His weight is up 4 kg (8.8 lb) from last month. TSH is 4.0 µU/mL. He scores 21/30 on the Montreal Cognitive Assessment (normal: ≥26), with deficits in delayed recall and attention. Which of the following is the most likely cause of this patient's cognitive impairment?
A)Alzheimer disease
B)Dementia with Lewy bodies
C)Dissociative amnesia
D)Frontotemporal dementia
E)Major depressive disorder
F)Subclinical hypothyroidism
G)Vascular dementia
A)Alzheimer disease
B)Dementia with Lewy bodies
C)Dissociative amnesia
D)Frontotemporal dementia
E)Major depressive disorder
F)Subclinical hypothyroidism
G)Vascular dementia

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
26
A 49-year-old woman comes to the office due to depression. She quit her retail sales job 6 months ago as she could no longer stand all day due to increasing numbness, tingling, and painful, burning sensations in her feet. The patient has since become increasingly depressed, withdrawn, and preoccupied with feelings of low self-esteem. She is unable to concentrate to read or watch television and has lost interest in her family and friends. The patient also describes severe insomnia and extremely low energy. Medical history is significant for obesity, hypercholesterolemia, and type 2 diabetes mellitus. Medications include glipizide and lisinopril. She has no prior psychiatric history. After medical evaluation, major depressive disorder is diagnosed. Which of the following is the most appropriate pharmacotherapy to treat this patient's condition?
A)Bupropion
B)Citalopram
C)Duloxetine
D)Mirtazapine
E)Trazodone
A)Bupropion
B)Citalopram
C)Duloxetine
D)Mirtazapine
E)Trazodone

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
27
A 68-year-old man comes to the office due to balance problems over the last 2 weeks. He has had muscle stiffness and 3 near-falls recently. The patient has no musculoskeletal pain or visual problems. He has a history of bipolar disorder and anxiety and was started on valproate and risperidone for a manic episode 5 months ago. Other medical issues include hypertension that is controlled with hydrochlorothiazide. Temperature is 37.2 C (99 F) and blood pressure is 122/78 mm Hg supine and 130/80 mm Hg standing. The patient appears slightly anxious but no longer manic. There is an asymmetric resting tremor in both hands. Finger tapping is slow and irregular bilaterally. Which of the following is the most likely cause of this patient's current condition?
A)Acute dystonia
B)Akathisia
C)Cerebellar stroke
D)Charcot-Marie-Tooth disease
E)Drug-induced parkinsonism
F)Essential tremor
G)Neuroleptic malignant syndrome
H)Tardive dyskinesia
A)Acute dystonia
B)Akathisia
C)Cerebellar stroke
D)Charcot-Marie-Tooth disease
E)Drug-induced parkinsonism
F)Essential tremor
G)Neuroleptic malignant syndrome
H)Tardive dyskinesia

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
28
A 76-year-old man is brought to the office by his daughter due to increasing confusion and falls. The patient was diagnosed with dementia with Lewy bodies 2 weeks ago and started on carbidopa-levodopa, risperidone, and rivastigmine for symptomatic management. Temperature is 37.2 C (99 F) and respirations are 14/min. Supine blood pressure and pulse are 129/82 mm Hg and 75/min, respectively; standing blood pressure and pulse are 101/74 mm Hg and 97/min, respectively. The patient is not oriented to place or time. Cranial nerves are intact and upper and lower limb deep tendon reflexes are 2+. Rigidity is present in both the upper and the lower extremities on passive movement and is notably worse compared with the previous examination. Which of the following is the most likely explanation for this patient's symptoms?
A)Carbidopa-levodopa
B)Postural tachycardia syndrome
C)Progression of disease
D)Risperidone
E)Rivastigmine
A)Carbidopa-levodopa
B)Postural tachycardia syndrome
C)Progression of disease
D)Risperidone
E)Rivastigmine

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
29
A 24-year-old woman is brought to the office by her roommate due to behavioral changes. After taking a few days off work to recover from flu-like symptoms a month ago, the patient started to feel anxious about getting fired. Despite repeated reassurance from her boss, she continued to fixate on losing her job and had difficulty sleeping. More recently, she became convinced that her employer was trying to harm her and stopped going to work. The patient has been increasingly forgetful over the past week and was briefly unable to recognize well-known friends that came to visit her. Earlier today, her roommate noticed the patient staring blankly and smacking her lips rhythmically for about a minute while they watched television. An incidental, 2-cm, right-sided ovarian teratoma was visualized on ultrasound 2 months ago; the patient is scheduled for surgical resection next month. She has no other medical or psychiatric history. Temperature is 38 C (100.4 F), blood pressure is 167/86 mm Hg, pulse is 122/min, and respirations are 14/min. The patient is fully oriented, although easily distracted. The left hand is clenched, and the left wrist is held in sustained flexion. Mild rigidity is noted in the upper extremities. Deep tendon reflexes are 3+ throughout, and her gait is normal. She appears to be responding to internal stimuli and mumbles to herself during the examination. Which of the following is the most likely diagnosis?
A)Aseptic meningitis
B)Autoimmune encephalitis
C)Brief psychotic disorder
D)Huntington disease
E)Schizophreniform disorder
A)Aseptic meningitis
B)Autoimmune encephalitis
C)Brief psychotic disorder
D)Huntington disease
E)Schizophreniform disorder

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
30
A 68-year-old woman with a 3-year history of idiopathic Parkinson disease comes to the office with her husband for follow-up. The patient reports adequate control of motor symptoms with levodopa-carbidopa therapy but states that for the past month, she no longer spends time with her friends or participates in her church choir due to difficulty focusing. She sleeps restlessly most nights, resulting in daytime naps, and skips dinner because she is not hungry. Medical history is otherwise noncontributory, and the patient takes no other medications. Vital signs are within normal limits. Physical examination shows reduced facial expressions and mild slowing on repeated finger tapping but no significant tremors. Posture and gait are normal. Which of the following is the best next step in management?
A)Add a dopamine agonist
B)Prescribe an antidepressant
C)Prescribe an atypical antipsychotic
D)Prescribe a stimulant
E)Reduce the levodopa-carbidopa dose
A)Add a dopamine agonist
B)Prescribe an antidepressant
C)Prescribe an atypical antipsychotic
D)Prescribe a stimulant
E)Reduce the levodopa-carbidopa dose

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
31
A 39-year-old woman comes to the emergency department with sudden right leg weakness. The patient's medical history is significant for gastroesophageal reflux disease, which provokes occasional heartburn after meals despite medication therapy. She does not use tobacco, alcohol, or illicit drugs. The patient's husband of 20 years recently died suddenly in a car accident. Blood pressure is 120/70 mm Hg, pulse is 82/min, and respirations are 12/min. She has mild epigastric discomfort on palpation, but the rest of the abdominal examination is within normal limits. Neurological examination shows normal muscle tone, normal deep-tendon reflexes, and no Babinski sign in the extremities. The patient cannot lift her right leg off the bed while supine and is very worried that something is wrong. She is able to stand without assistance from a sitting position and her gait is without abnormalities. Which of the following is the most likely diagnosis?
A)Conversion disorder
B)Factitious disorder
C)Illness anxiety disorder
D)Malingering
E)Multiple sclerosis
F)Somatic symptom disorder
A)Conversion disorder
B)Factitious disorder
C)Illness anxiety disorder
D)Malingering
E)Multiple sclerosis
F)Somatic symptom disorder

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
32
A 55-year-old man is brought to the office due to unusual movements of his face and extremities. He lives in a group home and was noted to be sticking out his tongue, smacking his lips, and twisting his body from side to side, actions that were disruptive to the other residents. The patient has a history of schizoaffective disorder that has been treated with risperidone, fluoxetine, and clonazepam for more than 20 years. Examination shows protruding and twisting movements of the tongue, dystonic postures of the neck, and squirming movements of the torso. Which of the following is the most likely underlying cause of this patient's symptoms?
A)Caudate nucleus atrophy
B)Dopamine receptor downregulation
C)Dopamine receptor supersensitivity
D)GABA receptor upregulation
E)Glutamate receptor supersensitivity
F)Serotonin receptor downregulation
G)Ventral tegmental area atrophy
A)Caudate nucleus atrophy
B)Dopamine receptor downregulation
C)Dopamine receptor supersensitivity
D)GABA receptor upregulation
E)Glutamate receptor supersensitivity
F)Serotonin receptor downregulation
G)Ventral tegmental area atrophy

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
33
A 19-year-old woman is brought to the emergency department by her father due to bizarre behavior. When the patient did not come down for breakfast this morning, her father went to her room and found her sitting up in bed, staring at the wall. The patient did not respond to questions and was very stiff when her father tried to help her stand. The patient was diagnosed with bipolar disorder last year. She takes lithium, risperidone, and fluoxetine. Her dosages of risperidone and fluoxetine were both increased recently to target residual depressive symptoms. Temperature is 36.6 C (97.9 F), blood pressure is 121/78 mm Hg, pulse is 68/min, and respirations are 14/min. When asked what today's date is, the patient repeats, "Date, date, date," repeatedly. She resists the examiner's movement of her arms, increasing her resistance in proportion to the applied force. Which of the following is the most likely diagnosis for this patient?
A)Akinetic mutism
B)Catatonia
C)Delirium
D)Drug-induced parkinsonism
E)Locked-in syndrome
F)Neuroleptic malignant syndrome
G)Serotonin syndrome
A)Akinetic mutism
B)Catatonia
C)Delirium
D)Drug-induced parkinsonism
E)Locked-in syndrome
F)Neuroleptic malignant syndrome
G)Serotonin syndrome

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
34
A 62-year-old man is brought to the office by his wife due to recent personality changes and cognitive impairment. The symptoms began 4 months ago with abrupt-onset depression and profound sleepiness. Soon after, the patient began having difficulty remembering names and events. He now cannot prepare his own meals or care for himself. The patient has a history of herpes simplex virus type 1 and takes acyclovir occasionally for recurrent symptoms; medical history is otherwise unremarkable. He has no history of psychiatric disease but has a family history of dementia from his father. The patient has a 40-pack-year smoking history. Temperature is 37.7 C (99.9 F), blood pressure is 118/79 mm Hg, pulse is 72/min, and respirations are 14/min. The patient is oriented only to self. Montreal Cognitive Assessment score is 10/30 (normal: ≥26). Near the end of the examination, the patient startles and jerks his arms when a door closes loudly. Lumbar puncture is recommended. Which of the following findings would be expected in this patient's cerebrospinal fluid?
A)High 14-3-3 protein titers
B)High anti-Hu antibody titers
C)High anti-NMDA receptor antibody titers
D)High herpes simplex viral DNA titers
E)Low alpha-synuclein titers
F)Low hypocretin titers
A)High 14-3-3 protein titers
B)High anti-Hu antibody titers
C)High anti-NMDA receptor antibody titers
D)High herpes simplex viral DNA titers
E)Low alpha-synuclein titers
F)Low hypocretin titers

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
35
A 68-year-old man is brought to the primary care physician's office by his wife. She reports that the patient has been flailing in his sleep, particularly during the early morning hours. She is worried that he will hurt himself or her with these movements. The episodes started several months ago with infrequent nighttime movements but now occur almost nightly. The patient's wife says, "It's like he can't control himself. I have seen him kicking in bed, pushing over the nightstand, and moving furniture out of the way. He has also tried to push me from behind with his whole body, all while appearing to be asleep." She is able to wake him from these episodes, and he doesn't appear disoriented or confused on awakening. The patient is unaware of his nighttime movements but describes a recurrent dream in which he feels lost and trapped in the woods and tries to escape. He has had no behavioral symptoms while awake during the day. His only other symptom is constipation. The patient's medical history includes well-controlled hypertension. Vital signs are within normal limits, and physical examination is normal except for slight slowness of gait. Which of the following is the most likely diagnosis?
A)Nightmare disorder
B)Nocturnal seizures
C)Obstructive sleep apnea
D)Rapid eye movement sleep behavior disorder
E)Restless legs syndrome
F)Sleep terrors
G)Sleepwalking
A)Nightmare disorder
B)Nocturnal seizures
C)Obstructive sleep apnea
D)Rapid eye movement sleep behavior disorder
E)Restless legs syndrome
F)Sleep terrors
G)Sleepwalking

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
36
A 21-year-old woman is brought to the emergency department by her roommate due to anxiety. The patient has generalized anxiety disorder and takes sertraline but has been increasingly restless for the past 2 days, pacing in her room and startling easily. She has been studying for a graduate school entrance examination for the past month, staying up late and drinking 2 cups of coffee a day. The patient has been taking her roommate's tramadol for headaches that have become more frequent. She has no other medical or psychiatric history. Temperature is 37.7 C (99.9 F), blood pressure is 140/80 mm Hg, pulse is 100/min, and respirations are 14/min. The patient appears jittery and has perspiration on her forehead. No abnormalities are noted on cardiopulmonary examination. Muscle tone is mildly increased in the upper and lower extremities. Deep tendon reflexes are symmetric and 3+ throughout. The patient says she feels overwhelmed and unprepared for her exam. Which of the following is the most likely diagnosis?
A)Caffeine intoxication
B)Hyperthyroidism
C)Panic attack
D)Serotonin syndrome
E)Stimulant intoxication
A)Caffeine intoxication
B)Hyperthyroidism
C)Panic attack
D)Serotonin syndrome
E)Stimulant intoxication

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
37
A 22-year-old man comes to the office due to irregular sleep for the past 3 months. The patient says, "School has become more stressful, and I have been feeling more fatigued since my girlfriend broke off our relationship last month." He is often sleepy during the day and sometimes falls asleep unintentionally during classes. The patient goes to bed at 1 AM and awakens at 9 AM. After classes, he avoids socializing and frequently returns straight to his dorm room to nap. The patient also describes "weird things happening as I fall asleep, like hearing whispering voices and seeing colorful animals." He describes another unusual experience last week when he suddenly felt weak in his face and knees following an upsetting phone call with his ex-girlfriend. The patient drinks beer socially but does not use illicit drugs. He has a history of depression as a teenager that responded to psychotherapy. Height is 170.2 cm (5 ft 7 in), and weight is 83.9 kg (185 lb). BMI is 29 kg/m2. Physical examination is normal. Which of the following is the most likely diagnosis for this patient?
A)Adjustment disorder
B)Delayed sleep-wake phase disorder
C)Hypersomnolence disorder
D)Insufficient sleep
E)Major depression with psychotic features
F)Narcolepsy
A)Adjustment disorder
B)Delayed sleep-wake phase disorder
C)Hypersomnolence disorder
D)Insufficient sleep
E)Major depression with psychotic features
F)Narcolepsy

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
38
A 68-year-old man is brought to the emergency department by his wife due to "uncharacteristic behavior." The patient started buying large numbers of lottery tickets and decided to quit his job 2 weeks ago. He has maxed out multiple credit cards buying expensive jewelry for his wife. The patient has had difficulty sleeping recently and stays up watching TV into the early morning hours. He says, "I feel really good and finally like what I'm doing." The patient has no psychiatric history. Medical history includes recently diagnosed restless leg syndrome, treated with ropinirole. Temperature is 37.1 C (98.8 F), blood pressure is 130/80 mm Hg, and pulse is 86/min. Physical examination is within normal limits. The patient is restless, appears to be easily distracted, and speaks rapidly. Complete blood count and basic metabolic panel are within normal limits. Urine drug screen is negative. Which of the following is the most appropriate initial step in management?
A)Obtain vitamin B12 level
B)Order MRI of the head
C)Start lithium
D)Start lorazepam
E)Stop ropinirole
A)Obtain vitamin B12 level
B)Order MRI of the head
C)Start lithium
D)Start lorazepam
E)Stop ropinirole

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
39
A 46-year-old man is hospitalized due to suicidal ideation and hearing voices. The patient has become increasingly depressed over the past month and has been unable to work. Last week he told his wife that he was "tormented by voices" and that "death would be a relief." She brought him to the hospital after she found him staring at a blank screen on the television and not responding to her questions. The patient was prescribed risperidone, lithium, and escitalopram by his psychiatrist, but his wife is unsure if he takes them regularly. He has a history of bipolar disorder since age 18 with multiple hospitalizations for both manic and depressive episodes. His other medical problems are hypercholesterolemia and seasonal allergies. Temperature is 37 C (98.6 F), blood pressure is 125/80 mm Hg, pulse is 68/min, and respirations are 12/min. Routine laboratory results are within normal limits, lithium level is within therapeutic range, and a toxicology screen is negative. During the evaluation, the patient stares blankly and is mute and motionless. He resists all instructions to move. When the physician lifts the patient's arm, it remains in the exact same position after she lets go. Which of the following is the most appropriate next step in management?
A)Benztropine
B)Clozapine
C)Cyproheptadine
D)Dantrolene
E)Increase risperidone
F)Lorazepam
A)Benztropine
B)Clozapine
C)Cyproheptadine
D)Dantrolene
E)Increase risperidone
F)Lorazepam

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
40
A 40-year-old man comes to the office due to hand tremors for the past 2 months. The patient is an art teacher and has had difficulty demonstrating techniques in front of the class due to shaky hands. When noticing others looking at his hands, he becomes increasingly anxious and self-conscious, which tends to worsen the tremor. The patient has a history of bipolar disorder with a manic episode 6 months ago. He currently reports stable mood on the prescribed medication. The patient drinks alcohol occasionally and has not noticed any tremor changes with alcohol use. There is no family history of neurologic disorders. Vital signs are within normal limits. Physical examination shows fine, bilateral hand tremors that worsen with posture held against gravity. Muscle tone, strength, and deep tendon reflexes are normal throughout. Gait is normal. On mental status examination, he is cooperative and appears mildly anxious. The remainder of the physical examination shows no abnormalities. Which of the following is the most likely cause of this patient's current symptoms?
A)Dystonic tremor
B)Essential tremor
C)Hyperthyroidism
D)Idiopathic Parkinson disease
E)Medication adverse effect
A)Dystonic tremor
B)Essential tremor
C)Hyperthyroidism
D)Idiopathic Parkinson disease
E)Medication adverse effect

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
41
A 37-year-old man is brought to the emergency department by police officers. He was found naked at a traffic signal, cursing at drivers and assaulting nearby pedestrians. The patient has a long history of abusing multiple substances and has been admitted to the hospital several times with a similar presentation. He has epilepsy and type 2 diabetes mellitus. Attempts to elicit a history from the patient prove unsuccessful because he is highly agitated and combative. He keeps repeating, "They are all out to get me. They are coming through the walls, ready to kill me." The patient alternates between screaming and pounding on the walls. Temperature is 38.3 C (100.9 F), blood pressure is 148/100 mm Hg, pulse is 98/min, and respirations are 16/min. Physical examination shows ataxia, nystagmus, and muscle rigidity. Which of the following is the most appropriate next step in management of this patient?
A)Dexmedetomidine
B)Dimercaprol
C)Fomepizole
D)Lorazepam
E)Phentolamine
F)Risperidone
G)Urinary acidification
A)Dexmedetomidine
B)Dimercaprol
C)Fomepizole
D)Lorazepam
E)Phentolamine
F)Risperidone
G)Urinary acidification

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
42
A 23-year-old man comes to the emergency department declaring that police helicopters have followed him for the past year. The patient is convinced that their surveillance lasers are damaging his sperm. He says that the lasers have caused burns on his stomach and a low sperm count. As evidence, the patient points to an area of slight discoloration that looks like a birthmark on his lower abdomen. He has contacted an officer in charge of internal affairs who is investigating his charge of police brutality. The patient has a history of 2 prior psychiatric hospitalizations. His psychosis rapidly improves during hospitalization, but following discharge he stops taking his medication. The patient says, "I used to have schizophrenia, but now I'm cured." He is highly anxious and frequently gets up to pace and look out the window. After describing his fears, he asks if the physician believes him. Which of the following is the best response to the patient?
A)I believe that these experiences have been very frightening for you.
B)I can assure you that in the hospital you are safe from any further attacks.
C)I can see that you are frightened but can assure you that the police are not following you.
D)I understand that you are frightened, but your concerns are more likely symptoms of your illness.
E)Let me assure you that we are here to help you and that the discoloration is only a birthmark.
F)Schizophrenia is a chronic illness; you have previously experienced similar fears that respond well to medication.
A)I believe that these experiences have been very frightening for you.
B)I can assure you that in the hospital you are safe from any further attacks.
C)I can see that you are frightened but can assure you that the police are not following you.
D)I understand that you are frightened, but your concerns are more likely symptoms of your illness.
E)Let me assure you that we are here to help you and that the discoloration is only a birthmark.
F)Schizophrenia is a chronic illness; you have previously experienced similar fears that respond well to medication.

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
43
A 16-year-old girl is brought to the emergency department by her parents for evaluation of bizarre behavior. The patient was found in her bedroom surrounded by broken lamps and ripped-up notebooks. Her father says, "She's been a bit irritable for the past few days, probably because she's been studying for final exams nonstop. We heard some noises in the middle of the night and found her wide awake and unable to sit still." The patient has no medical conditions and no psychiatric history; she takes diphenhydramine as needed when she cannot sleep. Family history is significant for bipolar disorder in the patient's older sister. Temperature is 37.6 C (99.7 F), blood pressure is 150/90 mm Hg, pulse is 120/min, and respirations are 18/min. On physical examination, the patient appears diaphoretic and restless. During the cardiovascular examination, the patient removes the physician's stethoscope and says, "I need to get home and finish my paper. It's due in a few hours." Which of the following is the most appropriate pharmacotherapy for this patient?
A)Clonidine
B)Lithium
C)Lorazepam
D)Physostigmine
E)Propranolol
F)Risperidone
A)Clonidine
B)Lithium
C)Lorazepam
D)Physostigmine
E)Propranolol
F)Risperidone

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
44
A 26-year-old man is brought to the emergency department due to hallucinations. The patient's mother reports that he was acting normally until a few hours ago when he started hallucinating that dogs were chasing him. She states that the patient has a history of schizoaffective disorder that was difficult to treat and is currently taking clozapine and doxepin; however, she is worried about his mental health because he broke up with his partner yesterday. Temperature is 38.3 C (100.9 F), blood pressure is 140/80 mm Hg, pulse is 145/min, and respirations are 24/min. Oxygen saturation is 97% on room air. The patient is delirious and actively hallucinating. His pupils are 6 mm and nonreactive. No murmurs or gallops are present on auscultation of the heart. Muscle tone and reflexes are normal. What is the best next step in management?
A)Administer a dopamine agonist
B)Administer intramuscular haloperidol
C)Electrocardiogram
D)Electroencephalogram
A)Administer a dopamine agonist
B)Administer intramuscular haloperidol
C)Electrocardiogram
D)Electroencephalogram

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
45
An 18-year-old woman is brought to the emergency department after a suspected drug overdose at 6 AM. The mother states that she had awakened this morning to find her daughter difficult to rouse and covered in emesis. The prescription bottle of paroxetine 20 mg containing 30 pills filled the previous day was next to her and was empty. She does not know when or if her daughter took the medication. She last saw her daughter the previous evening before going to bed at 10 PM. Her daughter has a history of major depressive disorder but has no known previous suicide attempts. Temperature is 36.1 C (97 F), blood pressure is 110/70 mm Hg, pulse is 70/min, and respirations are 10/min. Pulse oximetry is 98% on room air. On examination, the patient's clothes are stained with emesis. Her eyes are closed, and she does not follow commands but moans and withdraws all the extremities to painful stimuli. The pupils are normal sized, equal, and reactive. Muscle tone and reflexes are normal. Cardiopulmonary and abdominal examinations are normal. There is no evidence of trauma. Which of the following is the best next step in management?
A)Administer activated charcoal
B)Administer cyproheptadine
C)Administer sodium bicarbonate
D)Evaluate for coingestants
E)Obtain serum levels of paroxetine
A)Administer activated charcoal
B)Administer cyproheptadine
C)Administer sodium bicarbonate
D)Evaluate for coingestants
E)Obtain serum levels of paroxetine

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
46
A 16-year-old boy is brought to the emergency department by his friends for severe anxiety. He became paranoid and unusually withdrawn at a party and began rocking back and forth, saying, "I feel like I can't breathe" and "I'm afraid I'm going to die." Prior to the party, he was his regular "happy and outgoing" self. The patient has intermittent back pain from a bicycle accident last year for which he takes oxycodone as needed. Temperature is 36.1 C (97 F), blood pressure is 140/80 mm Hg, pulse is 110/min, and respirations are 18/min. Pulse oximetry is 98% on room air. Examination shows an anxious and withdrawn boy with 3-mm pupils, conjunctival injection, dry oral mucosa, and a healed scar on his right thigh from his bicycle accident. Which of the following is most consistent with this patient's presentation?
A)Bath salts intoxication
B)Cannabis intoxication
C)Cocaine intoxication
D)Cocaine withdrawal
E)Lysergic acid diethylamide intoxication
F)Opioid intoxication
G)Opioid withdrawal
H)Phencyclidine intoxication
A)Bath salts intoxication
B)Cannabis intoxication
C)Cocaine intoxication
D)Cocaine withdrawal
E)Lysergic acid diethylamide intoxication
F)Opioid intoxication
G)Opioid withdrawal
H)Phencyclidine intoxication

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
47
A 43-year-old man is brought to the emergency department by the police after being found walking in the middle of a busy parking lot while talking to himself and shouting at passing cars. The patient is barefoot and disheveled. He is oriented to person and place but is unable to give a coherent history. He says, "I've been in a lot of hospitals, but I won't take any medication." The patient appears tense and agitated. When the nurse attempts to take vital signs, he refuses and pulls his arm away. He glares at the nurse and shouts, "All you do is experiment on people." Which of the following is the most appropriate next step in management of this patient?
A)Administer intramuscular antipsychotic medication
B)Calmly explain that he will be restrained to ensure his safety and that of the staff
C)Inform the patient that security will be called if he cannot calm down
D)Offer the patient something to eat and drink
A)Administer intramuscular antipsychotic medication
B)Calmly explain that he will be restrained to ensure his safety and that of the staff
C)Inform the patient that security will be called if he cannot calm down
D)Offer the patient something to eat and drink

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
48
A 37-year-old man with a history of depression, alcohol, and polysubstance use comes to the emergency department saying, "I feel awful; I need help." The patient says he was feeling fine until last night, when he developed abdominal cramps that were initially mild but gradually worsened in intensity. Since this morning, he has had 4 loose stools with no blood or mucus. The patient has also had persistent nausea but no vomiting. He has had no fever. His medications include paroxetine, clonazepam, and diphenhydramine. Temperature is 36.6 C (97.8 F), blood pressure is 144/98 mm Hg, pulse is 88/min, and respirations are 16/min. Physical examination shows a diaphoretic, thin man in considerable distress. His pupils are dilated. This patient's clinical presentation is most consistent with withdrawal from which of the following drugs?
A)Alcohol
B)Amphetamine
C)Clonazepam
D)Cocaine
E)Diphenhydramine
F)Heroin
G)Paroxetine
A)Alcohol
B)Amphetamine
C)Clonazepam
D)Cocaine
E)Diphenhydramine
F)Heroin
G)Paroxetine

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
49
A 35-year-old man comes to the office due to sexual symptoms. The patient has normal libido and erectile function but has uncontrollable orgasm within a minute of vaginal penetration during intercourse. His symptoms started 6 months ago after his wife gave birth to their second child. The patient says his symptoms are distressing and are leading to considerable frustration in his relationship with his wife. Medical history and examination are unremarkable. Which of the following is the most appropriate next step in management of this patient's sexual symptoms?
A)Low-dose finasteride
B)Paroxetine therapy
C)Serum prolactin level
D)Serum testosterone level
E)Sildenafil as needed
A)Low-dose finasteride
B)Paroxetine therapy
C)Serum prolactin level
D)Serum testosterone level
E)Sildenafil as needed

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
50
A 63-year-old man is brought to the emergency department due to restlessness and altered mental status. His wife reports that the patient awakened at 6:00 AM agitated and slightly confused. Over the past 2 hours, his symptoms have worsened. She states that he was well the previous day but went to his primary care doctor due to a persistent, dry cough for 3 weeks following an upper respiratory tract infection. The patient was prescribed dextromethorphan and an albuterol inhaler. He has a history of major depressive disorder that is well controlled with fluoxetine. Temperature is 38.3 C (101 F), blood pressure is 160/90 mm Hg, pulse is 112/min, and respirations are 22/min. Pulse oximetry is 100% on room air. The patient is agitated and confused. Pupils are dilated, and lungs are clear to auscultation bilaterally. Hyperreflexia and ankle clonus are noted on neurological examination. Which of the following is the most appropriate initial therapy for this patient?
A)Bromocriptine
B)Haloperidol
C)Levofloxacin
D)Lorazepam
E)Physostigmine
A)Bromocriptine
B)Haloperidol
C)Levofloxacin
D)Lorazepam
E)Physostigmine

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
51
A 25-year-old woman comes to the office due to a 3-week history of depressed mood, low energy, loss of motivation, and oversleeping following the break-up of a relationship. The patient is sleeping 12 hours each day and describes difficulty getting out of bed and showering and dressing in the morning. Her concentration is poor at work, and she has difficulty completing everyday tasks. The patient has no psychotic symptoms or suicidal ideation. She has a history of major depressive episodes at age 16 and 20. The patient was treated briefly with fluoxetine at age 20 but stopped the medication after a week as she did not like the way it made her feel. Following a rape at age 22, she was treated with trauma-focused psychotherapy for 6 months. The patient has no significant medical history. She drinks a beer several times a week and uses cannabis approximately once every other month. Physical examination is normal. After the physician discusses treatment options for depression, the patient chooses to have combination treatment with psychotherapy and medication. Which of the following would be most important to obtain prior to initiating pharmacologic treatment for this patient?
A)Complete blood count and comprehensive metabolic panel
B)Detailed trauma history
C)History of anxiety symptoms
D)History of elevated mood
E)Thyroid function tests
F)Urine toxicology screen
A)Complete blood count and comprehensive metabolic panel
B)Detailed trauma history
C)History of anxiety symptoms
D)History of elevated mood
E)Thyroid function tests
F)Urine toxicology screen

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
52
A 19-year-old woman is brought to the emergency department by the police after she was found trespassing at an animal shelter. The patient had keys to a rental van, as well as numerous collars and leashes. She says, "The shelter is going to sell the animals to labs, where they'll do horrible experiments on them. I'm the only one who can save them!" The patient quit her retail job a week ago to spend more time researching escape routes for the animals. Throughout the evaluation, she interrupts the physician to yell at other patients and hospital staff walking by the room. She repeatedly refers to herself as a "cat burglar" and then laughs loudly for a few minutes. Physical examination is unremarkable and urine drug screening is negative. Which of the following additional features is most likely in this patient?
A)Experiencing a sensation of bugs crawling on skin
B)Experiencing intrusive, unwanted thoughts
C)Feeling a sense of detachment from self and the environment
D)Feeling well rested despite minimal sleep
E)Neglecting personal grooming
F)Pausing for long periods prior to responding to questions
A)Experiencing a sensation of bugs crawling on skin
B)Experiencing intrusive, unwanted thoughts
C)Feeling a sense of detachment from self and the environment
D)Feeling well rested despite minimal sleep
E)Neglecting personal grooming
F)Pausing for long periods prior to responding to questions

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
53
A 37-year-old man comes to the emergency department for evaluation of back pain. The patient was seen 2 days ago in the emergency department for similar pain symptoms and was discharged on naproxen. Medical history is significant for asthma, hepatitis C, and opioid use disorder. Temperature is 37.2 C (99 F), blood pressure is 138/92 mm Hg, and pulse is 104/min. The patient is irritable while his vital signs are being taken and angrily says to the nurse, "That medication I got was useless. My pain is now 10 times worse." His speech is very loud, filled with expletives, and disruptive to patients in adjacent rooms. His fists are clenched. Which of the following is the most appropriate next step in management of the patient interview?
A)Close the patient's room door and ask him to calm down and lower his voice
B)Inform the patient that he will not be treated if he continues to be verbally abusive
C)Inform the patient that restraints will be applied if he loses control
D)Inform the patient that security personnel will be called if he continues to be aggressive
E)Interview the patient with the door open and have security personnel nearby
A)Close the patient's room door and ask him to calm down and lower his voice
B)Inform the patient that he will not be treated if he continues to be verbally abusive
C)Inform the patient that restraints will be applied if he loses control
D)Inform the patient that security personnel will be called if he continues to be aggressive
E)Interview the patient with the door open and have security personnel nearby

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
54
A 22-year-old woman comes to student health services for evaluation of low mood and anxiety. The patient received a rejection letter a week ago from her top choice for graduate school. Although she has received multiple acceptance letters from other programs, she feels like a "failure" and has not spoken to any of her friends or family for the past few days because she is too ashamed. The patient angrily states, "I have classmates that got much worse grades and have no publications, but they all got into better schools than I did." She has been staying in bed instead of attending classes and has been eating large amounts of junk food. The patient says that her life is now "pointless" and that she would be "better off dead." She has no medical or psychiatric history. Vital signs are within normal limits. Physical examination shows no abnormalities. Which of the following is the most likely diagnosis?
A)Acute stress disorder
B)Adjustment disorder
C)Borderline personality disorder
D)Disruptive mood dysregulation disorder
E)Histrionic personality disorder
F)Major depressive disorder
A)Acute stress disorder
B)Adjustment disorder
C)Borderline personality disorder
D)Disruptive mood dysregulation disorder
E)Histrionic personality disorder
F)Major depressive disorder

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
55
A 23-year-old woman is brought to the emergency department by her roommate due to bizarre behavior. The roommate reports that, over the past few days, the patient has become increasingly paranoid. She stays up almost all night and believes the apartment is bugged. The roommate became alarmed when the patient did not go to work yesterday and started speaking in a whisper. When interviewed, the patient does not respond verbally to questions but calmly writes on a piece of paper, "I've been warned not to say anything." Her parents are contacted and report a history of depression treated with bupropion. They have never observed the behavior their daughter is exhibiting. The parents report that the patient drinks alcohol socially but do not believe she uses illicit drugs. Vital signs and physical examination are unremarkable. Family history is significant for bipolar disorder in a maternal uncle. Which of the following is the most appropriate next step in management of this patient?
A)Administer a mood stabilizer
B)Administer an antipsychotic medication
C)Obtain a bupropion blood level
D)Obtain a CT scan of the head
E)Obtain a urine toxicology screen
A)Administer a mood stabilizer
B)Administer an antipsychotic medication
C)Obtain a bupropion blood level
D)Obtain a CT scan of the head
E)Obtain a urine toxicology screen

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
56
A 24-year-old woman is brought to the emergency department due to sudden-onset difficulty breathing. She is preparing to defend her graduate school thesis at the end of the week. The patient feels that she "can't get enough air" into her lungs. Her fingertips have started tingling. She has no pain. Medical history includes allergic rhinitis and childhood eczema. Medications include nasal fluticasone. Temperature is 36.7 C (98 F), blood pressure is 110/76 mm Hg, pulse is 100/min, respirations are 20/min, and pulse oximetry is 99%. On examination, she is taking deep breaths with occasional audible deep sighs. The lungs are clear to auscultation. Cardiac auscultation is normal. Which of the following is the most appropriate treatment for this patient's condition?
A)High-dose intravenous lorazepam
B)Nebulized albuterol
C)Racemic epinephrine
D)Reassurance and breathing into a paper bag
E)Reassurance and breathing retraining
A)High-dose intravenous lorazepam
B)Nebulized albuterol
C)Racemic epinephrine
D)Reassurance and breathing into a paper bag
E)Reassurance and breathing retraining

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
57
A 57-year-old man is brought to the emergency department after being found confused and agitated in a park. Medical records indicate that he has a history of schizophrenia, alcohol use disorder, and liver cirrhosis. The patient states that he has not been taking his medications "because they never help." Temperature is 37.2 C (99 F), blood pressure is 160/80 mm Hg, pulse is 118/min, and respirations are 24/min. On examination, the patient is disheveled and disoriented, claiming that FBI agents have been chasing him. His breath smells of alcohol. Pupils are equal and reactive, and the neck is supple. The abdomen is distended but nontender. The skin and mucous membranes are dry. There is mild edema in both lower extremities but no deformity. Laboratory results are as follows:  During evaluation, the patient is initially cooperative but becomes increasingly aggressive and combative. For safety reasons, he is given intravenous haloperidol and lorazepam. Shortly afterward, the cardiac monitor displays the rhythm shown in the exhibit.
During evaluation, the patient is initially cooperative but becomes increasingly aggressive and combative. For safety reasons, he is given intravenous haloperidol and lorazepam. Shortly afterward, the cardiac monitor displays the rhythm shown in the exhibit. 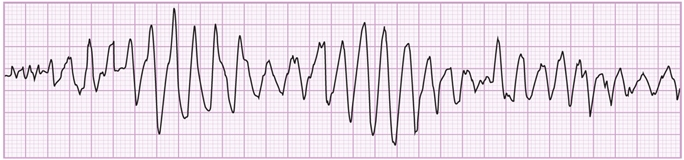 Which of the following most likely contributed to this patient's abnormal rhythm?
Which of the following most likely contributed to this patient's abnormal rhythm?
A)Elevated blood alcohol level
B)Elevated blood ammonia level
C)Haloperidol adverse effect
D)Lorazepam adverse effect
E)Low glucose level
F)Low sodium level
 During evaluation, the patient is initially cooperative but becomes increasingly aggressive and combative. For safety reasons, he is given intravenous haloperidol and lorazepam. Shortly afterward, the cardiac monitor displays the rhythm shown in the exhibit.
During evaluation, the patient is initially cooperative but becomes increasingly aggressive and combative. For safety reasons, he is given intravenous haloperidol and lorazepam. Shortly afterward, the cardiac monitor displays the rhythm shown in the exhibit. 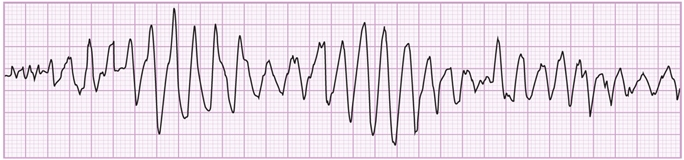 Which of the following most likely contributed to this patient's abnormal rhythm?
Which of the following most likely contributed to this patient's abnormal rhythm?A)Elevated blood alcohol level
B)Elevated blood ammonia level
C)Haloperidol adverse effect
D)Lorazepam adverse effect
E)Low glucose level
F)Low sodium level

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
58
A 26-year-old man is brought to the emergency department after an attempted suicide by medication overdose. He has had 2 seizures in the past hour. Temperature is 38.8 C (102 F), blood pressure is 90/60 mm Hg, pulse is 110/min, and respirations are 22/min. The patient is not oriented to time, place, and person. Pupils are dilated and respond poorly to light; the skin is flushed and dry. Abdominal examination shows reduced bowel sounds. ECG shows prolonged QRS complexes (0.19 sec). Toxicology studies are pending. Which of the following is the best predictor of complications due to overdose of the suspected drug?
A)Bowel sounds
B)Pupillary size
C)QRS duration
D)Serum drug levels
E)Urine drug levels
A)Bowel sounds
B)Pupillary size
C)QRS duration
D)Serum drug levels
E)Urine drug levels

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
59
A 46-year-old man with a history of medication-controlled hypertension comes to the office for a routine checkup. Blood pressure is 115/80 mm Hg and physical examination findings are normal. The physician notes that the patient's mood seems low. The patient admits that he has been "stressed out" for the past 2 months as a few people at work recently quit and he has had to take on more responsibility while management finds replacements. He has not been able to exercise or eat right as he is so busy. The patient feels irritable and tense at work and has had neck and shoulder pain. He is also worried about not being able to spend time with his wife, who complains that he works too much. The patient has occasional difficulty falling asleep at night after working long hours and feels tired during the day. Although he doesn't enjoy his job, he has no choice but to stay. He continues to get his work done and enjoys social activities, including playing golf on weekends. The patient drinks 2-3 cans of beer on weekends and smokes marijuana twice a month. Which of the following is the most likely diagnosis?
A)Acute stress disorder
B)Adjustment disorder with depressed mood
C)Generalized anxiety disorder
D)Major depressive disorder
E)Normal stress response
F)Substance/medication-induced depressive disorder
A)Acute stress disorder
B)Adjustment disorder with depressed mood
C)Generalized anxiety disorder
D)Major depressive disorder
E)Normal stress response
F)Substance/medication-induced depressive disorder

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
60
A 55-year-old man is brought by ambulance to the emergency department due to acute-onset agitation. While at work, the patient became angry during a meeting, throwing his laptop against a wall and accusing his coworkers of conspiring against him. On arrival, he is diaphoretic with flushed skin and dilated pupils. Temperature is 37.6 C (99.7 F), blood pressure is 150/90 mm Hg, pulse is 118/min, and respirations are 18/min. Physical examination shows no other abnormalities. ECG reveals sinus tachycardia and a prolonged QT interval. The patient refuses to provide a urine specimen. His voice becomes increasingly loud, and he is convinced that other patients are stealing money from him. Administration of a medication with which of the following properties is the most appropriate initial treatment?
A)Anti-beta adrenergic
B)Antidopaminergic
C)Cholinergic
D)GABA-ergic
E)Serotonergic
A)Anti-beta adrenergic
B)Antidopaminergic
C)Cholinergic
D)GABA-ergic
E)Serotonergic

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
61
A 27-year-old woman comes to the office due to headaches and neck and back pain. She has been coping with pain symptoms for several years but notes that they have increased since she was recently let go from her job as an administrative assistant. The patient worries about finding another job but says, "Most days I am just too tired to even look for work." She is also concerned about gaining weight but has no motivation to go to the gym or leave the house. The patient has been to the office twice in the past year for similar symptoms and is worried that something is wrong. At her last visit 4 months ago, laboratory testing, including a basic chemistry panel, thyroid function tests, and complete blood count, were within normal range. The patient says, "I doubt that anything will ever improve for me." Medications include ibuprofen for pain as needed. The patient drinks 1 or 2 glasses of wine 3 times a week. She has increased her use of marijuana to 3 or 4 times a week at bedtime to help her relax and fall asleep and has started smoking cigarettes after a 2-year abstinence. Family history includes hypertension and colon cancer in her father and hypothyroidism and anxiety in her mother. Vital signs and physical examination are normal except for a 2.27-kg (5-lb) weight gain since her last visit. Which of the following is the most appropriate next step in management of this patient?
A)Address her substance use with motivational interviewing
B)Examine for point tenderness
C)Explore the relationship of her symptoms to stress
D)Inquire about suicidal thoughts
E)Obtain a repeat TSH level
F)Offer reassurance and schedule regular follow-up
A)Address her substance use with motivational interviewing
B)Examine for point tenderness
C)Explore the relationship of her symptoms to stress
D)Inquire about suicidal thoughts
E)Obtain a repeat TSH level
F)Offer reassurance and schedule regular follow-up

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
62
A 25-year-old woman comes to the office due to weight gain. The patient has gained 4.5 kg (10 lb) since breaking up with her boyfriend and starting a stressful job 4 months ago. She says, "I hate the way I look. I try to limit my portions, but several times a week I end up eating a whole bag of cookies or a quart of ice cream in one sitting, even if I'm not hungry. My stomach is so bloated that I can't fit into my clothes. It is so depressing." The patient has had abdominal discomfort but no nausea or vomiting. Her weight is always fluctuating although she has tried numerous diets over the years. She also does 45 minutes of aerobic exercise 3 times a week. The patient prefers to eat alone because she feels embarrassed and "out of control." She feels guilty about her behavior, and her self-esteem is low. The patient is 160 cm (5 ft 3 in) tall and weighs 60 kg (132 lb). BMI is 23.4 kg/m2. Which of the following is the most likely diagnosis?
A)Adjustment disorder
B)Binge eating disorder
C)Body dysmorphic disorder
D)Bulimia nervosa
E)Irritable bowel syndrome
A)Adjustment disorder
B)Binge eating disorder
C)Body dysmorphic disorder
D)Bulimia nervosa
E)Irritable bowel syndrome

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
63
A 61-year-old attorney comes to the office with his wife for follow-up. Two months ago, the patient experienced an acute myocardial infarction while presenting a case in court and went into cardiac arrest. He was resuscitated in the emergency department, and a drug-eluting stent was placed. The patient recovered without complications and was discharged. He recently returned to work part-time, although his wife thinks he needs more time to rest. She states that he has been very stressed for the past month and worries that he is overworking. The patient has been sleeping restlessly and frequently wakes up startled and diaphoretic. While practicing a case presentation a few days ago, he had to stop and sit down because he felt overwhelmed. The patient plans to "take things slowly" and has asked his partner to cover upcoming court appearances. He has had no chest pain, palpitations, shortness of breath, or syncope. Medications include metoprolol, simvastatin, aspirin, and ticagrelor. Vital signs are within normal limits. Physical examination shows no abnormalities. ECG reveals no acute changes. Which of the following is the best next step in management of this patient?
A)Discontinue metoprolol
B)Initiate mirtazapine
C)Obtain an echocardiogram
D)Reassure the patient and follow up in a month
E)Recommend cognitive-behavioral therapy
A)Discontinue metoprolol
B)Initiate mirtazapine
C)Obtain an echocardiogram
D)Reassure the patient and follow up in a month
E)Recommend cognitive-behavioral therapy

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
64
A 32-year-old woman comes to the office due to feeling down for the past several months. The patient has had persistent tiredness, lack of motivation, memory impairment, and loss of libido. She also has had anorexia but reports an unusual craving for foods like salty pretzels or potato chips. Menses occur at regular intervals. The patient does not use tobacco, alcohol, or illicit drugs and works as a fashion designer. Blood pressure is 110/62 mm Hg and pulse is 88/min. BMI is 19.8 kg/m2 with weight of 54 kg (119 lb), which is 15 kg (33 lb) lower than her previous weight. The lungs are clear on auscultation and heart sounds are normal. The abdomen is soft and nontender with no organomegaly. There is decreased axillary and pubic hair. Mental status examination reveals a restricted affect. She has no suicidal ideation. Which of the following is most likely to establish the diagnosis in this patient?
A)Cosyntropin stimulation testing
B)CT scan of the chest, abdomen, and pelvis
C)Detailed nutritional history
D)HIV antigen and antibody testing
E)Trial of antidepressant therapy
A)Cosyntropin stimulation testing
B)CT scan of the chest, abdomen, and pelvis
C)Detailed nutritional history
D)HIV antigen and antibody testing
E)Trial of antidepressant therapy

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
65
A 32-year-old physician comes to the office due to insomnia for the past 6 weeks. He says, "I feel restless at night, and I can't get any sleep. I've tried reading boring books and drinking herbal teas, but nothing seems to help." The patient feels his lack of sleep has made it difficult to focus and started drinking 2 cups of coffee before his shifts "to get through the day." He previously worked in the emergency department but switched to doing shifts at an urgent care clinic a month ago. The patient says, "I was seeing a lot of gunshot wounds at the hospital. Compared to my old job, this one is much calmer, but I still feel anxious a lot of the time." He still thinks about patients he treated and what he could have done differently to save them. The patient says, "The world has just gotten too dangerous, and I feel like medicine can't keep up with it." He drinks 3-4 beers on the weekends and does not use tobacco or illicit drugs. Medical history is noncontributory. Temperature is 37 C (98.6 F), blood pressure is 130/80 mm Hg, pulse is 84/min, and respirations are 16/min. Physical examination is unremarkable. The patient appears tired and speaks in a low volume. Which of the following is the most appropriate next step in management of this patient?
A)Advise the patient to discontinue caffeine use
B)Prescribe low-dose lorazepam
C)Prescribe melatonin
D)Prescribe paroxetine
E)Provide reassurance and follow-up in 2 weeks
A)Advise the patient to discontinue caffeine use
B)Prescribe low-dose lorazepam
C)Prescribe melatonin
D)Prescribe paroxetine
E)Provide reassurance and follow-up in 2 weeks

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
66
A 44-year-old woman comes to the office due to worsening anxiety. Prior to starting her new job 3 months ago, the patient had not suffered from anxiety or any other psychiatric condition. She experiences the demands of her new job as overwhelming and disproportionate to the support and resources she has available at work. Around the same time that she started her new job, the patient began to suffer sudden episodes of palpitations, sweating, pounding headache, and panicky feelings that have recurred every few days for no apparent reason. The patient was also recently diagnosed with hypertension that has only slightly improved with antihypertensive medication. Temperature is 37.2 C (99 F), blood pressure is 184/86 mm Hg, pulse is 91/min, and respirations are 14/min. BMI is 23 kg/m2. The patient appears anxious, mildly tremulous, and diaphoretic on examination. Laboratory results are as follows:  Which of the following is the most likely explanation for this patient's symptoms?
Which of the following is the most likely explanation for this patient's symptoms?
A)Acute intermittent porphyria
B)Carcinoid syndrome
C)Generalized anxiety disorder
D)Hyperthyroidism
E)Insulinoma
F)Panic disorder
G)Pheochromocytoma
 Which of the following is the most likely explanation for this patient's symptoms?
Which of the following is the most likely explanation for this patient's symptoms?A)Acute intermittent porphyria
B)Carcinoid syndrome
C)Generalized anxiety disorder
D)Hyperthyroidism
E)Insulinoma
F)Panic disorder
G)Pheochromocytoma

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
67
A 66-year-old man comes to the office to follow up on his prostate cancer treatment. The patient has painful, bony metastasis in the pelvis and is being treated with hormonal therapy and radiotherapy. He has been receiving long-acting and as-needed short-acting morphine, but he continues to have significant pain. In the past 2 weeks, the patient has also experienced insomnia due to the pain, leading to worsening fatigue. He has no nausea, constipation, drowsiness, or suicidal ideation. Urine drug screen is positive for opioids and negative for other substances. A review of the state prescription drug monitoring program database reveals no irregularities. In addition to titration of opioid therapy to improve pain control, which of the following responses is the most appropriate recommendation for this patient?
A)"Bone pain is especially difficult to treat. Let's try a medication called calcitonin."
B)"I'll prescribe you clonazepam every night to help with sleep."
C)"I'll prescribe naloxone in case of overdose and talk to your family about how to use it."
D)"To prevent addiction, I'll prescribe naltrexone to lessen the euphoria associated with morphine."
A)"Bone pain is especially difficult to treat. Let's try a medication called calcitonin."
B)"I'll prescribe you clonazepam every night to help with sleep."
C)"I'll prescribe naloxone in case of overdose and talk to your family about how to use it."
D)"To prevent addiction, I'll prescribe naltrexone to lessen the euphoria associated with morphine."

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
68
A 33-year-old woman comes to the office for "help losing weight." She says, "I'm really trying, but I haven't seen any results." The patient has been on restrictive diets that cut out various food groups but gained 5 pounds in the past month. She feels "defeated" and says, "Nothing I try works. I end up feeling sorry for myself, and before I know it, I've eaten an entire cake. Even though I feel disgusting afterward, I still do it a few times a week." She reports no difficulty with sleep, energy, or concentration. The patient has been avoiding meals with friends and family because of embarrassment about overeating. Medical history is insignificant. Mental status examination reveals an overweight woman wearing loose clothing. She is cooperative and has a reactive affect. Treatment options are discussed, and the patient prefers to start medication. Which of the following medications would be most appropriate for this patient?
A)Bupropion
B)Lamotrigine
C)Orlistat
D)Phentermine
E)Sertraline
A)Bupropion
B)Lamotrigine
C)Orlistat
D)Phentermine
E)Sertraline

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
69
A 36-year-old woman comes to the office due to difficulty losing weight over the past several months. The patient says, "I typically lose 1 or 2 pounds in the first week of dieting, but by the second week I lose control and start eating bags of cookies and potato chips." These episodes are followed by a few days of fasting and exercising excessively. The patient is upset about her weight and appearance but has no persistent sadness. She enjoys her work and socializing with friends and family. The patient has no medical conditions, but her menstrual cycle is irregular. Weight is 67 kg (147.7 lb) and height is 160 cm (5 ft 3 in). BMI is 26.2 kg/m2. Blood pressure is 100/70 mm Hg and pulse is 86/min. Physical examination shows dry skin but is otherwise unremarkable. The patient has a full range of affect and no suicidal ideation. Laboratory results are as follows:  The diagnosis is discussed, and the patient asks if any medications are available for treatment. Which of the following is the most appropriate recommendation?
The diagnosis is discussed, and the patient asks if any medications are available for treatment. Which of the following is the most appropriate recommendation?
A)Bupropion
B)Fluoxetine
C)Methylphenidate
D)No pharmacological therapy is effective
E)Olanzapine
F)Orlistat
 The diagnosis is discussed, and the patient asks if any medications are available for treatment. Which of the following is the most appropriate recommendation?
The diagnosis is discussed, and the patient asks if any medications are available for treatment. Which of the following is the most appropriate recommendation?A)Bupropion
B)Fluoxetine
C)Methylphenidate
D)No pharmacological therapy is effective
E)Olanzapine
F)Orlistat

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
70
A 54-year-old man comes to the office due to chronic fatigue, decreased concentration, and depressed mood that began about a year ago. The patient says, "I think it all began last year when my wife and I started to fight more than usual. I was having a hard time concentrating at work and was eventually fired, which caused a lot of financial stress that spilled over into our marriage. Pretty soon, my wife started sleeping in the guest room; she said it was because my snoring was getting worse, but I think she was just sick of me." The patient acknowledges sleeping very poorly and awakening multiple times each night. He struggles to look for a new job because he feels so tired throughout the day. He has a history of hypercholesterolemia and hypertension. He has no known psychiatric history. Medications include hydrochlorothiazide and lovastatin. The patient drinks alcohol socially, although he has been avoiding social gatherings recently despite previously enjoying being around others. He is 175 cm (5 ft 9 in) tall and weighs 118 kg (260 lb); blood pressure is 140/85 mm Hg and pulse is 78/min. Physical examination shows no other abnormalities. Laboratory values are within normal range. Mental status examination shows depressed mood with a full range of affect and no suicidal ideation. Which of the following is the most likely diagnosis in this patient?
A)Adjustment disorder with depressed mood
B)Depressive disorder due to another medical condition
C)Major depressive disorder
D)Medication-induced depressive disorder
E)Persistent depressive disorder, dysthymia
F)Substance-induced depressive disorder
A)Adjustment disorder with depressed mood
B)Depressive disorder due to another medical condition
C)Major depressive disorder
D)Medication-induced depressive disorder
E)Persistent depressive disorder, dysthymia
F)Substance-induced depressive disorder

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
71
A 33-year-old man comes to the office with his wife due to marital difficulties. His wife says, "I came back from a work trip last week, and now my husband is convinced I'm having an affair with my coworker." She says that he is constantly demanding to look at her phone and has grabbed it from her several times. The husband says that he has always struggled with his temper, that he shouts with little provocation and his moods go up and down throughout the day. His wife asks if medication would help "balance him out." She describes how he binges on alcohol "every few months" when he feels low. He has had 2 minor car crashes while intoxicated and bought expensive cars after each one, which resulted in significant debt. Prior to their marriage 2 years ago, the patient had multiple short-lived relationships, each of which ended abruptly. He says, "My ex-girlfriends were terrible-they never cared about me." The patient expresses remorse for upsetting his wife and begs her not to leave him. Which of the following is the most likely diagnosis?
A)Bipolar II disorder
B)Borderline personality disorder
C)Delusional disorder
D)Disruptive mood dysregulation disorder
E)Paranoid personality disorder
A)Bipolar II disorder
B)Borderline personality disorder
C)Delusional disorder
D)Disruptive mood dysregulation disorder
E)Paranoid personality disorder

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
72
A 38-year-old man is evaluated for a 2-month history of depressed mood. He explains, "I'm just exhausted all the time. I can't sleep. I can't think. I just feel worn out." During further discussion, the patient tearfully admits to thoughts of suicide but has no plan or intent to act on these thoughts. He has no medical conditions. Family history is significant for type 2 diabetes mellitus and hypertension in his father and hyperthyroidism in his mother. After physical examination and laboratory workup, major depressive disorder is diagnosed and antidepressant therapy is initiated. The patient's symptoms do not respond to monotherapy, so an antipsychotic medication is added. Over the course of several months, the patient's antidepressant dose is increased to the maximal therapeutic dose. At his 6-month follow-up, the patient's mood is improved and his depression is in remission. Temperature is 36.7 C (98.1 F), blood pressure is 148/91 mm Hg, pulse is 72/min, and respirations are 14/min. Compared to his most recent visit, he has lost 0.5 kg (1.1 lb); he has also new-onset hypertension. Which of the following medications is the most likely cause of this adverse effect?
A)Aripiprazole
B)Mirtazapine
C)Paroxetine
D)Phenelzine
E)Sertraline
F)Venlafaxine
G)Ziprasidone
A)Aripiprazole
B)Mirtazapine
C)Paroxetine
D)Phenelzine
E)Sertraline
F)Venlafaxine
G)Ziprasidone

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
73
A 25-year-old woman comes to the office due to abdominal bloating, headache, fatigue, weight gain, mood swings, and decreased libido. She says, "The symptoms last about a week and then seem to subside, but they always come back again." During these episodes, her appetite increases and she craves sweet and salty foods. The episodes have been occurring for years. The patient has a history of depression as a teenager that responded well to cognitive-behavioral therapy and a family history of bipolar disorder in a maternal uncle. She has no recent change in sleep pattern or interest in activities, or feelings of hopelessness or guilt. She takes no medications and physical examination is normal. Complete blood count, serum chemistries, pregnancy test, and TSH levels are within normal limits. Which of the following is the most appropriate next step in management of this patient?
A)Cognitive-behavioral therapy
B)Fluoxetine
C)Gluten-free diet
D)Luteal-phase-only fluoxetine
E)Menstrual diary
F)Valproate
G)Vitamin B6
A)Cognitive-behavioral therapy
B)Fluoxetine
C)Gluten-free diet
D)Luteal-phase-only fluoxetine
E)Menstrual diary
F)Valproate
G)Vitamin B6

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
74
A 38-year-old man comes to the office due to disturbed sleep and depressed mood for the past several months. The patient has difficulty falling and staying asleep and says, "I lie awake at night thinking about all the weight I've gained and how I am too tired to even do anything about it." He constantly feels exhausted at work, which involves "sitting all day in a cubicle." The patient has also felt depressed and irritable, which he attributes to his appearance. He has no previous medical conditions and takes no medications. Family history is significant for bipolar disorder in his brother. Temperature is 36.8 C (98.2 F), blood pressure is 148/90 mm Hg, and pulse is 86/min. BMI is 34 kg/m2. On physical examination, the patient has a flat affect and a ruddy appearance with central obesity. The thyroid is normal to palpation. The lungs are clear to auscultation and heart sounds are normal. The abdomen is soft and nontender. There is no extremity edema. Proximal limb muscles are mildly weak with no associated pain or tenderness. The patient is tearful throughout the evaluation but has no suicidal ideation. Laboratory results are as follows:  Which of the following is the most appropriate next step in management of this patient?
Which of the following is the most appropriate next step in management of this patient?
A)Check anti-Jo-1 antibody titer
B)Measure urinary free cortisol
C)Obtain serum insulin-like growth factor-1
D)Prescribe low-dose paroxetine
E)Recommend cognitive-behavioral therapy
F)Refer for bariatric surgery evaluation
 Which of the following is the most appropriate next step in management of this patient?
Which of the following is the most appropriate next step in management of this patient?A)Check anti-Jo-1 antibody titer
B)Measure urinary free cortisol
C)Obtain serum insulin-like growth factor-1
D)Prescribe low-dose paroxetine
E)Recommend cognitive-behavioral therapy
F)Refer for bariatric surgery evaluation

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
75
A 58-year-old man is brought to the office by his daughter for evaluation of "abnormal behavior." The patient has been anxious and irritable for the past several days, and over the past 2 days, he has repeatedly said that "bad men" are following him. He has no history of psychiatric illness but was diagnosed with polymyositis 2 weeks ago. The patient has been taking high-dose prednisone with improvement in muscle weakness. He has no other medical conditions and takes no other medications. Vital signs are within normal limits. Physical examination shows mild symmetric, proximal muscle weakness. During the examination, the patient frequently looks around the room and startles easily when the nurse knocks on the door. He reports no suicidal ideation or hallucinations. Based on the patient's responses to questions, his memory and recall are intact. Which of the following is the most appropriate first step in the management of this patient's current symptoms?
A)Add haloperidol
B)Add quetiapine
C)Decrease prednisone dosage
D)Order brain MRI
E)Perform lumbar puncture
F)Provide reassurance only
A)Add haloperidol
B)Add quetiapine
C)Decrease prednisone dosage
D)Order brain MRI
E)Perform lumbar puncture
F)Provide reassurance only

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
76
A 46-year-old woman with alcohol use disorder comes to the office for follow-up. The patient has a prolonged history of heavy alcohol use and was hospitalized 6 months ago due to alcohol-induced pancreatitis. She stopped drinking after the hospitalization but restarted following a fight with her husband a month ago. Her daughters convinced her to stop again, and she has had no drinks for the past 2 weeks. The patient reports no anxiety or shakiness but has had occasional cravings and is afraid that she may relapse again. She has no other medical conditions, takes no medications, and does not use tobacco or illicit drugs. Vital signs are within normal limits, and physical examination shows no abnormalities. In addition to psychosocial interventions, which of the following is the most appropriate pharmacotherapy for this patient?
A)Acamprosate
B)Chlordiazepoxide
C)Disulfiram
D)Fomepizole
E)Naloxone
A)Acamprosate
B)Chlordiazepoxide
C)Disulfiram
D)Fomepizole
E)Naloxone

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
77
A 24-year-old man is brought to the emergency department by his wife due to bizarre behavior. She noticed a change in his behavior shortly after he started a fasting diet 4-5 days ago. He has become irritable and moody and has been snapping at his wife and children. The patient says that he is being haunted by large, shadowy figures that "come from another world and are trying to take me with them." He has anxiety, is sleeping less than usual, and has stopped going to work. The patient also has abdominal pain, constipation, and a tingling sensation in his fingertips. Medical history includes major depression and gastroesophageal reflux disease. His father also suffered from unexplained psychiatric episodes. The patient does not use tobacco, alcohol, or illicit drugs. His medications include omeprazole and acetaminophen. Temperature is 36.7 C (98.1 F), blood pressure is 140/80 mm Hg, pulse is 110/min, and respirations are 16/min. The abdomen is soft, bowel sounds are decreased, and there is no rebound tenderness or rigidity. Neurologic examination is within normal limits except for decreased sensation in the fingertips and mild weakness in the right arm. Which of the following is the most likely diagnosis in this patient?
A)Acute intermittent porphyria
B)Lyme disease
C)Major depressive episode with psychotic features
D)Schizophrenia
E)Wilson disease
A)Acute intermittent porphyria
B)Lyme disease
C)Major depressive episode with psychotic features
D)Schizophrenia
E)Wilson disease

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
78
A 15-year-old boy is brought to the office by his parents due to concern about a change in his behavior. Over the past 3 months he has become more withdrawn, spending more time alone and turning down opportunities to socialize with his friends. He is frequently moody and irritable. The patient feels unmotivated at school and seems unconcerned that his grades have dropped. His parents believe that his behavior changed after he was rejected by a girl, who subsequently called him a "loser" on social media. When seen alone, the patient says, "I don't think I will ever get over this girl," who he believes was his "soul mate." He uses marijuana occasionally but does not use alcohol. Physical examination is normal apart from a 2.7-kg (6-lb) weight loss since his last visit. He says, "I feel pretty down. I would consider talking to someone or taking medication but don't want to worry my parents." Which of the following is the most appropriate step prior to initiating treatment for this patient?
A)Assure the patient that everything he says is confidential
B)Discuss the risks and benefits of psychotherapy versus medication
C)Encourage the patient to tell his parents how he feels
D)Inform the patient that parental permission is needed to prescribe medication
E)Inquire if the patient has thoughts of harming himself
F)Reassure the patient that sadness is normal after a romantic breakup
G)Recommend psychotherapy in addition to medication
A)Assure the patient that everything he says is confidential
B)Discuss the risks and benefits of psychotherapy versus medication
C)Encourage the patient to tell his parents how he feels
D)Inform the patient that parental permission is needed to prescribe medication
E)Inquire if the patient has thoughts of harming himself
F)Reassure the patient that sadness is normal after a romantic breakup
G)Recommend psychotherapy in addition to medication

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
79
A 22-year-old man comes to the office due to difficulty concentrating and sleeping. The patient lost his job and moved in with his parents 2 months ago. Although he has been looking for work and revising his resume, he gets distracted and easily loses focus. The patient has not received any interview invitations and is worried that he will be living with his parents for a long time. He feels that he has "reverted to my high school self," playing video games most evenings and going out with friends on the weekends. The patient gets annoyed with his parents occasionally but states that he knows they are "just trying to be helpful." He has been eating more than usual since moving, gaining 3 kg (6.6 lb) and feeling tired during the day. The patient takes 2-3 hours to fall asleep each night and frequently checks the time while in bed. He drinks 3 or 4 beers a week and does not use recreational substances. Vital signs are within normal limits. Physical examination shows no abnormalities. The patient states that his mood is "okay," and he has a full range of affect. He reports no suicidal ideation. In addition to recommending psychotherapy, which of the following is the most appropriate pharmacotherapy for this patient?
A)Alprazolam
B)Lithium
C)Methylphenidate
D)Quetiapine
E)Zolpidem
A)Alprazolam
B)Lithium
C)Methylphenidate
D)Quetiapine
E)Zolpidem

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck
80
A 19-year-old man is brought to the office by his mother due to sad mood and declining grades at college. Previously a straight-A student, he is now getting Cs and Ds, and his mother worries he will not complete his freshman year. The patient says, "I feel depressed and hopeless about the future." He has little interest in his classes, has difficulty concentrating on assignments, and abruptly decided to quit the soccer team. He refuses to answer any phone calls from his friends and keeps himself isolated at home. The patient feels that there is little point in living but has no suicidal intent or plan. He has tried alcohol at parties on 2 occasions but does not use illicit drugs. There is no history of mania. There is a family history of untreated depression in his mother and grandmother. Physical examination and laboratory values are normal. Major depressive disorder is diagnosed, and treatment is discussed. The patient is willing to take medication, but his mother is concerned that antidepressants can cause people to become suicidal. Which of the following is the most appropriate response to the mother?
A)Due to the slightly increased risk of suicidal thoughts in adolescents, antidepressants are prescribed only for patients who fail psychotherapy.
B)Some classes of antidepressants have a lower risk of increasing suicidal thoughts, and for adolescents we prescribe those first.
C)There is a slightly increased risk of suicidal thoughts in young people treated with antidepressants, but only in those under age 18.
D)There is no association between antidepressants and an increased risk of suicidal thoughts in adolescents.
E)The slightly increased risk of suicidal thoughts with antidepressants in this age group needs to be weighed against the risk of completed suicide in untreated depression.
A)Due to the slightly increased risk of suicidal thoughts in adolescents, antidepressants are prescribed only for patients who fail psychotherapy.
B)Some classes of antidepressants have a lower risk of increasing suicidal thoughts, and for adolescents we prescribe those first.
C)There is a slightly increased risk of suicidal thoughts in young people treated with antidepressants, but only in those under age 18.
D)There is no association between antidepressants and an increased risk of suicidal thoughts in adolescents.
E)The slightly increased risk of suicidal thoughts with antidepressants in this age group needs to be weighed against the risk of completed suicide in untreated depression.

Unlock Deck
Unlock for access to all 336 flashcards in this deck.
Unlock Deck
k this deck



