Deck 1: STEP 2 CS - Sample Cases
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question

Unlock Deck
Sign up to unlock the cards in this deck!
Unlock Deck
Unlock Deck
1/31
Play
Full screen (f)
Deck 1: STEP 2 CS - Sample Cases
1
Doorway information about patient
The patient is a 55-year-old man brought in by his wife to discuss ways for him to stop drinking alcohol.
Vital signs
Temperature: 36.7 C (98.0 F)
Blood pressure: 110/70 mm Hg
Pulse: 80/min
Respiratory rate: 14/min
The patient is a 55-year-old man brought in by his wife to discuss ways for him to stop drinking alcohol.
Vital signs
Temperature: 36.7 C (98.0 F)
Blood pressure: 110/70 mm Hg
Pulse: 80/min
Respiratory rate: 14/min
Approach to the patient
Patients should be evaluated for unhealthy alcohol use if they have:
Excessive intake (men: >14 drinks/week or >4 drinks/day; women: >7 drinks/week or >3 drinks/day)
Impairment in social or occupational function
Legal or social consequences (eg, loss of job, arrest for driving while intoxicated)
Adverse health effects (eg, liver toxicity, resistant hypertension)
The evaluation of alcohol use disorders should address current alcohol intake, personal and family history of alcohol abuse and treatment, and medical and psychological complications of alcohol intake. Patients should also be screened for abuse of other substances (eg, tobacco, illicit drugs, prescription medications) and for comorbid psychiatric illnesses.
Differential diagnosis
The differential diagnosis for alcohol use disorder is usually straightforward. However, patients may have additional probems that need to be identified and addressed. The following disorders should be considered when evaluating a patient with alcohol abuse:
Polysubstance abuse
Affective disorders (eg, bipolar disorder, major depression)
Anxiety disorders (eg, post-traumatic stress disorder, panic disorder)
Chronic insomnia
Personality disorders (eg, antisocial personality disorder)
Dementia
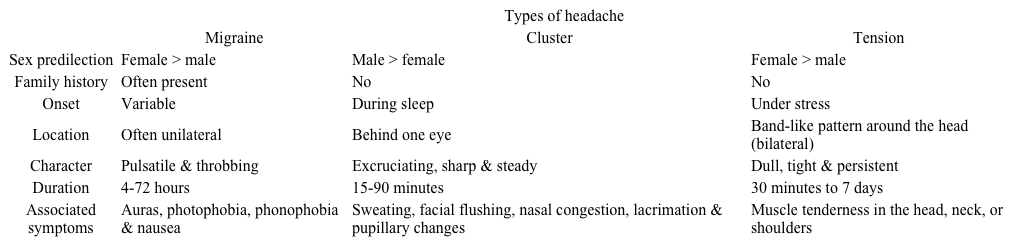
History and physical examination
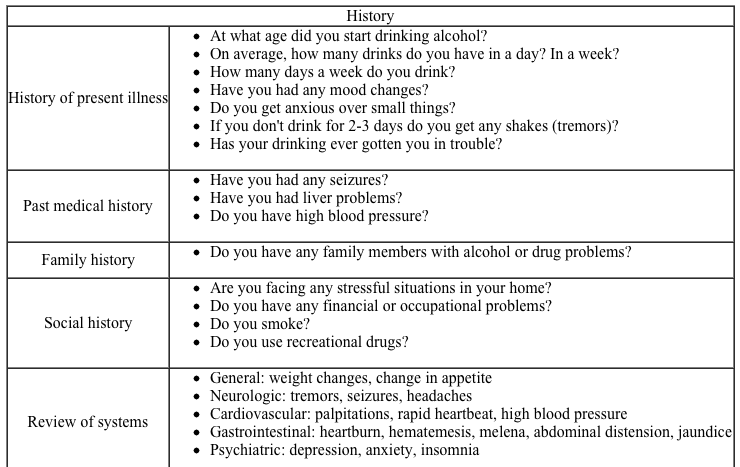
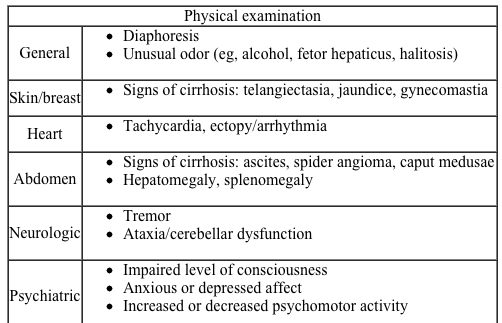
The initial screen for unhealthy alcohol use can utilize single-item screening, or the AUDIT or AUDIT-C test. The CAGE questions are helpful in further characterizing alcohol use in patients who are positive on the initial screen.
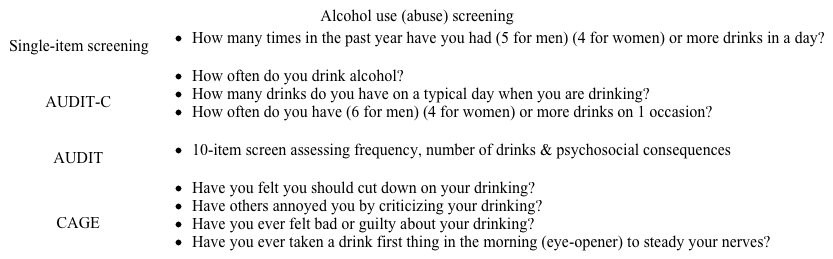 The following sections include additional items that may be useful in evaluation of a patient with alcohol abuse.
The following sections include additional items that may be useful in evaluation of a patient with alcohol abuse.
 Closing the encounter
Closing the encounter
Patients with alcohol abuse have frequently faced interpersonal conflicts and criticism from family, friends, and coworkers. For this reason, it is essential to convey empathy and use nonjudgmental language when conducting the interview. Adverse findings (eg, signs of cirrhosis) should be noted and discussed in a straightforward manner, but "lectures" are rarely helpful. Although treatment and disposition (eg, admit to alcohol treatment facility) are beyond the scope of the USMLE Step 2 CS exam, you should inquire about patients' desire for treatment and provide assurance that you will continue to work with them to address their medical problems.
Diagnostic studies
The diagnosis of alcohol use disorder is based on clinical findings. Additional testing is ordered only as necessary to evaluate potential medical complications (eg, alcoholic liver disease) and comorbidities. The following studies should be considered as the individual case warrants:
CBC
Hepatic transaminases (AST, ALT, gamma-glutamyltransferase), albumin
Coagulation markers (prothrombin time, partial thromboplastin time)
Hepatitis serologies (hepatitis A, B, C)
Liver ultrasound
Patients should be evaluated for unhealthy alcohol use if they have:
Excessive intake (men: >14 drinks/week or >4 drinks/day; women: >7 drinks/week or >3 drinks/day)
Impairment in social or occupational function
Legal or social consequences (eg, loss of job, arrest for driving while intoxicated)
Adverse health effects (eg, liver toxicity, resistant hypertension)
The evaluation of alcohol use disorders should address current alcohol intake, personal and family history of alcohol abuse and treatment, and medical and psychological complications of alcohol intake. Patients should also be screened for abuse of other substances (eg, tobacco, illicit drugs, prescription medications) and for comorbid psychiatric illnesses.
Differential diagnosis
The differential diagnosis for alcohol use disorder is usually straightforward. However, patients may have additional probems that need to be identified and addressed. The following disorders should be considered when evaluating a patient with alcohol abuse:
Polysubstance abuse
Affective disorders (eg, bipolar disorder, major depression)
Anxiety disorders (eg, post-traumatic stress disorder, panic disorder)
Chronic insomnia
Personality disorders (eg, antisocial personality disorder)
Dementia
History and physical examination
The initial screen for unhealthy alcohol use can utilize single-item screening, or the AUDIT or AUDIT-C test. The CAGE questions are helpful in further characterizing alcohol use in patients who are positive on the initial screen.
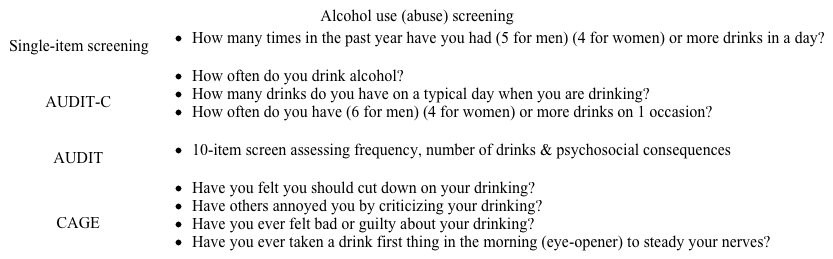 The following sections include additional items that may be useful in evaluation of a patient with alcohol abuse.
The following sections include additional items that may be useful in evaluation of a patient with alcohol abuse.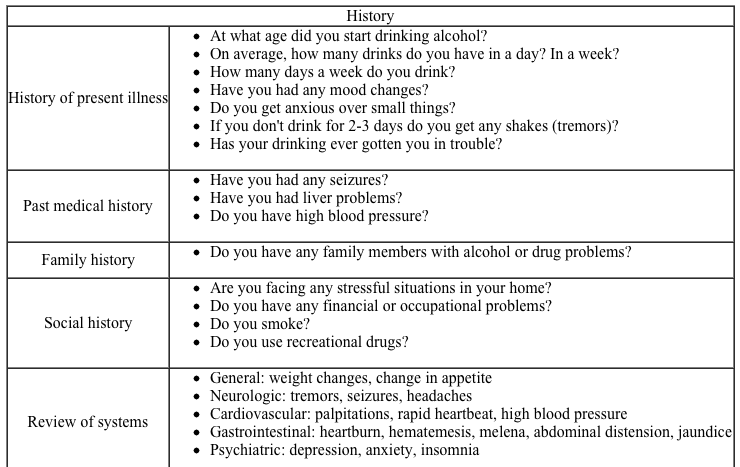
 Closing the encounter
Closing the encounterPatients with alcohol abuse have frequently faced interpersonal conflicts and criticism from family, friends, and coworkers. For this reason, it is essential to convey empathy and use nonjudgmental language when conducting the interview. Adverse findings (eg, signs of cirrhosis) should be noted and discussed in a straightforward manner, but "lectures" are rarely helpful. Although treatment and disposition (eg, admit to alcohol treatment facility) are beyond the scope of the USMLE Step 2 CS exam, you should inquire about patients' desire for treatment and provide assurance that you will continue to work with them to address their medical problems.
Diagnostic studies
The diagnosis of alcohol use disorder is based on clinical findings. Additional testing is ordered only as necessary to evaluate potential medical complications (eg, alcoholic liver disease) and comorbidities. The following studies should be considered as the individual case warrants:
CBC
Hepatic transaminases (AST, ALT, gamma-glutamyltransferase), albumin
Coagulation markers (prothrombin time, partial thromboplastin time)
Hepatitis serologies (hepatitis A, B, C)
Liver ultrasound
2
Doorway information about patient
The patient is a 20-year-old man who comes to the clinic due to dark urine for 5 days.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 122/80 mm Hg
Pulse: 74/min
Respirations: 14/min
The patient is a 20-year-old man who comes to the clinic due to dark urine for 5 days.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 122/80 mm Hg
Pulse: 74/min
Respirations: 14/min
Approach to the patient
Patients may report unusual or undifferentiated symptoms that could be due to disease in multiple systems. In some cases, this may represent a cardinal manifestation of an uncommon condition (eg, the "target shaped" rash of Lyme disease). Alternately, unusual symptoms may be an atypical manifestation of a common disorder (eg, systemic lupus erythematosus presenting as migratory mononeuropathy).
When evaluating a patient with nonspecific symptoms, review the medical history, risk factors, and medications to identify what disorders and complications are most likely. Identify the system involved, and consider what disorders are most likely to affect that system in the patient.
Dark urine can represent either an unusually concentrated urine, hematuria, or an abnormal pigment in the urine. Abnormal urine color is usually due to disorders of the renourinary tract, hepatobiliary system, blood/hematologic system, or musculoskeletal system. If the patient otherwise feels well, abnormal urine color is usually benign.
Differential diagnosis
The color of the urine can guide the differential diagnosis:
Red: Blood, food pigments (eg, beets, rhubarb), medications (eg, phenazopyridine, rifampin), porphyrins
Blue/green: Food dyes, medications (eg, indomethacin, amitriptyline), Pseudomonas urinary tract infection
Brown: Medications (eg, metronidazole, senna), liver/kidney disease, myoglobin/rhabdomyolysis
Orange: Hepatobiliary disease, dehydration
Hematuria can be categorized by the pattern through urination. Blood at the start of voiding that clears is usually from a urethral source. Blood at the end of voiding suggests a bladder or prostate source. Visible blood throughout voiding may represent an upper tract (kidney and collecting system) source.
Biliary obstruction may cause dark-yellow/orange urine with jaundice, pale stools, and right upper quandrant pain. Hematuria in a patient with a history of heavy smoking is a common presentation of bladder cancer. Dark urine following a crush injury or extreme physical exertion suggests rhabdomyolysis. In addition, hemolysis may cause dark urine with fatigue, jaundice, and back or abdominal pain.
History and physical examination
In addition to the standard general medical history and physical examination, the following sections include the most common items that should be included in the evaluation of a patient with dark urine.
![<strong>Approach to the patient</strong> Patients may report unusual or undifferentiated symptoms that could be due to disease in multiple systems. In some cases, this may represent a <strong>cardinal manifestation</strong> of an uncommon condition (eg, the target shaped rash of Lyme disease). Alternately, unusual symptoms may be an <strong>atypical manifestation</strong> of a common disorder (eg, systemic lupus erythematosus presenting as migratory mononeuropathy). When evaluating a patient with nonspecific symptoms, review the medical history, risk factors, and medications to identify what disorders and complications are most likely. Identify the system involved, and consider what disorders are most likely to affect that system in the patient. Dark urine can represent either an unusually concentrated urine, hematuria, or an <strong>abnormal pigment</strong> in the urine. Abnormal urine color is usually due to disorders of the renourinary tract, hepatobiliary system, blood/hematologic system, or musculoskeletal system. If the patient otherwise feels well, abnormal urine color is usually benign. <strong>Differential diagnosis</strong> The color of the urine can guide the differential diagnosis: <strong>Red</strong>: Blood, food pigments (eg, beets, rhubarb), medications (eg, phenazopyridine, rifampin), porphyrins <strong>Blue/green</strong>: Food dyes, medications (eg, indomethacin, amitriptyline), Pseudomonas urinary tract infection <strong>Brown</strong>: Medications (eg, metronidazole, senna), liver/kidney disease, myoglobin/rhabdomyolysis <strong>Orange</strong>: Hepatobiliary disease, dehydration <strong>Hematuria</strong> can be categorized by the pattern through urination. Blood at the start of voiding that clears is usually from a urethral source. Blood at the end of voiding suggests a bladder or prostate source. Visible blood throughout voiding may represent an upper tract (kidney and collecting system) source. <strong>Biliary obstruction</strong> may cause dark-yellow/orange urine with jaundice, pale stools, and right upper quandrant pain. Hematuria in a patient with a history of heavy smoking is a common presentation of <strong>bladder cancer</strong>. Dark urine following a crush injury or extreme physical exertion suggests <strong>rhabdomyolysis</strong>. In addition,<strong> hemolysis</strong> may cause dark urine with fatigue, jaundice, and back or abdominal pain. <strong>History and physical examination</strong> In addition to the standard general medical history and physical examination, the following sections include the most common items that should be included in the evaluation of a patient with dark urine. <strong>Closing the encounter</strong> In the wrap-up discussion, the first step is to discuss the likely diagnosis along with an assessment of the diagnostic uncertainty. If a patient has pathognomonic findings for a particular disease, you should explain the significance of them. If you are uncertain about the diagnosis, say so clearly, but reassure the patient that you will work with them to identify the cause. Regarding diagnostic tests, if invasive studies are necessary (eg, cystoscopy in an elderly smoker with hematuria), explain the rationale for the tests. Allow time for questions, and assess the patient's readiness to undergo the studies you recommend. <strong>Diagnostic studies</strong> Patients with an abnormal urine color should have a urinalysis with microscopic analysis of urinary sediment (ie, for casts, crystals, etc.). Note that patients with myoglobinuria may have a positive test for hemoglobin on chemical (dip stick) urinalysis without red blood cells on microscopic analysis. Other studies may include: Electrolytes, blood urea nitrogen, creatinine Liver function tests (eg, direct and indirect bilirubin) Urine culture Complete blood count (and peripheral smear, reticulocyte count) Muscle enzymes (eg, creatinine kinase, aspartate aminotransferase [AST]) CT urogram (for identifying kidney stones) Liver/biliary CT scan, ultrasound Cystoscopy Patients with hematuria should have evaluation of both the upper and lower urinary tract. Typical studies include CT urogram and cystoscopy, but the specific evaluation may be individualized. If hemolytic anemia is suspected, start with a complete blood count, reticulocyte count, and peripheral smear. Supportive findings include elevated lactate dehydrogenase, low haptoglobin, and elevated unconjugated bilirubin. These should be performed before more specific testing (eg, hemoglobin electrophoresis, glucose-6-phosphate dehydrogenase, osmotic fragility).](https://d2lvgg3v3hfg70.cloudfront.net/MD0004/11ec25d3_0de4_8555_bf52_57665ff6ea7e_MD0004_00.jpg)
![<strong>Approach to the patient</strong> Patients may report unusual or undifferentiated symptoms that could be due to disease in multiple systems. In some cases, this may represent a <strong>cardinal manifestation</strong> of an uncommon condition (eg, the target shaped rash of Lyme disease). Alternately, unusual symptoms may be an <strong>atypical manifestation</strong> of a common disorder (eg, systemic lupus erythematosus presenting as migratory mononeuropathy). When evaluating a patient with nonspecific symptoms, review the medical history, risk factors, and medications to identify what disorders and complications are most likely. Identify the system involved, and consider what disorders are most likely to affect that system in the patient. Dark urine can represent either an unusually concentrated urine, hematuria, or an <strong>abnormal pigment</strong> in the urine. Abnormal urine color is usually due to disorders of the renourinary tract, hepatobiliary system, blood/hematologic system, or musculoskeletal system. If the patient otherwise feels well, abnormal urine color is usually benign. <strong>Differential diagnosis</strong> The color of the urine can guide the differential diagnosis: <strong>Red</strong>: Blood, food pigments (eg, beets, rhubarb), medications (eg, phenazopyridine, rifampin), porphyrins <strong>Blue/green</strong>: Food dyes, medications (eg, indomethacin, amitriptyline), Pseudomonas urinary tract infection <strong>Brown</strong>: Medications (eg, metronidazole, senna), liver/kidney disease, myoglobin/rhabdomyolysis <strong>Orange</strong>: Hepatobiliary disease, dehydration <strong>Hematuria</strong> can be categorized by the pattern through urination. Blood at the start of voiding that clears is usually from a urethral source. Blood at the end of voiding suggests a bladder or prostate source. Visible blood throughout voiding may represent an upper tract (kidney and collecting system) source. <strong>Biliary obstruction</strong> may cause dark-yellow/orange urine with jaundice, pale stools, and right upper quandrant pain. Hematuria in a patient with a history of heavy smoking is a common presentation of <strong>bladder cancer</strong>. Dark urine following a crush injury or extreme physical exertion suggests <strong>rhabdomyolysis</strong>. In addition,<strong> hemolysis</strong> may cause dark urine with fatigue, jaundice, and back or abdominal pain. <strong>History and physical examination</strong> In addition to the standard general medical history and physical examination, the following sections include the most common items that should be included in the evaluation of a patient with dark urine. <strong>Closing the encounter</strong> In the wrap-up discussion, the first step is to discuss the likely diagnosis along with an assessment of the diagnostic uncertainty. If a patient has pathognomonic findings for a particular disease, you should explain the significance of them. If you are uncertain about the diagnosis, say so clearly, but reassure the patient that you will work with them to identify the cause. Regarding diagnostic tests, if invasive studies are necessary (eg, cystoscopy in an elderly smoker with hematuria), explain the rationale for the tests. Allow time for questions, and assess the patient's readiness to undergo the studies you recommend. <strong>Diagnostic studies</strong> Patients with an abnormal urine color should have a urinalysis with microscopic analysis of urinary sediment (ie, for casts, crystals, etc.). Note that patients with myoglobinuria may have a positive test for hemoglobin on chemical (dip stick) urinalysis without red blood cells on microscopic analysis. Other studies may include: Electrolytes, blood urea nitrogen, creatinine Liver function tests (eg, direct and indirect bilirubin) Urine culture Complete blood count (and peripheral smear, reticulocyte count) Muscle enzymes (eg, creatinine kinase, aspartate aminotransferase [AST]) CT urogram (for identifying kidney stones) Liver/biliary CT scan, ultrasound Cystoscopy Patients with hematuria should have evaluation of both the upper and lower urinary tract. Typical studies include CT urogram and cystoscopy, but the specific evaluation may be individualized. If hemolytic anemia is suspected, start with a complete blood count, reticulocyte count, and peripheral smear. Supportive findings include elevated lactate dehydrogenase, low haptoglobin, and elevated unconjugated bilirubin. These should be performed before more specific testing (eg, hemoglobin electrophoresis, glucose-6-phosphate dehydrogenase, osmotic fragility).](https://d2lvgg3v3hfg70.cloudfront.net/MD0004/11ec25d3_0de4_ac66_bf52_d3a705875c47_MD0004_00.jpg) Closing the encounter
Closing the encounter
In the wrap-up discussion, the first step is to discuss the likely diagnosis along with an assessment of the diagnostic uncertainty. If a patient has pathognomonic findings for a particular disease, you should explain the significance of them. If you are uncertain about the diagnosis, say so clearly, but reassure the patient that you will work with them to identify the cause.
Regarding diagnostic tests, if invasive studies are necessary (eg, cystoscopy in an elderly smoker with hematuria), explain the rationale for the tests. Allow time for questions, and assess the patient's readiness to undergo the studies you recommend.
Diagnostic studies
Patients with an abnormal urine color should have a urinalysis with microscopic analysis of urinary sediment (ie, for casts, crystals, etc.). Note that patients with myoglobinuria may have a positive test for hemoglobin on chemical ("dip stick") urinalysis without red blood cells on microscopic analysis. Other studies may include:
Electrolytes, blood urea nitrogen, creatinine
Liver function tests (eg, direct and indirect bilirubin)
Urine culture
Complete blood count (and peripheral smear, reticulocyte count)
Muscle enzymes (eg, creatinine kinase, aspartate aminotransferase [AST])
CT urogram (for identifying kidney stones)
Liver/biliary CT scan, ultrasound
Cystoscopy
Patients with hematuria should have evaluation of both the upper and lower urinary tract. Typical studies include CT urogram and cystoscopy, but the specific evaluation may be individualized.
If hemolytic anemia is suspected, start with a complete blood count, reticulocyte count, and peripheral smear. Supportive findings include elevated lactate dehydrogenase, low haptoglobin, and elevated unconjugated bilirubin. These should be performed before more specific testing (eg, hemoglobin electrophoresis, glucose-6-phosphate dehydrogenase, osmotic fragility).
Patients may report unusual or undifferentiated symptoms that could be due to disease in multiple systems. In some cases, this may represent a cardinal manifestation of an uncommon condition (eg, the "target shaped" rash of Lyme disease). Alternately, unusual symptoms may be an atypical manifestation of a common disorder (eg, systemic lupus erythematosus presenting as migratory mononeuropathy).
When evaluating a patient with nonspecific symptoms, review the medical history, risk factors, and medications to identify what disorders and complications are most likely. Identify the system involved, and consider what disorders are most likely to affect that system in the patient.
Dark urine can represent either an unusually concentrated urine, hematuria, or an abnormal pigment in the urine. Abnormal urine color is usually due to disorders of the renourinary tract, hepatobiliary system, blood/hematologic system, or musculoskeletal system. If the patient otherwise feels well, abnormal urine color is usually benign.
Differential diagnosis
The color of the urine can guide the differential diagnosis:
Red: Blood, food pigments (eg, beets, rhubarb), medications (eg, phenazopyridine, rifampin), porphyrins
Blue/green: Food dyes, medications (eg, indomethacin, amitriptyline), Pseudomonas urinary tract infection
Brown: Medications (eg, metronidazole, senna), liver/kidney disease, myoglobin/rhabdomyolysis
Orange: Hepatobiliary disease, dehydration
Hematuria can be categorized by the pattern through urination. Blood at the start of voiding that clears is usually from a urethral source. Blood at the end of voiding suggests a bladder or prostate source. Visible blood throughout voiding may represent an upper tract (kidney and collecting system) source.
Biliary obstruction may cause dark-yellow/orange urine with jaundice, pale stools, and right upper quandrant pain. Hematuria in a patient with a history of heavy smoking is a common presentation of bladder cancer. Dark urine following a crush injury or extreme physical exertion suggests rhabdomyolysis. In addition, hemolysis may cause dark urine with fatigue, jaundice, and back or abdominal pain.
History and physical examination
In addition to the standard general medical history and physical examination, the following sections include the most common items that should be included in the evaluation of a patient with dark urine.
![<strong>Approach to the patient</strong> Patients may report unusual or undifferentiated symptoms that could be due to disease in multiple systems. In some cases, this may represent a <strong>cardinal manifestation</strong> of an uncommon condition (eg, the target shaped rash of Lyme disease). Alternately, unusual symptoms may be an <strong>atypical manifestation</strong> of a common disorder (eg, systemic lupus erythematosus presenting as migratory mononeuropathy). When evaluating a patient with nonspecific symptoms, review the medical history, risk factors, and medications to identify what disorders and complications are most likely. Identify the system involved, and consider what disorders are most likely to affect that system in the patient. Dark urine can represent either an unusually concentrated urine, hematuria, or an <strong>abnormal pigment</strong> in the urine. Abnormal urine color is usually due to disorders of the renourinary tract, hepatobiliary system, blood/hematologic system, or musculoskeletal system. If the patient otherwise feels well, abnormal urine color is usually benign. <strong>Differential diagnosis</strong> The color of the urine can guide the differential diagnosis: <strong>Red</strong>: Blood, food pigments (eg, beets, rhubarb), medications (eg, phenazopyridine, rifampin), porphyrins <strong>Blue/green</strong>: Food dyes, medications (eg, indomethacin, amitriptyline), Pseudomonas urinary tract infection <strong>Brown</strong>: Medications (eg, metronidazole, senna), liver/kidney disease, myoglobin/rhabdomyolysis <strong>Orange</strong>: Hepatobiliary disease, dehydration <strong>Hematuria</strong> can be categorized by the pattern through urination. Blood at the start of voiding that clears is usually from a urethral source. Blood at the end of voiding suggests a bladder or prostate source. Visible blood throughout voiding may represent an upper tract (kidney and collecting system) source. <strong>Biliary obstruction</strong> may cause dark-yellow/orange urine with jaundice, pale stools, and right upper quandrant pain. Hematuria in a patient with a history of heavy smoking is a common presentation of <strong>bladder cancer</strong>. Dark urine following a crush injury or extreme physical exertion suggests <strong>rhabdomyolysis</strong>. In addition,<strong> hemolysis</strong> may cause dark urine with fatigue, jaundice, and back or abdominal pain. <strong>History and physical examination</strong> In addition to the standard general medical history and physical examination, the following sections include the most common items that should be included in the evaluation of a patient with dark urine. <strong>Closing the encounter</strong> In the wrap-up discussion, the first step is to discuss the likely diagnosis along with an assessment of the diagnostic uncertainty. If a patient has pathognomonic findings for a particular disease, you should explain the significance of them. If you are uncertain about the diagnosis, say so clearly, but reassure the patient that you will work with them to identify the cause. Regarding diagnostic tests, if invasive studies are necessary (eg, cystoscopy in an elderly smoker with hematuria), explain the rationale for the tests. Allow time for questions, and assess the patient's readiness to undergo the studies you recommend. <strong>Diagnostic studies</strong> Patients with an abnormal urine color should have a urinalysis with microscopic analysis of urinary sediment (ie, for casts, crystals, etc.). Note that patients with myoglobinuria may have a positive test for hemoglobin on chemical (dip stick) urinalysis without red blood cells on microscopic analysis. Other studies may include: Electrolytes, blood urea nitrogen, creatinine Liver function tests (eg, direct and indirect bilirubin) Urine culture Complete blood count (and peripheral smear, reticulocyte count) Muscle enzymes (eg, creatinine kinase, aspartate aminotransferase [AST]) CT urogram (for identifying kidney stones) Liver/biliary CT scan, ultrasound Cystoscopy Patients with hematuria should have evaluation of both the upper and lower urinary tract. Typical studies include CT urogram and cystoscopy, but the specific evaluation may be individualized. If hemolytic anemia is suspected, start with a complete blood count, reticulocyte count, and peripheral smear. Supportive findings include elevated lactate dehydrogenase, low haptoglobin, and elevated unconjugated bilirubin. These should be performed before more specific testing (eg, hemoglobin electrophoresis, glucose-6-phosphate dehydrogenase, osmotic fragility).](https://d2lvgg3v3hfg70.cloudfront.net/MD0004/11ec25d3_0de4_8555_bf52_57665ff6ea7e_MD0004_00.jpg)
![<strong>Approach to the patient</strong> Patients may report unusual or undifferentiated symptoms that could be due to disease in multiple systems. In some cases, this may represent a <strong>cardinal manifestation</strong> of an uncommon condition (eg, the target shaped rash of Lyme disease). Alternately, unusual symptoms may be an <strong>atypical manifestation</strong> of a common disorder (eg, systemic lupus erythematosus presenting as migratory mononeuropathy). When evaluating a patient with nonspecific symptoms, review the medical history, risk factors, and medications to identify what disorders and complications are most likely. Identify the system involved, and consider what disorders are most likely to affect that system in the patient. Dark urine can represent either an unusually concentrated urine, hematuria, or an <strong>abnormal pigment</strong> in the urine. Abnormal urine color is usually due to disorders of the renourinary tract, hepatobiliary system, blood/hematologic system, or musculoskeletal system. If the patient otherwise feels well, abnormal urine color is usually benign. <strong>Differential diagnosis</strong> The color of the urine can guide the differential diagnosis: <strong>Red</strong>: Blood, food pigments (eg, beets, rhubarb), medications (eg, phenazopyridine, rifampin), porphyrins <strong>Blue/green</strong>: Food dyes, medications (eg, indomethacin, amitriptyline), Pseudomonas urinary tract infection <strong>Brown</strong>: Medications (eg, metronidazole, senna), liver/kidney disease, myoglobin/rhabdomyolysis <strong>Orange</strong>: Hepatobiliary disease, dehydration <strong>Hematuria</strong> can be categorized by the pattern through urination. Blood at the start of voiding that clears is usually from a urethral source. Blood at the end of voiding suggests a bladder or prostate source. Visible blood throughout voiding may represent an upper tract (kidney and collecting system) source. <strong>Biliary obstruction</strong> may cause dark-yellow/orange urine with jaundice, pale stools, and right upper quandrant pain. Hematuria in a patient with a history of heavy smoking is a common presentation of <strong>bladder cancer</strong>. Dark urine following a crush injury or extreme physical exertion suggests <strong>rhabdomyolysis</strong>. In addition,<strong> hemolysis</strong> may cause dark urine with fatigue, jaundice, and back or abdominal pain. <strong>History and physical examination</strong> In addition to the standard general medical history and physical examination, the following sections include the most common items that should be included in the evaluation of a patient with dark urine. <strong>Closing the encounter</strong> In the wrap-up discussion, the first step is to discuss the likely diagnosis along with an assessment of the diagnostic uncertainty. If a patient has pathognomonic findings for a particular disease, you should explain the significance of them. If you are uncertain about the diagnosis, say so clearly, but reassure the patient that you will work with them to identify the cause. Regarding diagnostic tests, if invasive studies are necessary (eg, cystoscopy in an elderly smoker with hematuria), explain the rationale for the tests. Allow time for questions, and assess the patient's readiness to undergo the studies you recommend. <strong>Diagnostic studies</strong> Patients with an abnormal urine color should have a urinalysis with microscopic analysis of urinary sediment (ie, for casts, crystals, etc.). Note that patients with myoglobinuria may have a positive test for hemoglobin on chemical (dip stick) urinalysis without red blood cells on microscopic analysis. Other studies may include: Electrolytes, blood urea nitrogen, creatinine Liver function tests (eg, direct and indirect bilirubin) Urine culture Complete blood count (and peripheral smear, reticulocyte count) Muscle enzymes (eg, creatinine kinase, aspartate aminotransferase [AST]) CT urogram (for identifying kidney stones) Liver/biliary CT scan, ultrasound Cystoscopy Patients with hematuria should have evaluation of both the upper and lower urinary tract. Typical studies include CT urogram and cystoscopy, but the specific evaluation may be individualized. If hemolytic anemia is suspected, start with a complete blood count, reticulocyte count, and peripheral smear. Supportive findings include elevated lactate dehydrogenase, low haptoglobin, and elevated unconjugated bilirubin. These should be performed before more specific testing (eg, hemoglobin electrophoresis, glucose-6-phosphate dehydrogenase, osmotic fragility).](https://d2lvgg3v3hfg70.cloudfront.net/MD0004/11ec25d3_0de4_ac66_bf52_d3a705875c47_MD0004_00.jpg) Closing the encounter
Closing the encounterIn the wrap-up discussion, the first step is to discuss the likely diagnosis along with an assessment of the diagnostic uncertainty. If a patient has pathognomonic findings for a particular disease, you should explain the significance of them. If you are uncertain about the diagnosis, say so clearly, but reassure the patient that you will work with them to identify the cause.
Regarding diagnostic tests, if invasive studies are necessary (eg, cystoscopy in an elderly smoker with hematuria), explain the rationale for the tests. Allow time for questions, and assess the patient's readiness to undergo the studies you recommend.
Diagnostic studies
Patients with an abnormal urine color should have a urinalysis with microscopic analysis of urinary sediment (ie, for casts, crystals, etc.). Note that patients with myoglobinuria may have a positive test for hemoglobin on chemical ("dip stick") urinalysis without red blood cells on microscopic analysis. Other studies may include:
Electrolytes, blood urea nitrogen, creatinine
Liver function tests (eg, direct and indirect bilirubin)
Urine culture
Complete blood count (and peripheral smear, reticulocyte count)
Muscle enzymes (eg, creatinine kinase, aspartate aminotransferase [AST])
CT urogram (for identifying kidney stones)
Liver/biliary CT scan, ultrasound
Cystoscopy
Patients with hematuria should have evaluation of both the upper and lower urinary tract. Typical studies include CT urogram and cystoscopy, but the specific evaluation may be individualized.
If hemolytic anemia is suspected, start with a complete blood count, reticulocyte count, and peripheral smear. Supportive findings include elevated lactate dehydrogenase, low haptoglobin, and elevated unconjugated bilirubin. These should be performed before more specific testing (eg, hemoglobin electrophoresis, glucose-6-phosphate dehydrogenase, osmotic fragility).
3
Doorway information about patient
The patient is a 40-year-old woman who comes to the clinic due to headaches.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 120/70 mm Hg
Pulse: 80/min
Respiratory rate: 19/min
The patient is a 40-year-old woman who comes to the clinic due to headaches.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 120/70 mm Hg
Pulse: 80/min
Respiratory rate: 19/min
Approach to the patient
Most primary headache syndromes (eg, migraine, tension-type headache) usually present at a young age, and often become less severe with age. Onset (or significant change) at age >40 justifies greater concern. Clinical features suggesting a potentially serious cause of headache are summarized by the mnemonic "SNOOP":
Systemic symptoms (eg, weight loss, fever) or disease (eg, cancer, HIV/AIDS)
Neurologic symptoms (eg, focal deficits, altered sensorium)
Sudden Onset
Older age at first occurrence
Change from Previous headache
Headaches are usually diagnosed based on historical features. Examination is normal in most patients, and is primarily focused on ruling out uncommon diagnoses.
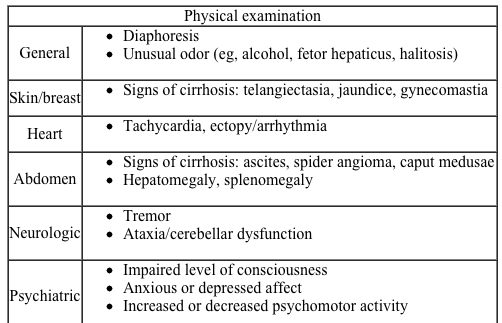
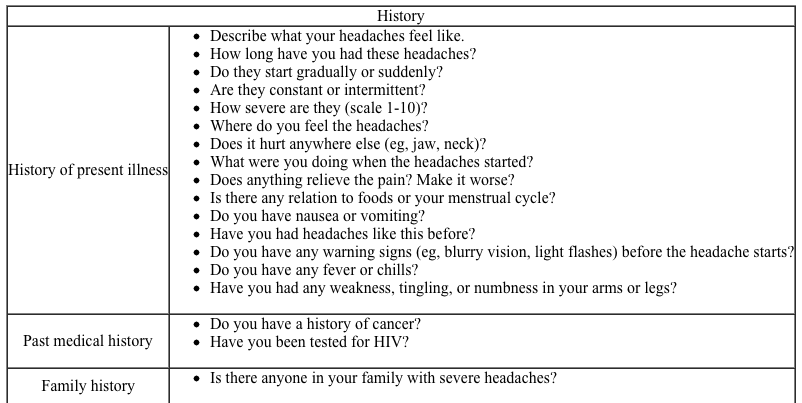
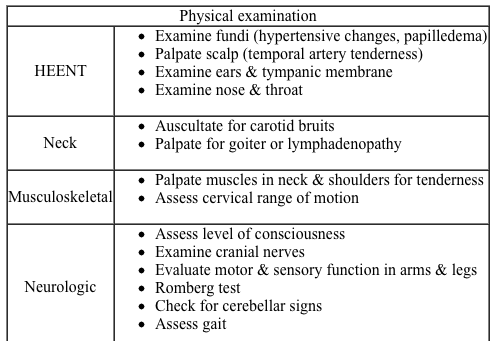
Differential diagnosis
 Tension-type headache is the most common headache syndrome. It begins slowly over several hours and may last for days if not treated. Characteristic features include a bilateral squeezing or pressure sensation, particularly at the temporal or occipital area. Associated symptoms (eg, nausea, visual changes) are rare.
Tension-type headache is the most common headache syndrome. It begins slowly over several hours and may last for days if not treated. Characteristic features include a bilateral squeezing or pressure sensation, particularly at the temporal or occipital area. Associated symptoms (eg, nausea, visual changes) are rare.
True migraine headaches are usually unilateral, have a throbbing quality, and may be associated with nausea and visual disturbances. Migraines generally have a rapid onset and recognizable triggers such as caffeine, foods/beverages (eg, chocolate, red wine), or menstruation. Migraines can be categorized as without aura (common migraine) or with aura (classic migraine). An aura is a transient neurologic (usually visual) symptom at the beginning of the headache. A history of "flashing lights" or "wavy lines" in the visual fields followed by a throbbing unilateral headache is virtually pathognomonic for migraine. Atypical migraines are common, and many nonstandard headache types (eg, sinus headache) actually represent migraine variants.
Secondary headaches are less common than primary headache syndromes but usually more ominous. Major syndromes include:
Intracranial neoplasm: Morning or nocturnal headaches, worsened by bending over, neurologic deficits, or seizures
Subarachnoid hemorrhage: Severe and sudden onset ("worst headache of my life"), vomiting, loss of consciousness, neck stiffness
Angle closure glaucoma: Periorbital pain, vomiting, visual symptoms, abnormal ocular examination
Bacterial meningitis: Fever, confusion, nuchal rigidity
Giant cell arteritis: Age >50, temporal location, jaw claudication, shoulder or hip pain
Hypertensive encephalopathy: Rapid rise in blood pressure (>180/120 mm Hg)
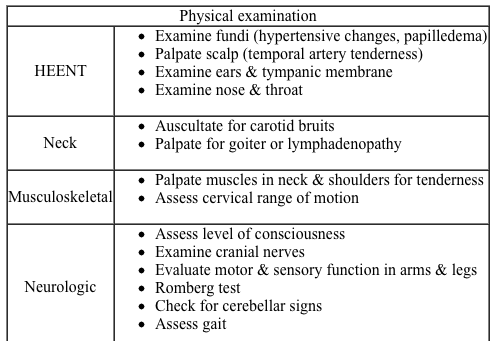
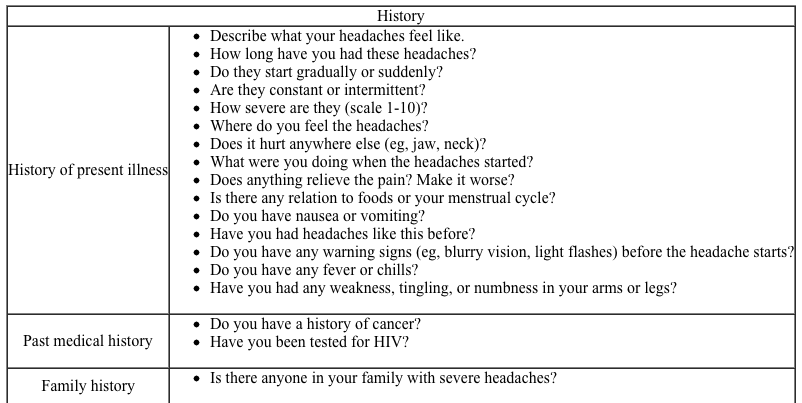
History and physical examination
In addition to the standard general medical history and physical examination, the following sections include the most common items that should be included in the evaluation of headaches.
 Closing the encounter
Closing the encounter
Older patients or patients with atypical symptoms may need additional diagnostic testing. In such cases, explain the possible causes and the goals of the tests. Give the patient an accurate assessment of the diagnostic uncertainty (eg, "Your symptoms suggest benign migraines, but it is unusual for someone your age to have headaches for the first time. I would like to do additional testing to be sure."). Explain that there are no tests to confirm migraine or tension-type headaches, but tests are done to rule out other disorders.
Diagnostic studies
Young patients with a classic headache history may not need any diagnostic tests. If no tests are needed to confirm the diagnosis, write, "No studies indicated" in the Diagnostic Studies section.
Patients with focal neurologic symptoms (other than a stereotypical aura) or any of the "SNOOP" criteria should be considered for neuroimaging. Patients with suspected subarachnoid hemorrhage or signs of elevated intracranial pressure usually undergo an urgent CT scan. For less urgent indications, MRI has greater sensitivity.
Lumbar puncture (LP) may be considered in the evaluation of atypical or potentially serious headache syndromes. LP can confirm subarachnoid hemorrhage, but CT is done first. Other indications for LP include bacterial meningitis and idiopathic intracranial hypertension (pseudotumor cerebri).
Patients with possible giant cell arteritis should have erythrocyte sedimentation rate or C-reactive protein tests. Patients with fever or other systemic symptoms should have a complete blood count. Patients with severe hypertension should have an ECG and renal function studies (blood urea nitrogen, creatinine, urinalysis).
Most primary headache syndromes (eg, migraine, tension-type headache) usually present at a young age, and often become less severe with age. Onset (or significant change) at age >40 justifies greater concern. Clinical features suggesting a potentially serious cause of headache are summarized by the mnemonic "SNOOP":
Systemic symptoms (eg, weight loss, fever) or disease (eg, cancer, HIV/AIDS)
Neurologic symptoms (eg, focal deficits, altered sensorium)
Sudden Onset
Older age at first occurrence
Change from Previous headache
Headaches are usually diagnosed based on historical features. Examination is normal in most patients, and is primarily focused on ruling out uncommon diagnoses.
Differential diagnosis
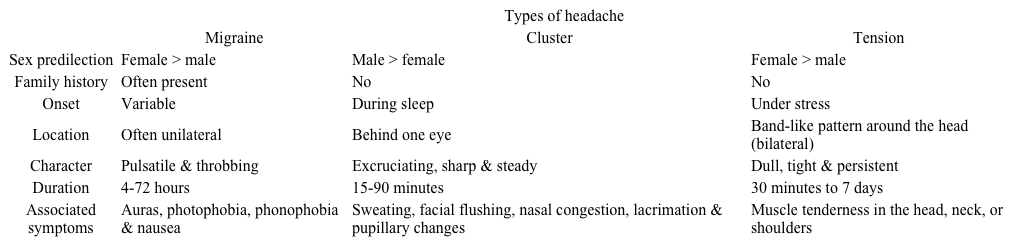 Tension-type headache is the most common headache syndrome. It begins slowly over several hours and may last for days if not treated. Characteristic features include a bilateral squeezing or pressure sensation, particularly at the temporal or occipital area. Associated symptoms (eg, nausea, visual changes) are rare.
Tension-type headache is the most common headache syndrome. It begins slowly over several hours and may last for days if not treated. Characteristic features include a bilateral squeezing or pressure sensation, particularly at the temporal or occipital area. Associated symptoms (eg, nausea, visual changes) are rare.True migraine headaches are usually unilateral, have a throbbing quality, and may be associated with nausea and visual disturbances. Migraines generally have a rapid onset and recognizable triggers such as caffeine, foods/beverages (eg, chocolate, red wine), or menstruation. Migraines can be categorized as without aura (common migraine) or with aura (classic migraine). An aura is a transient neurologic (usually visual) symptom at the beginning of the headache. A history of "flashing lights" or "wavy lines" in the visual fields followed by a throbbing unilateral headache is virtually pathognomonic for migraine. Atypical migraines are common, and many nonstandard headache types (eg, sinus headache) actually represent migraine variants.
Secondary headaches are less common than primary headache syndromes but usually more ominous. Major syndromes include:
Intracranial neoplasm: Morning or nocturnal headaches, worsened by bending over, neurologic deficits, or seizures
Subarachnoid hemorrhage: Severe and sudden onset ("worst headache of my life"), vomiting, loss of consciousness, neck stiffness
Angle closure glaucoma: Periorbital pain, vomiting, visual symptoms, abnormal ocular examination
Bacterial meningitis: Fever, confusion, nuchal rigidity
Giant cell arteritis: Age >50, temporal location, jaw claudication, shoulder or hip pain
Hypertensive encephalopathy: Rapid rise in blood pressure (>180/120 mm Hg)
History and physical examination
In addition to the standard general medical history and physical examination, the following sections include the most common items that should be included in the evaluation of headaches.
 Closing the encounter
Closing the encounterOlder patients or patients with atypical symptoms may need additional diagnostic testing. In such cases, explain the possible causes and the goals of the tests. Give the patient an accurate assessment of the diagnostic uncertainty (eg, "Your symptoms suggest benign migraines, but it is unusual for someone your age to have headaches for the first time. I would like to do additional testing to be sure."). Explain that there are no tests to confirm migraine or tension-type headaches, but tests are done to rule out other disorders.
Diagnostic studies
Young patients with a classic headache history may not need any diagnostic tests. If no tests are needed to confirm the diagnosis, write, "No studies indicated" in the Diagnostic Studies section.
Patients with focal neurologic symptoms (other than a stereotypical aura) or any of the "SNOOP" criteria should be considered for neuroimaging. Patients with suspected subarachnoid hemorrhage or signs of elevated intracranial pressure usually undergo an urgent CT scan. For less urgent indications, MRI has greater sensitivity.
Lumbar puncture (LP) may be considered in the evaluation of atypical or potentially serious headache syndromes. LP can confirm subarachnoid hemorrhage, but CT is done first. Other indications for LP include bacterial meningitis and idiopathic intracranial hypertension (pseudotumor cerebri).
Patients with possible giant cell arteritis should have erythrocyte sedimentation rate or C-reactive protein tests. Patients with fever or other systemic symptoms should have a complete blood count. Patients with severe hypertension should have an ECG and renal function studies (blood urea nitrogen, creatinine, urinalysis).
4
Doorway information about patient
The patient is a 52-year-old woman who comes to the clinic due to hot flashes.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 130/80 mm Hg
Heart rate: 80/min
Respirations: 12/min
The patient is a 52-year-old woman who comes to the clinic due to hot flashes.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 130/80 mm Hg
Heart rate: 80/min
Respirations: 12/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
5
Doorway information about patient
The patient is a 50-year-old man who comes to the clinic for a refill of his diabetes medications.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 135/70 mm Hg
Pulse: 73/min
Respirations: 16/min
The patient is a 50-year-old man who comes to the clinic for a refill of his diabetes medications.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 135/70 mm Hg
Pulse: 73/min
Respirations: 16/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
6
Doorway information about patient
The patient is a 22-year-old man who comes to the clinic due to night sweats.
Vital signs
Temperature: 36.9 C (98.4 F)
Blood pressure: 115/80 mm Hg
Pulse: 68/min
Respirations: 12/min
The patient is a 22-year-old man who comes to the clinic due to night sweats.
Vital signs
Temperature: 36.9 C (98.4 F)
Blood pressure: 115/80 mm Hg
Pulse: 68/min
Respirations: 12/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
7
Doorway information about patient
The patient is a 60-year-old woman who comes to the clinic due to 2 months of back pain.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 122/80 mm Hg
Pulse: 90/min
Respirations: 14/min
The patient is a 60-year-old woman who comes to the clinic due to 2 months of back pain.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 122/80 mm Hg
Pulse: 90/min
Respirations: 14/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
8
Doorway information about patient
The patient is a 65-year-old man who is brought to the clinic by his wife for 2-3 months of confusion.
Vital signs
Temperature: 36.7 C (98.0 F)
Blood pressure: 132/84 mm Hg
Pulse: 80/min
Respiratory rate: 14/min
The patient is a 65-year-old man who is brought to the clinic by his wife for 2-3 months of confusion.
Vital signs
Temperature: 36.7 C (98.0 F)
Blood pressure: 132/84 mm Hg
Pulse: 80/min
Respiratory rate: 14/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
9
Doorway information about patient
The patient is a 70-year-old woman who comes to the clinic due to episodes of forgetfulness.
Vital signs
Temperature: 36.1 C (97.0 F)
Blood pressure: 150/85 mm Hg
Pulse: 76/min
Respiratory rate: 16/min
The patient is a 70-year-old woman who comes to the clinic due to episodes of forgetfulness.
Vital signs
Temperature: 36.1 C (97.0 F)
Blood pressure: 150/85 mm Hg
Pulse: 76/min
Respiratory rate: 16/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
10
Doorway information about patient
The patient is a 65-year-old man who comes to the clinic with 1 day of episodic chest pain.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 122/80 mm Hg
Pulse: 90/min
Respiratory rate: 14/min
The patient is a 65-year-old man who comes to the clinic with 1 day of episodic chest pain.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 122/80 mm Hg
Pulse: 90/min
Respiratory rate: 14/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
11
Doorway information about patient
The patient is a 45-year-old man who comes to the clinic with a cough and blood in his sputum.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 120/70 mm Hg
Heart rate: 80/min
Respiratory rate: 12/min
The patient is a 45-year-old man who comes to the clinic with a cough and blood in his sputum.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 120/70 mm Hg
Heart rate: 80/min
Respiratory rate: 12/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
12
Doorway information about patient
The patient is a 40-year-old woman who comes to the clinic stating that she feels "down."
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 122/80 mm Hg
Pulse: 90/min
Respiratory rate: 14/min
The patient is a 40-year-old woman who comes to the clinic stating that she feels "down."
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 122/80 mm Hg
Pulse: 90/min
Respiratory rate: 14/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
13
Doorway information about patient
The patient is a 35-year-old man who comes to the clinic due to episodes of coughing for 3 months.
Vital signs
Temperature: 36.7 C (98.0 F)
Blood pressure: 122/80 mm Hg
Pulse: 90/min
Respirations: 14/min
The patient is a 35-year-old man who comes to the clinic due to episodes of coughing for 3 months.
Vital signs
Temperature: 36.7 C (98.0 F)
Blood pressure: 122/80 mm Hg
Pulse: 90/min
Respirations: 14/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
14
Doorway information about patient
The patient is a 65-year-old woman who comes to the clinic for episodes of dizziness.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 122/80 mm Hg
Pulse: 90/min
Respirations: 14/min
The patient is a 65-year-old woman who comes to the clinic for episodes of dizziness.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 122/80 mm Hg
Pulse: 90/min
Respirations: 14/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
15
Doorway information about patient
The patient is a 45-year-old woman who comes to the clinic due
to bruises on her arms and face after a fall.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 122/80 mm Hg
Heart rate: 90/min
Respirations: 14/min
The patient is a 45-year-old woman who comes to the clinic due
to bruises on her arms and face after a fall.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 122/80 mm Hg
Heart rate: 90/min
Respirations: 14/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
16
Doorway information about patient
The patient is a 41-year-old woman who comes to the clinic with hand pain.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 126/80 mm Hg
Heart rate: 72/min
Respirations: 12/min
The patient is a 41-year-old woman who comes to the clinic with hand pain.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 126/80 mm Hg
Heart rate: 72/min
Respirations: 12/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
17
Doorway information about patient
The patient is a 45-year-old man who comes to the clinic with insomnia.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 120/70 mm Hg
Pulse: 80/min
Respiratory rate: 14/min
The patient is a 45-year-old man who comes to the clinic with insomnia.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 120/70 mm Hg
Pulse: 80/min
Respiratory rate: 14/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
18
Doorway information about patient
The patient is a 34-year-old man who comes to the clinic due to 4 weeks of diarrhea.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 118/78 mm Hg
Pulse: 86/min
Respirations: 14/min
The patient is a 34-year-old man who comes to the clinic due to 4 weeks of diarrhea.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 118/78 mm Hg
Pulse: 86/min
Respirations: 14/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
19
Doorway information about patient
The patient is a 35-year-old man who comes to the clinic due to 1 week of left heel pain.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 120/70 mm Hg
Pulse: 80/min
Respirations: 12/min
The patient is a 35-year-old man who comes to the clinic due to 1 week of left heel pain.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 120/70 mm Hg
Pulse: 80/min
Respirations: 12/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
20
Doorway information about patient
You will be speaking with the mother of a 5-year-old boy who wets his bed frequently.
You will be speaking with the mother of a 5-year-old boy who wets his bed frequently.

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
21
Doorway information about patient
The patient is a 55-year-old woman who comes to the clinic for counseling on smoking cessation.
Vital signs
Temperature: 36.7 C (98.0 F)
Blood pressure: 122/80 mm Hg
Pulse: 70/min
Respirations: 14/min
The patient is a 55-year-old woman who comes to the clinic for counseling on smoking cessation.
Vital signs
Temperature: 36.7 C (98.0 F)
Blood pressure: 122/80 mm Hg
Pulse: 70/min
Respirations: 14/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
22
Doorway information about patient
The patient is a 25-year-old man who comes to the clinic for a pre-employment evaluation.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 117/80 mm Hg
Pulse: 64/min
Respirations: 12/min
The patient is a 25-year-old man who comes to the clinic for a pre-employment evaluation.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 117/80 mm Hg
Pulse: 64/min
Respirations: 12/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
23
Doorway information about patient
The patient is a 56-year-old man who comes to the clinic due to shoulder pain.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 130/80 mm Hg
Pulse: 80/min
Respirations: 12/min
The patient is a 56-year-old man who comes to the clinic due to shoulder pain.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 130/80 mm Hg
Pulse: 80/min
Respirations: 12/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
24
Doorway information about patient
The patient is a 22-year-old woman who comes to the clinic for follow-up of asthma.
Vital signs
Temperature: 36.8 C (98.2 F)
Blood pressure: 118/68 mm Hg
Pulse: 84/min
Respirations: 16/min
The patient is a 22-year-old woman who comes to the clinic for follow-up of asthma.
Vital signs
Temperature: 36.8 C (98.2 F)
Blood pressure: 118/68 mm Hg
Pulse: 84/min
Respirations: 16/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
25
Doorway information about patient
The patient is a 69-year-old man with terminal lung cancer who comes to the clinic requesting pain medication.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 130/80 mm Hg
Pulse: 80/min
Respirations: 12/min
The patient is a 69-year-old man with terminal lung cancer who comes to the clinic requesting pain medication.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 130/80 mm Hg
Pulse: 80/min
Respirations: 12/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
26
Doorway information about patient
The patient is a 5-year-old boy who has been vomiting for a day. His mother has left a phone message with the clinic. You will talk with the patient's mother on the phone.
The patient is a 5-year-old boy who has been vomiting for a day. His mother has left a phone message with the clinic. You will talk with the patient's mother on the phone.

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
27
Doorway information about patient
The patient is a 40-year-old woman who comes to the clinic due to weight gain.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 150/90 mm Hg
Pulse: 68/min
Respirations: 16/min
The patient is a 40-year-old woman who comes to the clinic due to weight gain.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 150/90 mm Hg
Pulse: 68/min
Respirations: 16/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
28
Doorway information about patient
The patient is a 28-year-old man who comes to the clinic due to palpitations.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 130/80 mm Hg
Pulse: 80/min
Respirations: 12/min
The patient is a 28-year-old man who comes to the clinic due to palpitations.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 130/80 mm Hg
Pulse: 80/min
Respirations: 12/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
29
Doorway information about patient
The patient is a 20-year-old woman who reports abnormal vaginal bleeding.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 110/70 mm Hg
Pulse: 80/min
Respirations: 16/min
The patient is a 20-year-old woman who reports abnormal vaginal bleeding.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 110/70 mm Hg
Pulse: 80/min
Respirations: 16/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
30
Doorway information about patient
The patient is a 25-year-old woman who comes to the clinic due to vomiting.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 110/70 mm Hg
Pulse: 80/min
Respirations: 14/min
The patient is a 25-year-old woman who comes to the clinic due to vomiting.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 110/70 mm Hg
Pulse: 80/min
Respirations: 14/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck
31
Doorway information about patient
The patient is a 55-year-old man who comes to the clinic due to passing out.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 130/80 mm Hg
Pulse: 80/min
Respirations: 12/min
The patient is a 55-year-old man who comes to the clinic due to passing out.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 130/80 mm Hg
Pulse: 80/min
Respirations: 12/min

Unlock Deck
Unlock for access to all 31 flashcards in this deck.
Unlock Deck
k this deck



