Deck 2: STEP 2 CS - Practice Cases
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question

Unlock Deck
Sign up to unlock the cards in this deck!
Unlock Deck
Unlock Deck
1/43
Play
Full screen (f)
Deck 2: STEP 2 CS - Practice Cases
1
Doorway information about patient
The patient is a 50-year-old man who comes to the office due to bilateral leg pain.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 140/80 mm Hg
Pulse: 78/min
Respirations: 20/min
Basic differential diagnosis
Bilateral pain
Atherosclerotic vascular disease
Lumbar spinal stenosis
Diabetic polyneuropathy
Radiculopathy due to spinal disease
Medications, such as statins
Trauma
Thromboangiitis obliterans
Unilateral pain
Cellulitis/myofasciitis
Deep vein thrombosis
Rupture of Baker cyst
Osteomyelitis
Radiculopathy/sciatica
Pathological fracture of the bone
The patient is a 50-year-old man who comes to the office due to bilateral leg pain.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 140/80 mm Hg
Pulse: 78/min
Respirations: 20/min
Basic differential diagnosis
Bilateral pain
Atherosclerotic vascular disease
Lumbar spinal stenosis
Diabetic polyneuropathy
Radiculopathy due to spinal disease
Medications, such as statins
Trauma
Thromboangiitis obliterans
Unilateral pain
Cellulitis/myofasciitis
Deep vein thrombosis
Rupture of Baker cyst
Osteomyelitis
Radiculopathy/sciatica
Pathological fracture of the bone
Instructions:
If the doctor asks you about anything other than these, just say "no," or provide an answer that a normal patient might give.
You are a 50-year-old man with bilateral leg pain.
History of present illness
Onset 2 months ago
Pain started gradually and has become progressively worse
Throbbing pain with 5-6/10 severity
Located in the calf muscles, no radiation
Worse with walking, running, and prolonged standing
Better while sitting and at rest
No history of trauma
Review of systems
No fever
No back pain
No weakness, numbness, or tingling in the legs
No sexual or bladder symptoms
Past medical/family/social history
Diabetes for the past 3 years, controlled by diet
High cholesterol
No surgeries
Medications: Simvastatin 40 mg daily at bedtime
Allergies: No
Father died at age 65 of a stroke; mother and 2 siblings are healthy
Occupation: Postal worker
Married, live with wife
Tobacco: 2 packs a day for past 30 years
Alcohol: Occasional beer
Recreational drugs: No
Physical examination
Abdomen:
No bruits
Extremities:
Pulses 2+ and symmetrical in bilateral lower extremities
Musculoskeletal:
Negative Homans sign
No calf tenderness to palpation bilaterally
Neurologic:
Motor strength 5/6 in both lower extremities
Grossly intact sensation
Deep tendon reflexes 2+ symmetrically
Checklist:
Following the encounter, check which of the following items were performed by the examinee.
History of present illness/review of systems
Asked about the location and radiation of pain
Asked about the onset of pain
Asked about whether it is continuous or intermittent pain
Asked about the intensity of pain
Asked about the quality of pain
Asked about the course of pain over time
Asked about any aggravating or relieving factors
Asked about rest pain
Asked about swelling of the legs
Asked about sensory changes (such as numbness) and paresthesia
Asked about any weakness of the legs
Asked about any history of back pain
Asked about fever
Asked about trauma to the legs
Asked about other joint pain
Asked about recent surgeries or prolonged immobilization
Asked about impotence
Past medical/family/social history
Asked about similar episodes in the past
Asked about past medical issues (especially high blood pressure, diabetes, high cholesterol, disc prolapse)
Asked about current medications
Asked about medication allergies
Asked about family health (especially history of blood clots)
Asked about tobacco, alcohol, and recreational drug use
Asked about occupation
Examination
Washed hands before examination
Examined without gown, not through the gown
Examined calf tenderness
Elicited Homans sign
Checked pulses in both legs and arms
Listened for bruit at the distal aorta, iliac, or femoral arteries
Checked sensation in both legs
Checked reflexes in both legs
Checked for vibration sense in both legs
Counseling
Explained physical findings and possible diagnosis
Explained further workup
Discussed lifestyle modifications, including quitting smoking
Communication skills and professional conduct
Knocked before entering the room
Introduced self and greeted you warmly
Used your name to address you
Paid attention to what you said and maintained good eye contact
Asked open-ended questions
Asked nonleading questions
Asked one question at a time
Listened to what you said without interrupting
Used plain English rather than technical jargon
Used appropriate transition sentences
Used appropriate draping techniques
Expressed empathy and gave appropriate reassurances
Asked whether you had any concerns/questions
Differential diagnosis
Thromboangiitis obliterans
Atherosclerotic vascular disease
Drug induced (statins)
Diabetic polyneuropathy
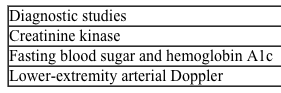
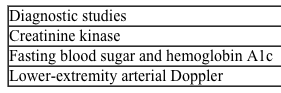
Diagnostic study/studies
Creatinine kinase
Blood sugar and hemoglobin A1c
Lipid profile
Arterial doppler study of the lower extremities
Duplex venous ultrasound of lower limbs
CBC with differential
Spine MRI
Case 20 Patient Notes
The following represents a typical note for this patient encounter. The details may vary depending on the information given by the simulated patient.
History: Describe the history you just obtained from this patient. Include only information (pertinent positives and negatives) relevant to this patient's problem(s).
50-yo man with 2 months of worsening bilateral leg pain.
Throbbing pain mainly over the calf muscles made worse with walking, running, and prolonged standing.
Symptom improvement with rest and sitting.
ROS: No pain at rest, fever, trauma, swelling, back pain, weakness, sexual difficulties, numbness, or tingling in legs
PMHx: Diabetes for 3 years under diet control, hypercholesterolemia
PSHx: None
Meds: Simvastatin 40 mg daily at bedtime
Allergies: None
FHx: Father died at age 65 of stroke; mother and 2 siblings are healthy
SHx: 2 PPD smoker for past 30 years, occasional alcohol use
Physical examination: Describe any positive and negative findings relevant to this patient's problem(s). Be careful to include only those parts of examination performed in this encounter.
Vital signs: Temperature, 36.7 C (98.1 F); blood pressure, 140/80 mm Hg; pulse, 78/min; and respirations, 20/min
Abdomen: No bruits
Extremities: Pulses 2+ and symmetrical in bilateral lower extremities
Musculoskeletal: Negative Homans sign, no calf tenderness to palpation bilaterally
Neurologic: Bilateral lower extremities with 5/5 motor strength, intact vibratory sensation and proprioception, and DTR 2+
Data interpretation: Based on what you have learned from the history and physical examination, list up to 3 diagnoses that might explain this patient's complaint(s). List your diagnoses from most to least likely. For some cases, fewer than 3 diagnoses will be appropriate. Then enter the positive or negative findings from the history and the physical examination (if present) that support each diagnosis. Lastly, list initial diagnostic studies (if any) you would order for each listed diagnosis (eg, restricted physical examination maneuvers, laboratory tests, imaging, ECG).
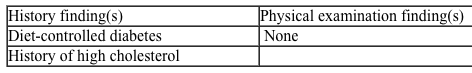
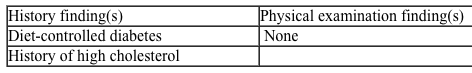
Diagnosis #1: Drug-induced (statin) myopathy
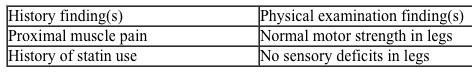
Diagnosis #2: Atherosclerotic peripheral vascular disease
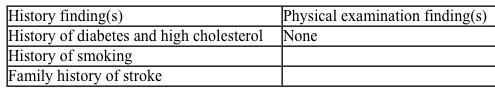
Diagnosis #3: Diabetic polyneuropathy
If the doctor asks you about anything other than these, just say "no," or provide an answer that a normal patient might give.
You are a 50-year-old man with bilateral leg pain.
History of present illness
Onset 2 months ago
Pain started gradually and has become progressively worse
Throbbing pain with 5-6/10 severity
Located in the calf muscles, no radiation
Worse with walking, running, and prolonged standing
Better while sitting and at rest
No history of trauma
Review of systems
No fever
No back pain
No weakness, numbness, or tingling in the legs
No sexual or bladder symptoms
Past medical/family/social history
Diabetes for the past 3 years, controlled by diet
High cholesterol
No surgeries
Medications: Simvastatin 40 mg daily at bedtime
Allergies: No
Father died at age 65 of a stroke; mother and 2 siblings are healthy
Occupation: Postal worker
Married, live with wife
Tobacco: 2 packs a day for past 30 years
Alcohol: Occasional beer
Recreational drugs: No
Physical examination
Abdomen:
No bruits
Extremities:
Pulses 2+ and symmetrical in bilateral lower extremities
Musculoskeletal:
Negative Homans sign
No calf tenderness to palpation bilaterally
Neurologic:
Motor strength 5/6 in both lower extremities
Grossly intact sensation
Deep tendon reflexes 2+ symmetrically
Checklist:
Following the encounter, check which of the following items were performed by the examinee.
History of present illness/review of systems
Asked about the location and radiation of pain
Asked about the onset of pain
Asked about whether it is continuous or intermittent pain
Asked about the intensity of pain
Asked about the quality of pain
Asked about the course of pain over time
Asked about any aggravating or relieving factors
Asked about rest pain
Asked about swelling of the legs
Asked about sensory changes (such as numbness) and paresthesia
Asked about any weakness of the legs
Asked about any history of back pain
Asked about fever
Asked about trauma to the legs
Asked about other joint pain
Asked about recent surgeries or prolonged immobilization
Asked about impotence
Past medical/family/social history
Asked about similar episodes in the past
Asked about past medical issues (especially high blood pressure, diabetes, high cholesterol, disc prolapse)
Asked about current medications
Asked about medication allergies
Asked about family health (especially history of blood clots)
Asked about tobacco, alcohol, and recreational drug use
Asked about occupation
Examination
Washed hands before examination
Examined without gown, not through the gown
Examined calf tenderness
Elicited Homans sign
Checked pulses in both legs and arms
Listened for bruit at the distal aorta, iliac, or femoral arteries
Checked sensation in both legs
Checked reflexes in both legs
Checked for vibration sense in both legs
Counseling
Explained physical findings and possible diagnosis
Explained further workup
Discussed lifestyle modifications, including quitting smoking
Communication skills and professional conduct
Knocked before entering the room
Introduced self and greeted you warmly
Used your name to address you
Paid attention to what you said and maintained good eye contact
Asked open-ended questions
Asked nonleading questions
Asked one question at a time
Listened to what you said without interrupting
Used plain English rather than technical jargon
Used appropriate transition sentences
Used appropriate draping techniques
Expressed empathy and gave appropriate reassurances
Asked whether you had any concerns/questions
Differential diagnosis
Thromboangiitis obliterans
Atherosclerotic vascular disease
Drug induced (statins)
Diabetic polyneuropathy
Diagnostic study/studies
Creatinine kinase
Blood sugar and hemoglobin A1c
Lipid profile
Arterial doppler study of the lower extremities
Duplex venous ultrasound of lower limbs
CBC with differential
Spine MRI
Case 20 Patient Notes
The following represents a typical note for this patient encounter. The details may vary depending on the information given by the simulated patient.
History: Describe the history you just obtained from this patient. Include only information (pertinent positives and negatives) relevant to this patient's problem(s).
50-yo man with 2 months of worsening bilateral leg pain.
Throbbing pain mainly over the calf muscles made worse with walking, running, and prolonged standing.
Symptom improvement with rest and sitting.
ROS: No pain at rest, fever, trauma, swelling, back pain, weakness, sexual difficulties, numbness, or tingling in legs
PMHx: Diabetes for 3 years under diet control, hypercholesterolemia
PSHx: None
Meds: Simvastatin 40 mg daily at bedtime
Allergies: None
FHx: Father died at age 65 of stroke; mother and 2 siblings are healthy
SHx: 2 PPD smoker for past 30 years, occasional alcohol use
Physical examination: Describe any positive and negative findings relevant to this patient's problem(s). Be careful to include only those parts of examination performed in this encounter.
Vital signs: Temperature, 36.7 C (98.1 F); blood pressure, 140/80 mm Hg; pulse, 78/min; and respirations, 20/min
Abdomen: No bruits
Extremities: Pulses 2+ and symmetrical in bilateral lower extremities
Musculoskeletal: Negative Homans sign, no calf tenderness to palpation bilaterally
Neurologic: Bilateral lower extremities with 5/5 motor strength, intact vibratory sensation and proprioception, and DTR 2+
Data interpretation: Based on what you have learned from the history and physical examination, list up to 3 diagnoses that might explain this patient's complaint(s). List your diagnoses from most to least likely. For some cases, fewer than 3 diagnoses will be appropriate. Then enter the positive or negative findings from the history and the physical examination (if present) that support each diagnosis. Lastly, list initial diagnostic studies (if any) you would order for each listed diagnosis (eg, restricted physical examination maneuvers, laboratory tests, imaging, ECG).
Diagnosis #1: Drug-induced (statin) myopathy
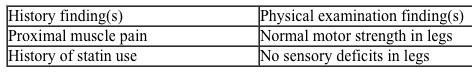
Diagnosis #2: Atherosclerotic peripheral vascular disease
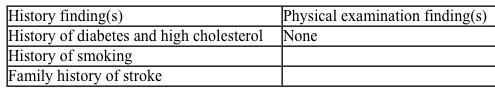
Diagnosis #3: Diabetic polyneuropathy
2
Doorway information about patient
The patient is a 35-year-old man who comes to the office due to acute diarrhea.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 110/65 mm Hg
Pulse: 100/min
Respirations: 18/min
Basic differential diagnosis
Viral gastroenteritis
Bacterial gastroenteritis & food-borne pathogens
Medication induced
Giardiasis
Clostridium difficle colitis
Inflammatory bowel disease
Irritable bowel disease
Malabsorption
HIV
The patient is a 35-year-old man who comes to the office due to acute diarrhea.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 110/65 mm Hg
Pulse: 100/min
Respirations: 18/min
Basic differential diagnosis
Viral gastroenteritis
Bacterial gastroenteritis & food-borne pathogens
Medication induced
Giardiasis
Clostridium difficle colitis
Inflammatory bowel disease
Irritable bowel disease
Malabsorption
HIV
Instructions:
If the doctor asks you about anything other than these, just say "no," or provide an answer that a normal patient might give.
You are a 35-year-old man who has diarrhea.
History of present illness
Onset 1 day ago, 6-8 hours after meal
Ate salad and shrimp at a local seafood restaurant
Loose, watery stools with no blood or mucus
6 or 7 bowel movements in 24 hours
Associated symptoms: Diffuse abdominal cramps
Nausea and vomiting
Difficulty keeping down solids or liquids
No fever or chills
Nothing seems to make it worse, and you have not tried any over-the-counter treatments
2 friends who ate with you have similar symptoms
No recent travel
Review of systems
Sinus infection 2 weeks ago, treated with amoxicillin (last dose 2 days ago)
No chest pain or shortness of breath
No urinary symptoms
No back pain
Past medical/family/social history
No significant past medical problems or surgeries
No other medications (other than amoxicillin)
No medication allergies
Both parents and siblings (2 brothers) are healthy
Single, live alone
Occupation: Software engineer
Smoking: No
Alcohol: No
Recreational drugs: No
Physical examination
Head and neck:
No erythema or exudates in the mouth/pharynx
Dry mucous membranes
No enlarged lymph nodes
Skin:
No jaundice
Chest/lungs:
Clear to auscultation bilaterally
Heart:
Regular rhythm without murmurs, gallops, or rubs
Abdomen:
Nontender, nondistended
Normoactive bowel sounds throughout
Tympanic to percussion
No hepatosplenomegaly
Checklist:
Following the encounter, check which of the following items were performed by the examinee.
History of present illness/review of systems
Asked to clarify characteristics of diarrhea: Increased frequency? Increased volume? Altered consistency?
Asked about the onset and duration of diarrhea
Asked about the frequency of diarrhea
Asked about associated symptoms (eg, vomiting, fever, abdominal pain, anorexia, prior constipation, myalgia, tenesmus)
Asked about any blood or mucus in stools
Asked about any recent travel
Asked whether any other family members or other contacts are sick
Asked about exposure to suspicious foods (eg, unpasteurized/undercooked food, unusual foods, dairy products, seafood)
Past medical/family/social history
Asked about prior episodes of diarrhea and gastrointestinal illness
Asked about other medical issues
Asked about medications (especially antibiotics) and medication allergies
Asked about recent and previous hospitalizations
Asked about any abdominal surgeries
Asked about occupation
Asked about tobacco, alcohol, and drug use
Asked about family history (especially gastrointestinal diseases)
Examination
Examinee washed hands
Examined without gown, not through gown
Auscultated abdomen
Palpated abdomen superficially
Palpated abdomen deeply
Examination of skin for any rashes
Examination of oral cavity
Respiratory examination
Cardiac auscultation
Counseling
Explained the physical findings and possible diagnosis
Explained further workup
Discussed need for rectal examination
Discussed fluids and other basic interventions
Communication skills and professional conduct
Knocked before entering the room
Introduced self and greeted you warmly
Used your name to address you
Paid attention to what you said and maintained good eye contact
Asked open-ended questions
Asked nonleading questions
Asked one question at a time
Listened to what you said without interrupting
Used plain English rather than technical jargon
Used appropriate transition sentences
Used appropriate draping techniques
Summarized the history and explained physical findings
Expressed empathy and gave appropriate reassurances
Asked whether you have any concerns/questions
Differential diagnosis
Viral gastroenteritis
Bacterial gastroenteritis
Clostridium difficile diarrhea
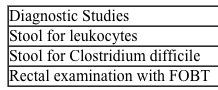
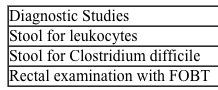
Diagnostic study/studies
Rectal examination
Fecal occult blood test
CBC with differential count
Basic metabolic panel (electrolytes, BUN, creatinine, glucose)
Stool for C difficile toxin
Stool for fecal leukocytes
Case 7 Patient Note
The following represents a typical note for this patient encounter. The details may vary depending on the information given by the simulated patient.
History: Describe the history you just obtained from this patient. Include only information (pertinent positives and negatives) relevant to this patient's problem(s).
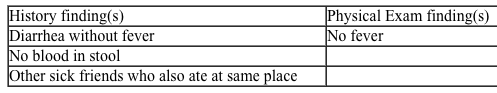
35-yo male with 1 day of diarrhea with 6-7 loose BM/day without blood or mucus.
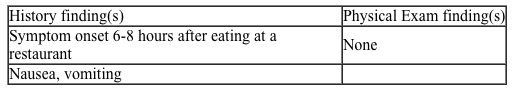
Ate seafood and salad at a restaurant 6-8 hours before symptom onset.
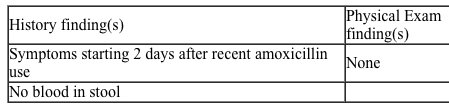
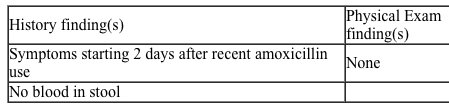
Recent sinus infection treated with amoxicillin, last dose 2 days ago.
Diffuse crampy abdominal pain, nausea, vomiting, decreased PO intake.
Two other friends who ate at the restaurant have the same symptoms.
ROS: No fever, chills, chest pain, shortness of breath, burning with urination, recent travel, or back pain
PMHx: None
PSHx: None
Meds: None
Allergies: None
FHx: Noncontributory
SHx: Denies tobacco and alcohol use
Physical examination: Describe any positive and negative findings relevant to this patient's problem(s). Be careful to include only those parts of the examination performed in this encounter.
Vital signs: Temperature, 36.7 C (98 F); blood pressure, 110/65 mm Hg; pulse,100/min; and respirations, 18/min
Head/neck: Oropharynx with dry mucous membranes but no erythema or exudates, no enlarged lymph nodes, no jaundice
Chest/lungs: Clear to auscultation bilaterally
Heart: RRR without M/G/R
Abdomen: Nontender, nondistended, normoactive bowel sounds throughout; tympanic on percussion; no hepatosplenomegaly
Data interpretation: Based on what you have learned from the history and physical examination, list up to 3 diagnoses that might explain this patient's complaint(s). List your diagnoses from most to least likely. For some cases, fewer than 3 diagnoses will be appropriate. Then, enter the positive or negative findings from the history and the physical examination (if present) that support each diagnosis. Lastly, list initial diagnostic studies (if any) you would order for each listed diagnosis (e.g., restricted physical exam maneuvers, laboratory tests, imaging, ECG, etc.).
Diagnosis #1: Viral gastroenteritis
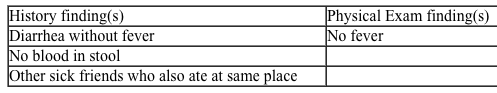
Diagnosis #2: Bacterial gastroenteritis
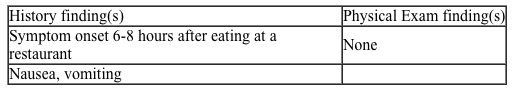
Diagnosis #3: Clostridium difficile colitis
If the doctor asks you about anything other than these, just say "no," or provide an answer that a normal patient might give.
You are a 35-year-old man who has diarrhea.
History of present illness
Onset 1 day ago, 6-8 hours after meal
Ate salad and shrimp at a local seafood restaurant
Loose, watery stools with no blood or mucus
6 or 7 bowel movements in 24 hours
Associated symptoms: Diffuse abdominal cramps
Nausea and vomiting
Difficulty keeping down solids or liquids
No fever or chills
Nothing seems to make it worse, and you have not tried any over-the-counter treatments
2 friends who ate with you have similar symptoms
No recent travel
Review of systems
Sinus infection 2 weeks ago, treated with amoxicillin (last dose 2 days ago)
No chest pain or shortness of breath
No urinary symptoms
No back pain
Past medical/family/social history
No significant past medical problems or surgeries
No other medications (other than amoxicillin)
No medication allergies
Both parents and siblings (2 brothers) are healthy
Single, live alone
Occupation: Software engineer
Smoking: No
Alcohol: No
Recreational drugs: No
Physical examination
Head and neck:
No erythema or exudates in the mouth/pharynx
Dry mucous membranes
No enlarged lymph nodes
Skin:
No jaundice
Chest/lungs:
Clear to auscultation bilaterally
Heart:
Regular rhythm without murmurs, gallops, or rubs
Abdomen:
Nontender, nondistended
Normoactive bowel sounds throughout
Tympanic to percussion
No hepatosplenomegaly
Checklist:
Following the encounter, check which of the following items were performed by the examinee.
History of present illness/review of systems
Asked to clarify characteristics of diarrhea: Increased frequency? Increased volume? Altered consistency?
Asked about the onset and duration of diarrhea
Asked about the frequency of diarrhea
Asked about associated symptoms (eg, vomiting, fever, abdominal pain, anorexia, prior constipation, myalgia, tenesmus)
Asked about any blood or mucus in stools
Asked about any recent travel
Asked whether any other family members or other contacts are sick
Asked about exposure to suspicious foods (eg, unpasteurized/undercooked food, unusual foods, dairy products, seafood)
Past medical/family/social history
Asked about prior episodes of diarrhea and gastrointestinal illness
Asked about other medical issues
Asked about medications (especially antibiotics) and medication allergies
Asked about recent and previous hospitalizations
Asked about any abdominal surgeries
Asked about occupation
Asked about tobacco, alcohol, and drug use
Asked about family history (especially gastrointestinal diseases)
Examination
Examinee washed hands
Examined without gown, not through gown
Auscultated abdomen
Palpated abdomen superficially
Palpated abdomen deeply
Examination of skin for any rashes
Examination of oral cavity
Respiratory examination
Cardiac auscultation
Counseling
Explained the physical findings and possible diagnosis
Explained further workup
Discussed need for rectal examination
Discussed fluids and other basic interventions
Communication skills and professional conduct
Knocked before entering the room
Introduced self and greeted you warmly
Used your name to address you
Paid attention to what you said and maintained good eye contact
Asked open-ended questions
Asked nonleading questions
Asked one question at a time
Listened to what you said without interrupting
Used plain English rather than technical jargon
Used appropriate transition sentences
Used appropriate draping techniques
Summarized the history and explained physical findings
Expressed empathy and gave appropriate reassurances
Asked whether you have any concerns/questions
Differential diagnosis
Viral gastroenteritis
Bacterial gastroenteritis
Clostridium difficile diarrhea
Diagnostic study/studies
Rectal examination
Fecal occult blood test
CBC with differential count
Basic metabolic panel (electrolytes, BUN, creatinine, glucose)
Stool for C difficile toxin
Stool for fecal leukocytes
Case 7 Patient Note
The following represents a typical note for this patient encounter. The details may vary depending on the information given by the simulated patient.
History: Describe the history you just obtained from this patient. Include only information (pertinent positives and negatives) relevant to this patient's problem(s).
35-yo male with 1 day of diarrhea with 6-7 loose BM/day without blood or mucus.
Ate seafood and salad at a restaurant 6-8 hours before symptom onset.
Recent sinus infection treated with amoxicillin, last dose 2 days ago.
Diffuse crampy abdominal pain, nausea, vomiting, decreased PO intake.
Two other friends who ate at the restaurant have the same symptoms.
ROS: No fever, chills, chest pain, shortness of breath, burning with urination, recent travel, or back pain
PMHx: None
PSHx: None
Meds: None
Allergies: None
FHx: Noncontributory
SHx: Denies tobacco and alcohol use
Physical examination: Describe any positive and negative findings relevant to this patient's problem(s). Be careful to include only those parts of the examination performed in this encounter.
Vital signs: Temperature, 36.7 C (98 F); blood pressure, 110/65 mm Hg; pulse,100/min; and respirations, 18/min
Head/neck: Oropharynx with dry mucous membranes but no erythema or exudates, no enlarged lymph nodes, no jaundice
Chest/lungs: Clear to auscultation bilaterally
Heart: RRR without M/G/R
Abdomen: Nontender, nondistended, normoactive bowel sounds throughout; tympanic on percussion; no hepatosplenomegaly
Data interpretation: Based on what you have learned from the history and physical examination, list up to 3 diagnoses that might explain this patient's complaint(s). List your diagnoses from most to least likely. For some cases, fewer than 3 diagnoses will be appropriate. Then, enter the positive or negative findings from the history and the physical examination (if present) that support each diagnosis. Lastly, list initial diagnostic studies (if any) you would order for each listed diagnosis (e.g., restricted physical exam maneuvers, laboratory tests, imaging, ECG, etc.).
Diagnosis #1: Viral gastroenteritis
Diagnosis #2: Bacterial gastroenteritis
Diagnosis #3: Clostridium difficile colitis
3
Doorway information about patient
The patient is a 40-year-old woman who comes to the office due to increased urination.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 110/70 mm Hg
Pulse: 86/min
Respirations: 16/min
Basic differential diagnosis
Increased urine volume
Diabetes mellitus
Diabetes insipidus (central, nephrogenic)
Psychogenic polydypsia
Diuretic use
Hypercalcemia
Increased urinary frequency
Urinary tract infection
Overactive bladder
Excess caffeine intake
Vaginitis, urethritis
The patient is a 40-year-old woman who comes to the office due to increased urination.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 110/70 mm Hg
Pulse: 86/min
Respirations: 16/min
Basic differential diagnosis
Increased urine volume
Diabetes mellitus
Diabetes insipidus (central, nephrogenic)
Psychogenic polydypsia
Diuretic use
Hypercalcemia
Increased urinary frequency
Urinary tract infection
Overactive bladder
Excess caffeine intake
Vaginitis, urethritis
Instructions:
If the doctor asks you about anything other than these, just say "no," or provide an answer that a normal patient might give.
You are a 40-year-old woman complaining of increased urinary frequency.
History of present illness
Onset 2 months ago
Urinating 8-10 times during the day and 2-3 times a night
Increased urinary volume
Increased feeling of thirst for last month
Associated symptoms: Fatigue
4.5-kg (10-lb) weight loss (despite increased appetite)
No dysuria or urgency
No fever or chills
Past medical/family/social history
Bipolar disorder diagnosed 20 years ago
Minor head injury after falling off bicycle 3 months ago; seen in emergency department and discharged without intervention
No surgeries or hospitalizations
Medications: Lithium 60 mg twice daily
Medication allergies: None
Married, live with husband
2 pregnancies with normal vaginal delivery; both children are healthy
Both parents have type 2 diabetes mellitus; no siblings
Tobacco: No
Alcohol: No
Recreational drugs: No
Physical examination
HEENT:
PERRLA, EOMI
Visual fields intact
Heart:
Regular rate and rhythm
No murmurs, gallops, or rubs
Abdomen:
Soft and nontender with normal bowel sounds
No suprapubic or CVA tenderness
Neurologic:
Muscle strength 5/5 throughout
Sensation in tact in all 4 extremities
Reflexes 2+ in all 4 extremities
Checklist:
Following the encounter, check which of the following items were performed by the examinee.
History of present illness/review of systems
Asked about the onset of problem
Asked about the frequency of urination
Asked about nocturia
Asked about urine volume
Asked about burning on urination
Asked about urgency and hesitancy of urination
Asked about increased thirst and fluid intake
Asked about appetite and changes in weight
Asked about the trauma to the head
Past medical/family/social history
Asked about similar problems in the past
Asked about past medical issues, hospitalizations, and surgeries
Asked about psychiatric problems (history of bipolar disorder, schizophrenia)
Asked about current medications
Asked about medication allergies
Asked about family health (especially diabetes)
Asked about tobacco, alcohol, and drug use
Asked about occupation
Examination
Washed hands before examination
Examined without gown, not through gown
Examined mucous membranes
Examined heart and lungs
Tested muscle power in both upper and lower limbs
Tested sensation in the lower extremities
Tested reflexes in the lower extremities
Tested visual fields and examined fundus
Tested for suprapubic and costovertebral angle tenderness
Counseling
Explained physical findings and possible diagnosis
Explained further workup
Communication skills and professional conduct
Knocked before entering the room
Introduced self and greeted you warmly
Used your name to address you
Paid attention to what you said and maintained good eye contact
Asked open-ended questions
Asked nonleading questions
Asked one question at a time
Listened to what you said without interrupting
Used plain English rather than technical jargon
Used appropriate transition sentences
Used appropriate draping techniques
Expressed empathy and gave appropriate reassurances
Asked whether you had any concerns/questions
Differential diagnosis
Diabetes mellitus
Central diabetes insipidus
Nephrogenic diabetes insipidus (lithium side effect)
Psychogenic polydypsia
Hypercalcemia
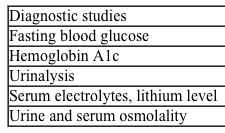
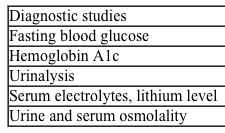
Diagnostic study/studies
Fasting blood sugar
Urinalysis
Serum electrolytes (Na, K, Cl, Co2, BUN, Cr, and calcium)
Urine and serum osmolality
Case 16 Patient Notes
The following represents a typical note for this patient encounter. The details may vary depending on the information given by the simulated patient.
History: Describe the history you just obtained from this patient. Include only information (pertinent positives and negatives) relevant to this patient's problem(s).
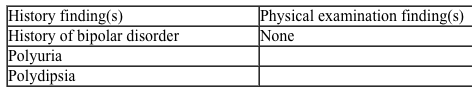
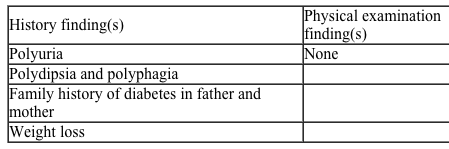
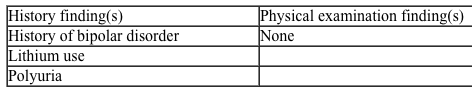
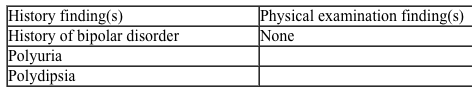
40-yo woman with 2 months of polyuria, polydipsia, nocturia, and polyphagia.
2-3 months of 4.5-kg (10-lb) weight loss with fatigue.
No dysuria or urinary urgency.
ROS: No fever or chills
PMHx: Bipolar disorder diagnosed 20 years ago; minor head trauma 3 months ago, seen in emergency department and discharged without intervention
PSHx: None
Meds: Lithium 600 mg 2 times daily
Allergies: None
FHx: Father and mother have diabetes
SHx: No history of tobacco or alcohol use
Physical examination: Describe any positive and negative findings relevant to this patient's problem(s). Be careful to include only those parts of the examination performed in this encounter.
Vital signs: Temperature, 36.7 C (98.1 F); blood pressure, 110/70 mm Hg; pulse, 86/min; and respirations,16/min
HEENT: PERRLA, EOMI, intact visual fields
Heart: RRR without murmurs, gallops, or rubs
Abdomen: Nontender without suprapubic tenderness, no CVA tenderness
Neurologic: Muscle strength 5/5 throughout, sensation grossly intact in bilateral lower extremities, DTR 2+ in bilateral lower extremities
Data interpretation: Based on what you have learned from the history and physical examination, list up to 3 diagnoses that might explain this patient's complaint(s). List your diagnoses from most to least likely. For some cases, fewer than 3 diagnoses will be appropriate. Then, enter the positive or negative findings from the history and the physical examination (if present) that support each diagnosis. Lastly, list initial diagnostic studies (if any) you would order for each listed diagnosis (eg, restricted physical examination maneuvers, laboratory tests, imaging, ECG).
Diagnosis #1: Diabetes mellitus
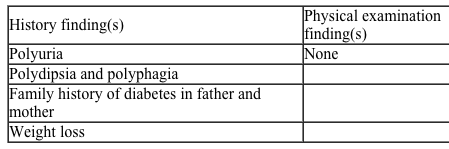
Diagnosis #2: Diabetes insipidus
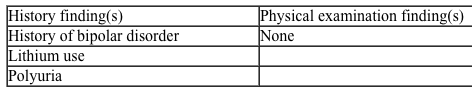
Diagnosis #3: Psychogenic polydipsia
If the doctor asks you about anything other than these, just say "no," or provide an answer that a normal patient might give.
You are a 40-year-old woman complaining of increased urinary frequency.
History of present illness
Onset 2 months ago
Urinating 8-10 times during the day and 2-3 times a night
Increased urinary volume
Increased feeling of thirst for last month
Associated symptoms: Fatigue
4.5-kg (10-lb) weight loss (despite increased appetite)
No dysuria or urgency
No fever or chills
Past medical/family/social history
Bipolar disorder diagnosed 20 years ago
Minor head injury after falling off bicycle 3 months ago; seen in emergency department and discharged without intervention
No surgeries or hospitalizations
Medications: Lithium 60 mg twice daily
Medication allergies: None
Married, live with husband
2 pregnancies with normal vaginal delivery; both children are healthy
Both parents have type 2 diabetes mellitus; no siblings
Tobacco: No
Alcohol: No
Recreational drugs: No
Physical examination
HEENT:
PERRLA, EOMI
Visual fields intact
Heart:
Regular rate and rhythm
No murmurs, gallops, or rubs
Abdomen:
Soft and nontender with normal bowel sounds
No suprapubic or CVA tenderness
Neurologic:
Muscle strength 5/5 throughout
Sensation in tact in all 4 extremities
Reflexes 2+ in all 4 extremities
Checklist:
Following the encounter, check which of the following items were performed by the examinee.
History of present illness/review of systems
Asked about the onset of problem
Asked about the frequency of urination
Asked about nocturia
Asked about urine volume
Asked about burning on urination
Asked about urgency and hesitancy of urination
Asked about increased thirst and fluid intake
Asked about appetite and changes in weight
Asked about the trauma to the head
Past medical/family/social history
Asked about similar problems in the past
Asked about past medical issues, hospitalizations, and surgeries
Asked about psychiatric problems (history of bipolar disorder, schizophrenia)
Asked about current medications
Asked about medication allergies
Asked about family health (especially diabetes)
Asked about tobacco, alcohol, and drug use
Asked about occupation
Examination
Washed hands before examination
Examined without gown, not through gown
Examined mucous membranes
Examined heart and lungs
Tested muscle power in both upper and lower limbs
Tested sensation in the lower extremities
Tested reflexes in the lower extremities
Tested visual fields and examined fundus
Tested for suprapubic and costovertebral angle tenderness
Counseling
Explained physical findings and possible diagnosis
Explained further workup
Communication skills and professional conduct
Knocked before entering the room
Introduced self and greeted you warmly
Used your name to address you
Paid attention to what you said and maintained good eye contact
Asked open-ended questions
Asked nonleading questions
Asked one question at a time
Listened to what you said without interrupting
Used plain English rather than technical jargon
Used appropriate transition sentences
Used appropriate draping techniques
Expressed empathy and gave appropriate reassurances
Asked whether you had any concerns/questions
Differential diagnosis
Diabetes mellitus
Central diabetes insipidus
Nephrogenic diabetes insipidus (lithium side effect)
Psychogenic polydypsia
Hypercalcemia
Diagnostic study/studies
Fasting blood sugar
Urinalysis
Serum electrolytes (Na, K, Cl, Co2, BUN, Cr, and calcium)
Urine and serum osmolality
Case 16 Patient Notes
The following represents a typical note for this patient encounter. The details may vary depending on the information given by the simulated patient.
History: Describe the history you just obtained from this patient. Include only information (pertinent positives and negatives) relevant to this patient's problem(s).
40-yo woman with 2 months of polyuria, polydipsia, nocturia, and polyphagia.
2-3 months of 4.5-kg (10-lb) weight loss with fatigue.
No dysuria or urinary urgency.
ROS: No fever or chills
PMHx: Bipolar disorder diagnosed 20 years ago; minor head trauma 3 months ago, seen in emergency department and discharged without intervention
PSHx: None
Meds: Lithium 600 mg 2 times daily
Allergies: None
FHx: Father and mother have diabetes
SHx: No history of tobacco or alcohol use
Physical examination: Describe any positive and negative findings relevant to this patient's problem(s). Be careful to include only those parts of the examination performed in this encounter.
Vital signs: Temperature, 36.7 C (98.1 F); blood pressure, 110/70 mm Hg; pulse, 86/min; and respirations,16/min
HEENT: PERRLA, EOMI, intact visual fields
Heart: RRR without murmurs, gallops, or rubs
Abdomen: Nontender without suprapubic tenderness, no CVA tenderness
Neurologic: Muscle strength 5/5 throughout, sensation grossly intact in bilateral lower extremities, DTR 2+ in bilateral lower extremities
Data interpretation: Based on what you have learned from the history and physical examination, list up to 3 diagnoses that might explain this patient's complaint(s). List your diagnoses from most to least likely. For some cases, fewer than 3 diagnoses will be appropriate. Then, enter the positive or negative findings from the history and the physical examination (if present) that support each diagnosis. Lastly, list initial diagnostic studies (if any) you would order for each listed diagnosis (eg, restricted physical examination maneuvers, laboratory tests, imaging, ECG).
Diagnosis #1: Diabetes mellitus
Diagnosis #2: Diabetes insipidus
Diagnosis #3: Psychogenic polydipsia
4
Doorway information about patient
The patient is a 35-year-old man who comes to the office due to a cough.
Vital signs
Temperature: 38.5 C (101.3 F)
Blood pressure: 120/75 mm Hg
Pulse: 98/min
Respirations: 20/min
Basic differential diagnosis
Common cold
Acute sinusitis
Allergic rhinitis
Acute bronchitis
Pneumonia
Pertussis
Pulmonary embolism
Drugs (ACE inhibitors)
Asthma
Congestive heart failure
Chronic obstructive pulmonary disease (COPD) exacerbation
The patient is a 35-year-old man who comes to the office due to a cough.
Vital signs
Temperature: 38.5 C (101.3 F)
Blood pressure: 120/75 mm Hg
Pulse: 98/min
Respirations: 20/min
Basic differential diagnosis
Common cold
Acute sinusitis
Allergic rhinitis
Acute bronchitis
Pneumonia
Pertussis
Pulmonary embolism
Drugs (ACE inhibitors)
Asthma
Congestive heart failure
Chronic obstructive pulmonary disease (COPD) exacerbation

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
5
Doorway information about patient
The patient is a 24-year-old woman who comes to the office for an initial prenatal visit.
Vital signs
Temperature: 37.1 C (98.8 F)
Blood pressure: 120/75 mm Hg
Pulse: 78/min
Respirations: 20/min
The patient is a 24-year-old woman who comes to the office for an initial prenatal visit.
Vital signs
Temperature: 37.1 C (98.8 F)
Blood pressure: 120/75 mm Hg
Pulse: 78/min
Respirations: 20/min

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
6
Doorway information about patient
The patient is a 45-year-old man who comes to the emergency department due to right lower abdominal pain.
Vital signs
Temperature: 37.1 C (98.7 F)
Blood pressure: 130/80 mm Hg
Pulse: 100/min
Respirations: 20/min
Basic differential diagnosis
Appendicitis
Meckel diverticulitis
Perforated viscus
Intestinal obstruction
Yersinia enterocolitica
Pancreatitis
Urolithiasis
Acute cholecystitis
Herpes zoster (shingles)
The patient is a 45-year-old man who comes to the emergency department due to right lower abdominal pain.
Vital signs
Temperature: 37.1 C (98.7 F)
Blood pressure: 130/80 mm Hg
Pulse: 100/min
Respirations: 20/min
Basic differential diagnosis
Appendicitis
Meckel diverticulitis
Perforated viscus
Intestinal obstruction
Yersinia enterocolitica
Pancreatitis
Urolithiasis
Acute cholecystitis
Herpes zoster (shingles)

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
7
Doorway information about patient
The patient is a 65-year-old woman who comes to the emergency department due to arm and leg weakness.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 160/90 mm Hg
Pulse: 78/min
Respirations: 22/min
Basic differential diagnosis
Neurologic
Stroke
Transient ischemic attack (TIA)
Subarachnoid hemorrhage
Subdural hematoma
Intracranial mass
Guillain-Barré syndrome
Spinal cord lesion
Complex migraine
Metabolic
Hypoglycemia
Hypothyroidism
Adrenal insufficiency
Electrolyte disorders
Musculoskeletal
Myopathy
Miscellaneous
Conversion disorder
Heat-related illness
The patient is a 65-year-old woman who comes to the emergency department due to arm and leg weakness.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 160/90 mm Hg
Pulse: 78/min
Respirations: 22/min
Basic differential diagnosis
Neurologic
Stroke
Transient ischemic attack (TIA)
Subarachnoid hemorrhage
Subdural hematoma
Intracranial mass
Guillain-Barré syndrome
Spinal cord lesion
Complex migraine
Metabolic
Hypoglycemia
Hypothyroidism
Adrenal insufficiency
Electrolyte disorders
Musculoskeletal
Myopathy
Miscellaneous
Conversion disorder
Heat-related illness

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
8
Doorway information about patient
The patient is a 35-year-old woman who comes to the emergency department due to chest pain.
Vital signs
Temperature: 36.8 C (98.3 F)
Blood pressure: 120/75 mm Hg
Pulse: 98/min
Respirations: 12/min
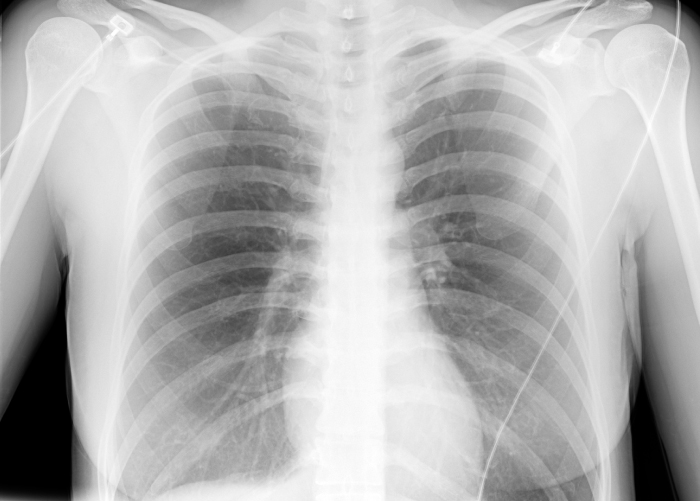
Chest x-ray is as shown in the exhibit.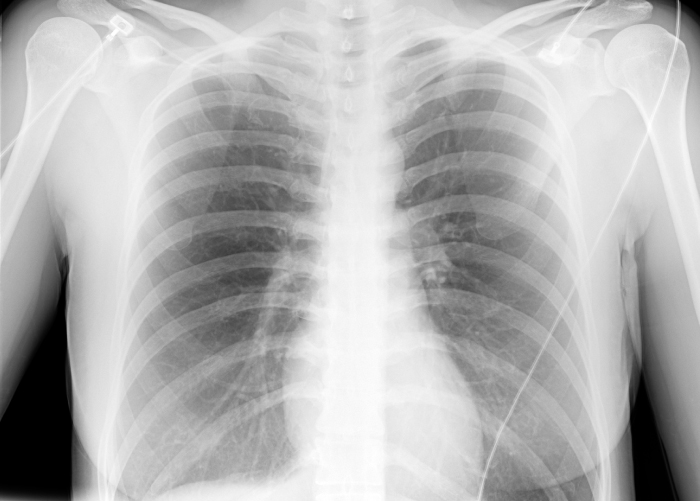
Basic differential diagnosis
Pneumonia
Gastroesophageal reflux disease
Panic disorder/hyperventilation syndrome
Hyperthyroidism
Angina
Costochondritis
The patient is a 35-year-old woman who comes to the emergency department due to chest pain.
Vital signs
Temperature: 36.8 C (98.3 F)
Blood pressure: 120/75 mm Hg
Pulse: 98/min
Respirations: 12/min
Chest x-ray is as shown in the exhibit.
Basic differential diagnosis
Pneumonia
Gastroesophageal reflux disease
Panic disorder/hyperventilation syndrome
Hyperthyroidism
Angina
Costochondritis

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
9
Doorway information about patient
The patient is a 30-year-old woman who comes to the clinic due to abdominal pain.
Vital signs
Temperature: 38.5 C (101.3 F)
Blood pressure: 120/75 mm Hg
Pulse: 98/min
Respirations: 22/min
Basic differential diagnosis
Gastrointestinal
Appendicitis
Acute cholecystitis
Pancreatitis
Inflammatory bowel disease
Irritable bowel syndrome
Diverticulitis
Bowel obstruction
Acute gastroenteritis
Urinary
Urinary tract infection/pyelonephritis
Renal colic
Reproductive
Pelvic inflammatory disease
Pelvic abscess
Endometriosis
Ovarian cyst/torsion
Ectopic pregnancy
Spontaneous abortion
Miscellaneous
Shingles
Aortic dissection
The patient is a 30-year-old woman who comes to the clinic due to abdominal pain.
Vital signs
Temperature: 38.5 C (101.3 F)
Blood pressure: 120/75 mm Hg
Pulse: 98/min
Respirations: 22/min
Basic differential diagnosis
Gastrointestinal
Appendicitis
Acute cholecystitis
Pancreatitis
Inflammatory bowel disease
Irritable bowel syndrome
Diverticulitis
Bowel obstruction
Acute gastroenteritis
Urinary
Urinary tract infection/pyelonephritis
Renal colic
Reproductive
Pelvic inflammatory disease
Pelvic abscess
Endometriosis
Ovarian cyst/torsion
Ectopic pregnancy
Spontaneous abortion
Miscellaneous
Shingles
Aortic dissection

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
10
Doorway information about patient
The patient is a 56-year-old man who comes to the office for a blood pressure check and medication refill.
Vital signs
Temperature: 36.1 C (97 F)
Blood pressure: 150/90 mm Hg
Pulse: 80/min
Respirations: 16/min
Basic differential diagnosis
When patients come for follow-up of known conditions, the primary diagnosis is known. However, you should be aware of complications and associated conditions.
Congestive cardiac failure
Coronary artery disease (angina)
Peripheral vascular disease
Retinopathy
Side effects of the medications
The patient is a 56-year-old man who comes to the office for a blood pressure check and medication refill.
Vital signs
Temperature: 36.1 C (97 F)
Blood pressure: 150/90 mm Hg
Pulse: 80/min
Respirations: 16/min
Basic differential diagnosis
When patients come for follow-up of known conditions, the primary diagnosis is known. However, you should be aware of complications and associated conditions.
Congestive cardiac failure
Coronary artery disease (angina)
Peripheral vascular disease
Retinopathy
Side effects of the medications

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
11
Doorway information about patient
The patient is a 60-year-old man who comes to the emergency department due to acute shortness of breath.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 110/70 mm Hg
Pulse: 90/min
Respirations: 26/min
Basic differential diagnosis
Pulmonary embolism
Congestive heart failure
Chronic obstructive pulmonary disease exacerbation
Pneumonia
Spontaneous pneumothorax
Asthma exacerbation
Anxiety/panic attack
The patient is a 60-year-old man who comes to the emergency department due to acute shortness of breath.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 110/70 mm Hg
Pulse: 90/min
Respirations: 26/min
Basic differential diagnosis
Pulmonary embolism
Congestive heart failure
Chronic obstructive pulmonary disease exacerbation
Pneumonia
Spontaneous pneumothorax
Asthma exacerbation
Anxiety/panic attack

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
12
Doorway information about patient
The patient is a 27-year-old woman who comes to the office due to a rash.
Vital signs
Temperature: 36.8 C (98.3 F)
Blood pressure: 120/75 mm Hg
Pulse: 78/min
Respirations: 16/min
Basic differential diagnosis
Infections Bacterial (eg, cellulitis)
Viral (eg, herpes zoster/shingles)
Fungal (eg, tinea corporis)
Parasitic (eg, scabies)
Psoriasis
Acne vulgaris
Rosacea
Immune/autoimmune (eg, systemic lupus erythematosus, erythema multiforme)
Allergic/irritant (eg, contact dermatitis, drug rash, photodermatitis, urticaria)
Stasis dermatitis
Bullous disorders (eg, bullous pemphigoid, dermatitis herpetiformis)
The patient is a 27-year-old woman who comes to the office due to a rash.
Vital signs
Temperature: 36.8 C (98.3 F)
Blood pressure: 120/75 mm Hg
Pulse: 78/min
Respirations: 16/min
Basic differential diagnosis
Infections Bacterial (eg, cellulitis)
Viral (eg, herpes zoster/shingles)
Fungal (eg, tinea corporis)
Parasitic (eg, scabies)
Psoriasis
Acne vulgaris
Rosacea
Immune/autoimmune (eg, systemic lupus erythematosus, erythema multiforme)
Allergic/irritant (eg, contact dermatitis, drug rash, photodermatitis, urticaria)
Stasis dermatitis
Bullous disorders (eg, bullous pemphigoid, dermatitis herpetiformis)

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
13
Doorway information about patient
The patient is a 50-year-old man who comes to the office due to fatigue and weight loss.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 120/76 mm Hg
Pulse: 78/min
Respirations: 18/min
Basic differential diagnosis
Infection
HIV
Tuberculosis
Metabolic disorders
Diabetes mellitus
Thyroid disorder
Adrenal insufficiency
Malignancy
Solid tumor
Hematologic malignancy
Gastrointestinal
Hepatitis
Malabsorption
Other
Depression
Eating disorder
Medication side effect
The patient is a 50-year-old man who comes to the office due to fatigue and weight loss.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 120/76 mm Hg
Pulse: 78/min
Respirations: 18/min
Basic differential diagnosis
Infection
HIV
Tuberculosis
Metabolic disorders
Diabetes mellitus
Thyroid disorder
Adrenal insufficiency
Malignancy
Solid tumor
Hematologic malignancy
Gastrointestinal
Hepatitis
Malabsorption
Other
Depression
Eating disorder
Medication side effect

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
14
Doorway information about patient
The patient is a 50-year-old man who comes to the clinic due to impotence.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 150/80 mm Hg
Pulse: 80/min
Respirations: 16/min
Basic differential diagnosis
Cardiovascular
Atherosclerotic vascular disease
Metabolic/endocrine
Diabetes
Hypogonadism
Hyperprolactinemia
Neurologic
Spinal cord disorders
Psychological
Anxiety
Depression
Alcohol or other substance abuse
Other
Medications (eg, antihypertensives)
The patient is a 50-year-old man who comes to the clinic due to impotence.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 150/80 mm Hg
Pulse: 80/min
Respirations: 16/min
Basic differential diagnosis
Cardiovascular
Atherosclerotic vascular disease
Metabolic/endocrine
Diabetes
Hypogonadism
Hyperprolactinemia
Neurologic
Spinal cord disorders
Psychological
Anxiety
Depression
Alcohol or other substance abuse
Other
Medications (eg, antihypertensives)

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
15
Doorway information about patient
The patient is a 35-year-old woman who comes to the office due to jaundice.
Vital signs
Temperature: 38.5 C (101.3 F)
Blood pressure: 120/75 mm Hg
Pulse: 98/min
Respirations: 22/min
Basic differential diagnosis
Infectious hepatitis
Hemolytic jaundice
Alcoholic hepatitis
Drug-induced hepatitis
Primary biliary cirrhosis
Wilson disease
Hemochromatosis
Malignancy
The patient is a 35-year-old woman who comes to the office due to jaundice.
Vital signs
Temperature: 38.5 C (101.3 F)
Blood pressure: 120/75 mm Hg
Pulse: 98/min
Respirations: 22/min
Basic differential diagnosis
Infectious hepatitis
Hemolytic jaundice
Alcoholic hepatitis
Drug-induced hepatitis
Primary biliary cirrhosis
Wilson disease
Hemochromatosis
Malignancy

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
16
Doorway information about patient
The patient is a 25-year-old woman who comes to the clinic due to a sore throat.
Vital signs
Temperature: 38.3 C (101 F)
Blood pressure: 120/70 mm Hg
Pulse: 90/min
Respirations: 22/min
Basic differential diagnosis
Viral pharyngitis
Bacterial pharyngitis Group A streptococcal pharyngitis
Mycoplasma pneumoniaNeisseria gonorrhea
Epstein-Barr virus mononucleosis
Allergic rhinitis/postnasal drip
Chronic tonsillitis
Primary HIV
The patient is a 25-year-old woman who comes to the clinic due to a sore throat.
Vital signs
Temperature: 38.3 C (101 F)
Blood pressure: 120/70 mm Hg
Pulse: 90/min
Respirations: 22/min
Basic differential diagnosis
Viral pharyngitis
Bacterial pharyngitis Group A streptococcal pharyngitis
Mycoplasma pneumoniaNeisseria gonorrhea
Epstein-Barr virus mononucleosis
Allergic rhinitis/postnasal drip
Chronic tonsillitis
Primary HIV

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
17
Doorway information about patient
You will be speaking with the mother of a 1-year-old with fever.
Basic differential diagnosis
Respiratory tract infection
Ear infection
Exanthematous disease
Meningitis
Urinary tract infection
Gastroenteritis
You will be speaking with the mother of a 1-year-old with fever.
Basic differential diagnosis
Respiratory tract infection
Ear infection
Exanthematous disease
Meningitis
Urinary tract infection
Gastroenteritis

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
18
Doorway information about patient
The patient is a 29-year-old woman with known sickle cell anemia who comes to the emergency department due to chest pain.
Vital signs
Temperature: 38.5 C (101.3 F)
Blood pressure: 120/75 mm Hg
Pulse: 110/min
Respirations: 22/min
Clinical images
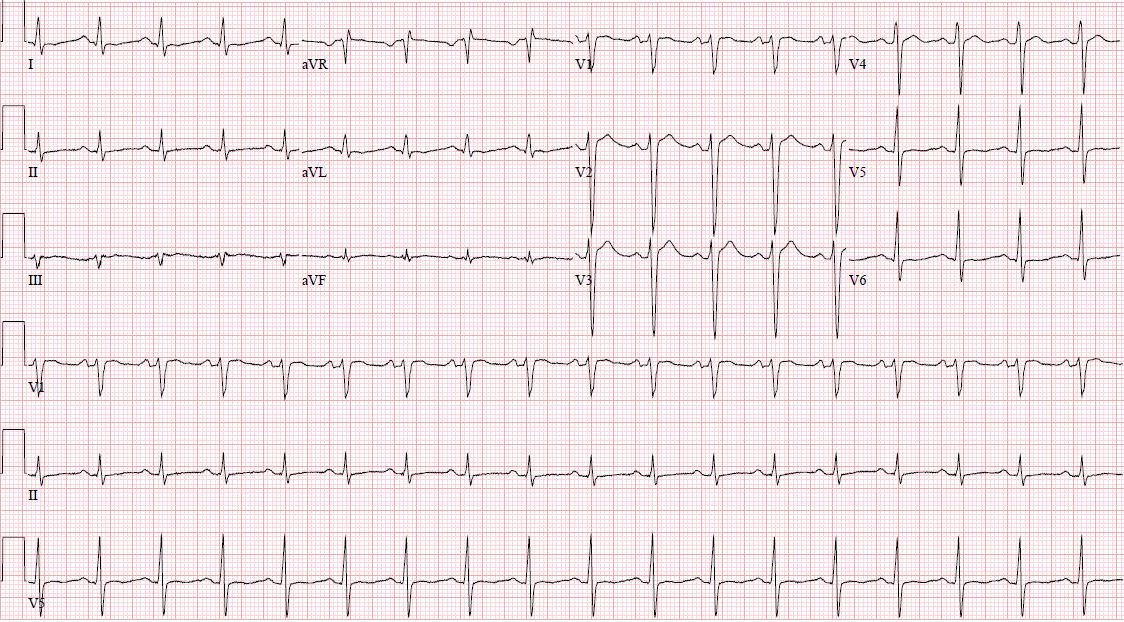
Electrocardiogram is shown in the image.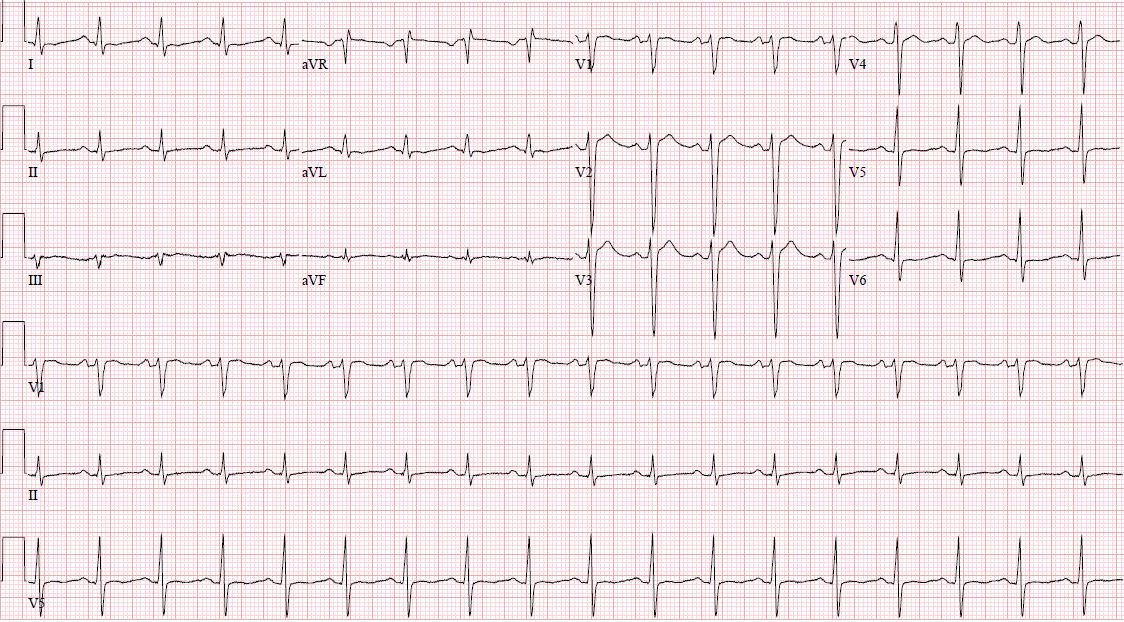
Basic differential diagnosis
Hematologic
Chest syndrome due to sickle cell anemia
Cardiovascular
Pericarditis
Acute coronary syndrome
Pulmonary
Pneumonia
Pulmonary thromboembolism
Musculoskeletal
Costochondritis
Salmonella osteomyelitis
Other
Panic attacks
The patient is a 29-year-old woman with known sickle cell anemia who comes to the emergency department due to chest pain.
Vital signs
Temperature: 38.5 C (101.3 F)
Blood pressure: 120/75 mm Hg
Pulse: 110/min
Respirations: 22/min
Clinical images
Electrocardiogram is shown in the image.
Basic differential diagnosis
Hematologic
Chest syndrome due to sickle cell anemia
Cardiovascular
Pericarditis
Acute coronary syndrome
Pulmonary
Pneumonia
Pulmonary thromboembolism
Musculoskeletal
Costochondritis
Salmonella osteomyelitis
Other
Panic attacks

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
19
Doorway information about patient
The patient is a 66-year-old man who comes to the clinic due to constipation.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 120/70 mm Hg
Pulse: 70/min
Respirations: 16/min
Basic differential diagnosis
Functional constipation
Obstructive lesions (eg, bowel obstruction, carcinoma of colon)
Metabolic disturbances (eg, hypothyroidism, diabetes mellitus, hypercalcemia)
Neurologic dysfunction (eg, stroke, autonomic neuropathy, spinal cord trauma, multiple sclerosis, Parkinson disease)
Medication-induced (eg, iron preparations, opiates, anticholinergics)
The patient is a 66-year-old man who comes to the clinic due to constipation.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 120/70 mm Hg
Pulse: 70/min
Respirations: 16/min
Basic differential diagnosis
Functional constipation
Obstructive lesions (eg, bowel obstruction, carcinoma of colon)
Metabolic disturbances (eg, hypothyroidism, diabetes mellitus, hypercalcemia)
Neurologic dysfunction (eg, stroke, autonomic neuropathy, spinal cord trauma, multiple sclerosis, Parkinson disease)
Medication-induced (eg, iron preparations, opiates, anticholinergics)

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
20
Doorway information about patient
The patient is a 45-year-old woman who comes to the office due to acute right upper quadrant abdominal pain.
Vital signs
Temperature: 38.3 C (101 F)
Blood pressure: 130/80 mm Hg
Pulse: 100/min
Respirations: 20/min
Basic differential diagnosis
Gastrointestinal
Acute cholecystitis
Biliary colic
Acute hepatitis
Peptic ulcer (perforation)
Acute pancreatitis (biliary pain)
Pulmonary
Right lower lobe pneumonia
Cardiovascular
Myocardial infarction
Heart failure with hepatic congestion
Miscellaneous
Herpes zoster (shingles)
The patient is a 45-year-old woman who comes to the office due to acute right upper quadrant abdominal pain.
Vital signs
Temperature: 38.3 C (101 F)
Blood pressure: 130/80 mm Hg
Pulse: 100/min
Respirations: 20/min
Basic differential diagnosis
Gastrointestinal
Acute cholecystitis
Biliary colic
Acute hepatitis
Peptic ulcer (perforation)
Acute pancreatitis (biliary pain)
Pulmonary
Right lower lobe pneumonia
Cardiovascular
Myocardial infarction
Heart failure with hepatic congestion
Miscellaneous
Herpes zoster (shingles)

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
21
Doorway information about patient
The patient is a 20-year-old woman who comes to the office due to burning during urination.
Vital signs
Temperature: 38.3 C (100.9 F)
Blood pressure: 110/80 mm Hg
Pulse: 82/min
Respirations: 16/min
Basic differential diagnosis
Cystitis
Pyelonephritis
Urethritis
Vulvovaginitis
Pelvic inflammatory disease
The patient is a 20-year-old woman who comes to the office due to burning during urination.
Vital signs
Temperature: 38.3 C (100.9 F)
Blood pressure: 110/80 mm Hg
Pulse: 82/min
Respirations: 16/min
Basic differential diagnosis
Cystitis
Pyelonephritis
Urethritis
Vulvovaginitis
Pelvic inflammatory disease

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
22
Doorway information about patient
The patient is a 30-year-old man who comes to the office to refill medications for HIV.
Vital signs
Temperature: 37.1 C (98.8 F)
Blood pressure: 120/75 mm Hg
Pulse: 78/min
Respirations: 16/min
Basic differential diagnosis
HIV
The patient is a 30-year-old man who comes to the office to refill medications for HIV.
Vital signs
Temperature: 37.1 C (98.8 F)
Blood pressure: 120/75 mm Hg
Pulse: 78/min
Respirations: 16/min
Basic differential diagnosis
HIV

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
23
Doorway information about patient
The patient is a 53-year-old man who comes to the emergency department due to right knee pain and swelling.
Vital signs
Temperature: 38.3 C (101 F)
Blood pressure: 130/60 mm Hg
Pulse: 80/min
Respirations: 18/min
Basic differential diagnosis
Osteoarthritis
Septic arthritis and bursitis
Pseudogout and gout
Reactive arthritis
Traumatic knee injury
Lyme disease
Monoarticular rheumatoid arthritis
Psoriatic arthritis
The patient is a 53-year-old man who comes to the emergency department due to right knee pain and swelling.
Vital signs
Temperature: 38.3 C (101 F)
Blood pressure: 130/60 mm Hg
Pulse: 80/min
Respirations: 18/min
Basic differential diagnosis
Osteoarthritis
Septic arthritis and bursitis
Pseudogout and gout
Reactive arthritis
Traumatic knee injury
Lyme disease
Monoarticular rheumatoid arthritis
Psoriatic arthritis

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
24
Doorway information about patient
The patient is a 55-year-old man who comes to the emergency department due to chest pain.
Vital signs
Temperature: 37.1 C (98.7 F)
Blood pressure: 130/80 mm Hg
Pulse: 78/min
Respirations: 20/min
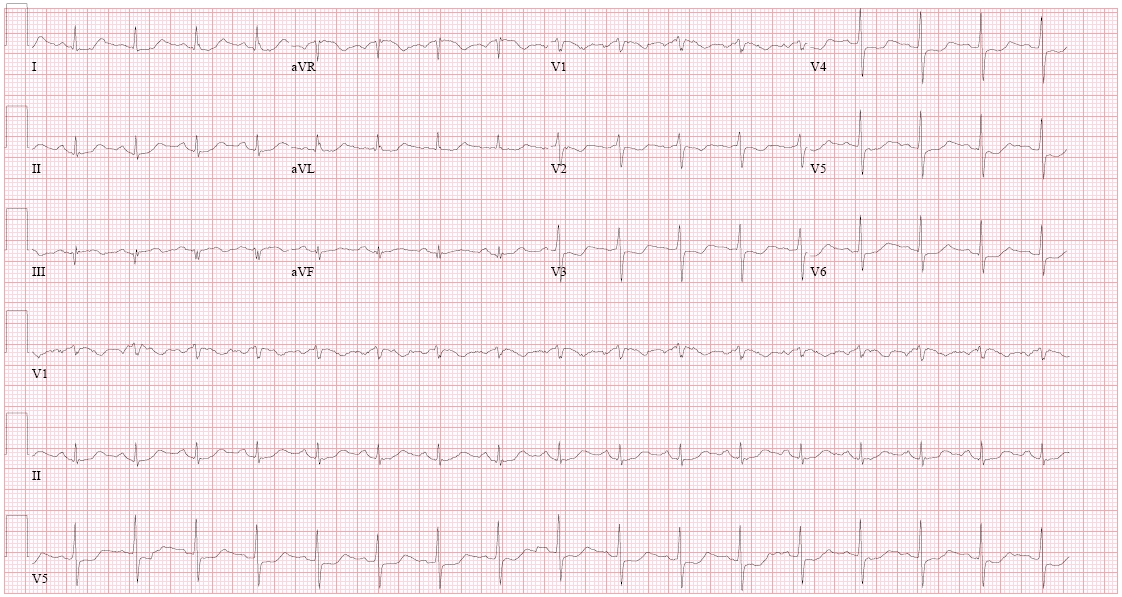
Clinical images
ECG is shown in the image.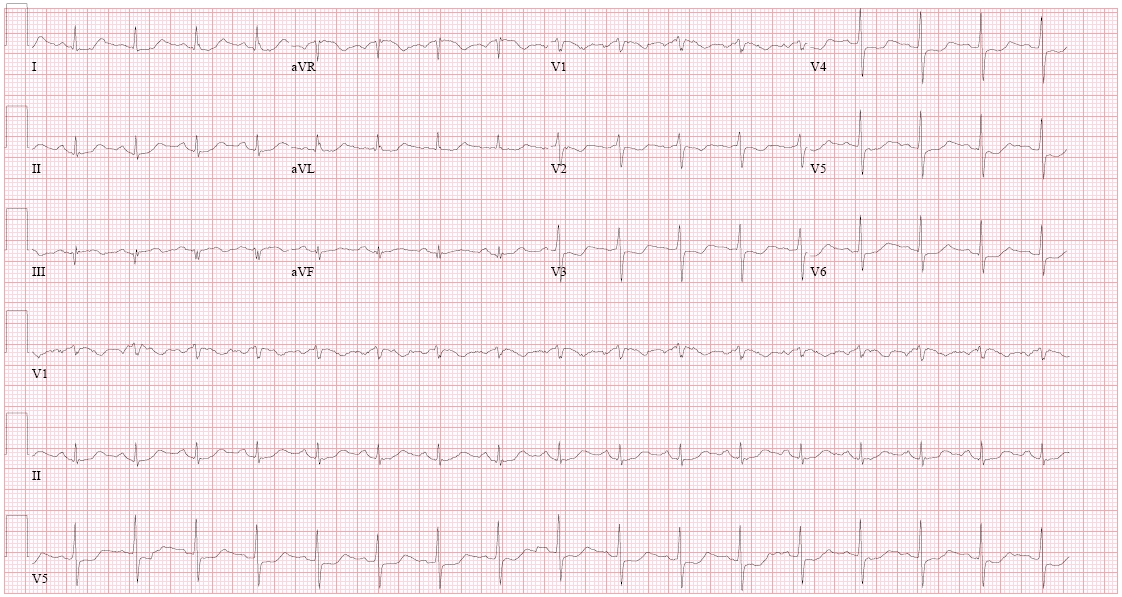
Basic differential diagnosis
Myocardial infarction
Unstable angina
Pulmonary embolism
Costochondritis
Pleuritis
Pericarditis
Aortic dissection
Gastroesophageal reflux
Esophageal perforation
The patient is a 55-year-old man who comes to the emergency department due to chest pain.
Vital signs
Temperature: 37.1 C (98.7 F)
Blood pressure: 130/80 mm Hg
Pulse: 78/min
Respirations: 20/min
Clinical images
ECG is shown in the image.
Basic differential diagnosis
Myocardial infarction
Unstable angina
Pulmonary embolism
Costochondritis
Pleuritis
Pericarditis
Aortic dissection
Gastroesophageal reflux
Esophageal perforation

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
25
Doorway information about patient
The patient is a 65-year-old woman who comes to the office due to loss of hearing.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 130/86 mm Hg
Pulse: 80/min
Respirations: 16/min
Basic differential diagnosis
Conductive hearing loss
Cerumen impaction
Otitis media with effusion
Tympanic membrane perforation
Otosclerosis
Foreign body in ear canal
Cholesteatoma
Tympanosclerosis
Tumor of the ear canal or middle ear
Sensorineural hearing loss
Presbycusis (age-related hearing loss)
Ototoxicity
Noise-induced hearing loss
Ménière disease
Diabetes
Acoustic neuroma
The patient is a 65-year-old woman who comes to the office due to loss of hearing.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 130/86 mm Hg
Pulse: 80/min
Respirations: 16/min
Basic differential diagnosis
Conductive hearing loss
Cerumen impaction
Otitis media with effusion
Tympanic membrane perforation
Otosclerosis
Foreign body in ear canal
Cholesteatoma
Tympanosclerosis
Tumor of the ear canal or middle ear
Sensorineural hearing loss
Presbycusis (age-related hearing loss)
Ototoxicity
Noise-induced hearing loss
Ménière disease
Diabetes
Acoustic neuroma

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
26
Doorway information about patient
The patient is a 53-year-old man who comes to the emergency department due to epigastric pain.
Vital signs
Temperature: 36.1 C (97 F)
Blood pressure: 120/70 mm Hg
Pulse: 84/min
Respirations: 16/min
Abdominal x-ray is as shown in the exhibit.
Basic differential diagnosis
Peptic ulcer
Gastritis
Esophagitis (GERD)
Carcinoma of esophagus, stomach, or pancreas
Acute or chronic pancreatitis
Cholecystitis
Hepatitis
Acute coronary event
The patient is a 53-year-old man who comes to the emergency department due to epigastric pain.
Vital signs
Temperature: 36.1 C (97 F)
Blood pressure: 120/70 mm Hg
Pulse: 84/min
Respirations: 16/min
Abdominal x-ray is as shown in the exhibit.

Basic differential diagnosis
Peptic ulcer
Gastritis
Esophagitis (GERD)
Carcinoma of esophagus, stomach, or pancreas
Acute or chronic pancreatitis
Cholecystitis
Hepatitis
Acute coronary event

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
27
Doorway information about patient
The patient is a 50-year-old man who comes to the office due to blurred vision.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 160/90 mm Hg
Pulse: 70/min
Respirations: 22/min
Basic differential diagnosis
Diabetes mellitus
Cataract
Hypertensive retinopathy
Glaucoma
Macular degeneration
Brain lesions
Hyperviscosity syndrome (eg, polycythemia)
Illicit drugs
Temporal arteritis (usually starts unilaterally)
Trauma to or infections of the eye (if unilateral)
The patient is a 50-year-old man who comes to the office due to blurred vision.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 160/90 mm Hg
Pulse: 70/min
Respirations: 22/min
Basic differential diagnosis
Diabetes mellitus
Cataract
Hypertensive retinopathy
Glaucoma
Macular degeneration
Brain lesions
Hyperviscosity syndrome (eg, polycythemia)
Illicit drugs
Temporal arteritis (usually starts unilaterally)
Trauma to or infections of the eye (if unilateral)

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
28
Doorway information about patient
The patient is a 70-year-old man with insomnia.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 130/90 mm Hg
Pulse: 58/min
Respirations: 16/min
Basic differential diagnosis
Depression
Post-traumatic stress disorder
Anxiety disorder
Chronic pain syndromes
Adverse effect of medication
Age-related sleep changes
Thyroid problems
Sleep apnea
Restless legs syndrome
The patient is a 70-year-old man with insomnia.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 130/90 mm Hg
Pulse: 58/min
Respirations: 16/min
Basic differential diagnosis
Depression
Post-traumatic stress disorder
Anxiety disorder
Chronic pain syndromes
Adverse effect of medication
Age-related sleep changes
Thyroid problems
Sleep apnea
Restless legs syndrome

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
29
Doorway information about patient
The patient is a 65-year-old man who comes to the office due to difficulty with urination.
Vital signs
Temperature: 37.2 C (99 F)
Blood pressure: 130/80 mm Hg
Pulse: 92/min
Respirations: 16/min
Basic differential diagnosis
Benign prostatic hyperplasia
Prostatitis
UTI/cystitis
Carcinoma of the prostate
Stone in the urinary tract (obstructive)
Carcinoma of the bladder
Neurological dysfunction
Drug-induced bladder dysfunction
The patient is a 65-year-old man who comes to the office due to difficulty with urination.
Vital signs
Temperature: 37.2 C (99 F)
Blood pressure: 130/80 mm Hg
Pulse: 92/min
Respirations: 16/min
Basic differential diagnosis
Benign prostatic hyperplasia
Prostatitis
UTI/cystitis
Carcinoma of the prostate
Stone in the urinary tract (obstructive)
Carcinoma of the bladder
Neurological dysfunction
Drug-induced bladder dysfunction

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
30
Doorway information about patient
The patient is a 32-year-old woman who comes to the emergency department due to multiple bruises.
Vital signs
Temperature: 37.4 C (99.3 F)
Blood pressure: 120/80 mm Hg
Pulse: 90/min
Respirations: 16/min
Basic differential diagnosis
Accident
Physical assault
Spousal abuse
Bleeding disorders
Collagen vascular disorders
The patient is a 32-year-old woman who comes to the emergency department due to multiple bruises.
Vital signs
Temperature: 37.4 C (99.3 F)
Blood pressure: 120/80 mm Hg
Pulse: 90/min
Respirations: 16/min
Basic differential diagnosis
Accident
Physical assault
Spousal abuse
Bleeding disorders
Collagen vascular disorders

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
31
Doorway information about patient
The patient is a 60-year-old man who comes to the emergency department due to lower abdominal pain.
Vital signs
Temperature: 38.3 C (101 F)
Blood pressure: 130/84 mm Hg
Pulse: 98/min
Respirations: 22/min
Basic differential diagnosis
Diverticulitis
Renal colic
Appendicitis
Ischemic colitis
Infectious colitis
Abdominal aortic aneurysm
Intestinal obstruction
The patient is a 60-year-old man who comes to the emergency department due to lower abdominal pain.
Vital signs
Temperature: 38.3 C (101 F)
Blood pressure: 130/84 mm Hg
Pulse: 98/min
Respirations: 22/min
Basic differential diagnosis
Diverticulitis
Renal colic
Appendicitis
Ischemic colitis
Infectious colitis
Abdominal aortic aneurysm
Intestinal obstruction

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
32
Doorway information about patient
The patient is a 35-year-old man who comes to the office due to cough and chest pain.
Vital signs
Temperature: 38.7 C (101.7 F)
Blood pressure: 130/80 mm Hg
Pulse: 94/min
Respirations: 24/min
Basic differential diagnosis
Pneumonia
Pleuritic pain
Pleural effusion
Pulmonary edema
Tuberculosis
Pulmonary embolism
Lung cancer
Infective endocarditis
GERD
The patient is a 35-year-old man who comes to the office due to cough and chest pain.
Vital signs
Temperature: 38.7 C (101.7 F)
Blood pressure: 130/80 mm Hg
Pulse: 94/min
Respirations: 24/min
Basic differential diagnosis
Pneumonia
Pleuritic pain
Pleural effusion
Pulmonary edema
Tuberculosis
Pulmonary embolism
Lung cancer
Infective endocarditis
GERD

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
33
Doorway information about patient
The patient is a 35-year-old man who comes to the office due to fatigue.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 120/80 mm Hg
Pulse: 82/min
Respirations: 16/min
Basic differential diagnosis
Depression
Anemia
Thyroid disorders
HIV/AIDS
Chronic fatigue syndrome
The patient is a 35-year-old man who comes to the office due to fatigue.
Vital signs
Temperature: 37 C (98.6 F)
Blood pressure: 120/80 mm Hg
Pulse: 82/min
Respirations: 16/min
Basic differential diagnosis
Depression
Anemia
Thyroid disorders
HIV/AIDS
Chronic fatigue syndrome

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
34
Doorway information about patient
The patient is a 16-year-old girl who comes to the office due to amenorrhea.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 120/70 mm Hg
Pulse: 76/min
Respirations: 16/min
Basic differential diagnosis
Pregnancy
Primary amenorrhea Chromosomal disorders
Abnormal müllerian development
Androgen insensitivity
Secondary amenorrhea Eating disorder
Hyperprolactinemia
Thyroid dysfunction
Polycystic ovarian syndrome
Functional hypothalamic amenorrhea
Postpill amenorrhea
Hypothalamic/pituitary mass
The patient is a 16-year-old girl who comes to the office due to amenorrhea.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 120/70 mm Hg
Pulse: 76/min
Respirations: 16/min
Basic differential diagnosis
Pregnancy
Primary amenorrhea Chromosomal disorders
Abnormal müllerian development
Androgen insensitivity
Secondary amenorrhea Eating disorder
Hyperprolactinemia
Thyroid dysfunction
Polycystic ovarian syndrome
Functional hypothalamic amenorrhea
Postpill amenorrhea
Hypothalamic/pituitary mass

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
35
Doorway information about patient
The patient is a 35-year-old woman who comes to the emergency department due to breathlessness and anxiety.
Vital signs
Temperature: 36.1 C (97 F)
Blood pressure: 130/80 mm Hg
Pulse: 94/min
Respirations: 22/min
Basic differential diagnosis
Anxiety secondary to medical condition (eg, hyperthyroidism, arrhythmias)
Substance abuse
Panic disorder
Generalized anxiety disorder
Adjustment disorder with anxious mood
Acute stress disorder or post-traumatic stress disorder
Hypochondriasis
The patient is a 35-year-old woman who comes to the emergency department due to breathlessness and anxiety.
Vital signs
Temperature: 36.1 C (97 F)
Blood pressure: 130/80 mm Hg
Pulse: 94/min
Respirations: 22/min
Basic differential diagnosis
Anxiety secondary to medical condition (eg, hyperthyroidism, arrhythmias)
Substance abuse
Panic disorder
Generalized anxiety disorder
Adjustment disorder with anxious mood
Acute stress disorder or post-traumatic stress disorder
Hypochondriasis

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
36
Doorway information about patient
The patient is a 45-year-old man who comes to the emergency department due to vomiting blood.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 100/60 mm Hg
Pulse: 90/min
Respirations: 18/min
Basic differential diagnosis
Peptic ulcer
Esophageal and gastric varices
Mallory-Weiss tear
Gastritis
Erosive esophagitis
Gastric malignancy
Vascular ectasia
The patient is a 45-year-old man who comes to the emergency department due to vomiting blood.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 100/60 mm Hg
Pulse: 90/min
Respirations: 18/min
Basic differential diagnosis
Peptic ulcer
Esophageal and gastric varices
Mallory-Weiss tear
Gastritis
Erosive esophagitis
Gastric malignancy
Vascular ectasia

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
37
Doorway information about patient
The patient is a 50-year-old man who comes to the office due to difficulty swallowing.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 130/90 mm Hg
Pulse: 85/min
Respirations: 16/min
Basic differential diagnosis
Oropharyngeal dysphagia Neuromuscular (stroke, parkinsonism, multiple sclerosis)
Mechanical obstruction (Zenker diverticulum, thyromegaly)
Skeletal muscle disorders (myasthenia gravis, muscular dystrophies, polymyositis)
Miscellaneous (medications, radiation)
Esophageal dysphagia Mechanical obstruction (esophageal carcinoma, benign strictures, webs and rings [Schatzki])
Abnormal motility (achalasia, scleroderma)
Gastroesophageal reflux disease
Miscellaneous (diabetes, alcoholism)
The patient is a 50-year-old man who comes to the office due to difficulty swallowing.
Vital signs
Temperature: 36.7 C (98.1 F)
Blood pressure: 130/90 mm Hg
Pulse: 85/min
Respirations: 16/min
Basic differential diagnosis
Oropharyngeal dysphagia Neuromuscular (stroke, parkinsonism, multiple sclerosis)
Mechanical obstruction (Zenker diverticulum, thyromegaly)
Skeletal muscle disorders (myasthenia gravis, muscular dystrophies, polymyositis)
Miscellaneous (medications, radiation)
Esophageal dysphagia Mechanical obstruction (esophageal carcinoma, benign strictures, webs and rings [Schatzki])
Abnormal motility (achalasia, scleroderma)
Gastroesophageal reflux disease
Miscellaneous (diabetes, alcoholism)

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
38
Doorway information about patient
The patient is a 70-year-old man who comes to the office due to frequent falls.
Vital signs
Temperature: 37.1 C (98.7 F)
Blood pressure: 130/80 mm Hg
Pulse: 78/min
Respirations: 20/min
Basic differential diagnosis
Neurologic
Cerebellar disease (alcohol, tumor, stroke)
Parkinson disease
Brain tumor
Seizure
Decreased vision
Metabolic
Diabetic neuropathy
Hypoglycemia
Thyroid disease
Cardiovascular
Valvular heart disease
Miscellaneous
Medication side effect
Vitamin B12 deficiency
Vertigo
The patient is a 70-year-old man who comes to the office due to frequent falls.
Vital signs
Temperature: 37.1 C (98.7 F)
Blood pressure: 130/80 mm Hg
Pulse: 78/min
Respirations: 20/min
Basic differential diagnosis
Neurologic
Cerebellar disease (alcohol, tumor, stroke)
Parkinson disease
Brain tumor
Seizure
Decreased vision
Metabolic
Diabetic neuropathy
Hypoglycemia
Thyroid disease
Cardiovascular
Valvular heart disease
Miscellaneous
Medication side effect
Vitamin B12 deficiency
Vertigo

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
39
Doorway information about patient
The patient is a 56-year-old woman who comes to the emergency department due to vomiting blood.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 90/60 mm Hg
Pulse: 98/min
Respirations: 20/min
Clinical images
The patient has vomited into a pan of water at the bedside, as shown in the image.
Basic differential diagnosis
Peptic ulcer disease
Gastric erosions
Esophageal varices
Mallory-Weiss tear
Esophagitis
Duodenitis
Malignancy (esophageal and gastric)
The patient is a 56-year-old woman who comes to the emergency department due to vomiting blood.
Vital signs
Temperature: 36.7 C (98 F)
Blood pressure: 90/60 mm Hg
Pulse: 98/min
Respirations: 20/min
Clinical images
The patient has vomited into a pan of water at the bedside, as shown in the image.

Basic differential diagnosis
Peptic ulcer disease
Gastric erosions
Esophageal varices
Mallory-Weiss tear
Esophagitis
Duodenitis
Malignancy (esophageal and gastric)

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
40
Doorway information about patient
The patient is a 35-year-old woman who comes to the office due to acute right lumbar and lower abdominal pain.
Vital signs
Temperature: 38.3 C (100.9 F)
Blood pressure: 110/70 mm Hg
Pulse: 100/min
Respirations: 16/min
Basic differential diagnosis
Renal colic
Ovarian torsion
Urinary tract infection/pyelonephritis
Pelvic inflammatory disease
Mittelschmerz
Appendicitis
Threatened abortion
Ectopic pregnancy
Dysmenorrhea
Endometriosis
Fibroids
The patient is a 35-year-old woman who comes to the office due to acute right lumbar and lower abdominal pain.
Vital signs
Temperature: 38.3 C (100.9 F)
Blood pressure: 110/70 mm Hg
Pulse: 100/min
Respirations: 16/min
Basic differential diagnosis
Renal colic
Ovarian torsion
Urinary tract infection/pyelonephritis
Pelvic inflammatory disease
Mittelschmerz
Appendicitis
Threatened abortion
Ectopic pregnancy
Dysmenorrhea
Endometriosis
Fibroids

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
41
Doorway information about patient
The patient is a 30-year-old man who comes to the emergency department due to a new-onset seizure.
Vital signs
Temperature: 37.2 C (99 F)
Blood pressure: 120/80 mm Hg
Pulse: 82/min, regular
Respirations: 18/min
Basic differential diagnosis
Seizures (secondary to head trauma, infections, drugs, metabolic disorders)
Hypoglycemia
Syncope
Migraine
Stroke
Psychogenic seizure
Space-occupying lesions
Alcohol or drug withdrawal
The patient is a 30-year-old man who comes to the emergency department due to a new-onset seizure.
Vital signs
Temperature: 37.2 C (99 F)
Blood pressure: 120/80 mm Hg
Pulse: 82/min, regular
Respirations: 18/min
Basic differential diagnosis
Seizures (secondary to head trauma, infections, drugs, metabolic disorders)
Hypoglycemia
Syncope
Migraine
Stroke
Psychogenic seizure
Space-occupying lesions
Alcohol or drug withdrawal

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
42
Doorway information about patient
The patient is a 60-year-old man who comes to the office due to dizziness.
Vital signs
Temperature: 36.1 C (97 F)
Blood pressure: 140/90 mm Hg
Pulse: 80/min
Respirations: 16/min
Basic differential diagnosis
Vertigo (benign paroxysmal positional vertigo, labyrinthitis, Ménière disease, posterior circulation stroke)
Lightheadedness (hypotension, postural hypotension, arrhythmia, anemia, congestive heart failure)
Dysequilibrium (anxiety, autonomic dysfunction)
TIA or stroke
Medication effect
Hypoglycemia
The patient is a 60-year-old man who comes to the office due to dizziness.
Vital signs
Temperature: 36.1 C (97 F)
Blood pressure: 140/90 mm Hg
Pulse: 80/min
Respirations: 16/min
Basic differential diagnosis
Vertigo (benign paroxysmal positional vertigo, labyrinthitis, Ménière disease, posterior circulation stroke)
Lightheadedness (hypotension, postural hypotension, arrhythmia, anemia, congestive heart failure)
Dysequilibrium (anxiety, autonomic dysfunction)
TIA or stroke
Medication effect
Hypoglycemia

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck
43
Doorway information about patient
The patient is a 23-year-old man who comes to the emergency department due to rectal bleeding.
Vital signs
Temperature: 38.3 C (101 F)
Blood pressure: 110/60 mm Hg
Pulse: 90/min
Respirations: 18/min
Basic differential diagnosis
Young patients
Anal fistula/fissure
Hemorrhoid
Inflammatory bowel disease
Infectious colitis
Neoplasm
Vascular ectasia
Elderly patients
Diverticulosis
Angiodysplasia
Malignancy/polyp
Ischemic colitis
Inflammatory bowel disease
The patient is a 23-year-old man who comes to the emergency department due to rectal bleeding.
Vital signs
Temperature: 38.3 C (101 F)
Blood pressure: 110/60 mm Hg
Pulse: 90/min
Respirations: 18/min
Basic differential diagnosis
Young patients
Anal fistula/fissure
Hemorrhoid
Inflammatory bowel disease
Infectious colitis
Neoplasm
Vascular ectasia
Elderly patients
Diverticulosis
Angiodysplasia
Malignancy/polyp
Ischemic colitis
Inflammatory bowel disease

Unlock Deck
Unlock for access to all 43 flashcards in this deck.
Unlock Deck
k this deck



