Deck 1: Advanced Clinical Medicine
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question

Unlock Deck
Sign up to unlock the cards in this deck!
Unlock Deck
Unlock Deck
1/1121
Play
Full screen (f)
Deck 1: Advanced Clinical Medicine
1
A randomized, parallel-group, controlled clinical trial evaluates the effectiveness of an anti-inflammatory intervention as treatment for neuropathic pain following spinal cord injury. Participants with varying levels and severities of spinal cord injury are randomly assigned to either a 24-week, anti-inflammatory diet treatment group or a control group. Primary outcomes consist of changes in pain scores and markers of inflammation at 6 months. Preliminary analyses reveal a significant reduction in pain scores in the treatment group from baseline to 6 months (p = 0.03). There was a significant reduction in pain scores among nonobese subjects (p = 0.01) and a nonsignificant increase in pain scores among obese subjects (p = 0.06). Which of the following is the best explanation for these differences in findings between obese and nonobese subjects?
A)Confounding bias
B)Effect modification
C)Hawthorne effect
D)Randomization failure
E)Selection bias
A)Confounding bias
B)Effect modification
C)Hawthorne effect
D)Randomization failure
E)Selection bias
B
Explanation:
Effect modification (interaction bias) occurs when an extraneous variable (effect modifier) changes the direction or strength of the effect that the independent variable (exposure or treatment) has on the dependent variable (outcome). For instance, aspirin use is associated with Reye syndrome in children but not adults; therefore, age (effect modifier) modifies the effect of aspirin (exposure) on Reye syndrome development (outcome). Stratification based on the modifier (eg, analyzing the data by age group) can help detect effect modification as it typically shows different effects in each stratum (eg, children, adults); separate measures of effect should be reported for each stratum.
In this case, the treatment group (ie, 24-week anti-inflammatory diet) had a significant reduction in pain scores from baseline to 6 months compared to the control group (p < 0.03). However, the effect was significant only among nonobese (nonsignificant among obese subjects), and went in opposite directions depending on weight status (reduced pain among nonobese versus increased pain among obese). Therefore, weight status is an effect modifier that changes the effect of the intervention diet on pain scores. A stratified analysis by weight group (nonobese and obese) helps to estimate the real effect.
(Choices A and D) Effect modification is sometimes confused with confounding bias, which occurs when an extraneous variable (ie, confounder) associated with both the exposure and the outcome obscures the association between the exposure and the outcome. With confounding (unlike with effect modification), no change in the strength or direction of the effect is typically seen with stratification. Randomization usually helps remove confounder effects. If successful randomization has occurred, characteristics such as obesity, age, and sex should be similarly distributed between the treatment and the control groups, and confounding should be minimized. Because obesity was found to be an effect modifier and not a confounder, neither confounding bias nor randomization failure explain the differences seen between obese and nonobese groups.
(Choice C) The Hawthorne (observer) effect is the tendency of study subjects to change their behavior as a result of their awareness of being studied. However, it is commonly seen in studies concerning behavioral outcomes or outcomes that can be influenced by behavioral changes.
(Choice E) Selection bias can occur with inappropriate (random or nonrandom) selection methods or through selective attrition of the study participants. Randomization in a clinical trial reduces selection bias.
Educational objective:
Effect modification occurs when the magnitude or direction of the effect of the independent variable on the dependent variable (outcome) varies depending on the level of a third variable (effect modifier). Separate (stratified) analyses should be conducted for each level of the effect modifier.
Explanation:
Effect modification (interaction bias) occurs when an extraneous variable (effect modifier) changes the direction or strength of the effect that the independent variable (exposure or treatment) has on the dependent variable (outcome). For instance, aspirin use is associated with Reye syndrome in children but not adults; therefore, age (effect modifier) modifies the effect of aspirin (exposure) on Reye syndrome development (outcome). Stratification based on the modifier (eg, analyzing the data by age group) can help detect effect modification as it typically shows different effects in each stratum (eg, children, adults); separate measures of effect should be reported for each stratum.
In this case, the treatment group (ie, 24-week anti-inflammatory diet) had a significant reduction in pain scores from baseline to 6 months compared to the control group (p < 0.03). However, the effect was significant only among nonobese (nonsignificant among obese subjects), and went in opposite directions depending on weight status (reduced pain among nonobese versus increased pain among obese). Therefore, weight status is an effect modifier that changes the effect of the intervention diet on pain scores. A stratified analysis by weight group (nonobese and obese) helps to estimate the real effect.
(Choices A and D) Effect modification is sometimes confused with confounding bias, which occurs when an extraneous variable (ie, confounder) associated with both the exposure and the outcome obscures the association between the exposure and the outcome. With confounding (unlike with effect modification), no change in the strength or direction of the effect is typically seen with stratification. Randomization usually helps remove confounder effects. If successful randomization has occurred, characteristics such as obesity, age, and sex should be similarly distributed between the treatment and the control groups, and confounding should be minimized. Because obesity was found to be an effect modifier and not a confounder, neither confounding bias nor randomization failure explain the differences seen between obese and nonobese groups.
(Choice C) The Hawthorne (observer) effect is the tendency of study subjects to change their behavior as a result of their awareness of being studied. However, it is commonly seen in studies concerning behavioral outcomes or outcomes that can be influenced by behavioral changes.
(Choice E) Selection bias can occur with inappropriate (random or nonrandom) selection methods or through selective attrition of the study participants. Randomization in a clinical trial reduces selection bias.
Educational objective:
Effect modification occurs when the magnitude or direction of the effect of the independent variable on the dependent variable (outcome) varies depending on the level of a third variable (effect modifier). Separate (stratified) analyses should be conducted for each level of the effect modifier.
2
A group of graduate students conducted a case-control study to evaluate the association between sporadic frontotemporal dementia and thyroid disease. A total of 80 patients with sporadic frontotemporal dementia along with 160 age and sex surrogate informant matched controls participated in the study. Results showed that thyroid disease was associated with frontotemporal dementia with an odds ratio of 2.5 and a 95% confidence interval: 0.9-7.9. The students reported that patients with sporadic frontotemporal dementia were 2.5 times more likely to have thyroid disease compared to patients with no sporadic frontotemporal dementia. They concluded that there is a statistically significant association between sporadic frontotemporal dementia and thyroid disease. Based on this information, which of the following is the best evaluation of the students' conclusion?
A)Correct because the confidence interval is wide
B)Correct because the findings are clinically significant
C)Correct because the odds ratio is greater than zero
D)Incorrect because the authors did not perform a power calculation
E)Incorrect because the findings are not statistically significant
A)Correct because the confidence interval is wide
B)Correct because the findings are clinically significant
C)Correct because the odds ratio is greater than zero
D)Incorrect because the authors did not perform a power calculation
E)Incorrect because the findings are not statistically significant
E
Explanation:
This case-control study evaluated the association between sporadic frontotemporal dementia and thyroid disease in 80 patients with sporadic frontotemporal dementia and 160 age and sex surrogate informant matched controls. The results of the study showed that thyroid disease was associated with frontotemporal dementia with an odds ratio (OR) of 2.5 and a 95% confidence interval (CI): 0.9-7.9.
The OR is a measure of association between an exposure to a risk factor and an outcome, usually defined as the odds of an exposure in cases divided by the odds of the same exposure in controls. The OR may also be defined as the odds of outcome among exposed patients relative to nonexposed patients. These OR definitions are mathematically equivalent.
OR = (odds of outcome in exposed group) / (odds of outcome in nonexposed group)
An OR > 1.0 indicates that the exposure is associated with an increase in odds of outcome.
The CI of an OR indicates, with a certain confidence level, whether a given OR is statistically different from the null value (OR = 1.0). A CI that excludes the null value is statistically significant (at that confidence level).
In this study, the 95% CI includes the null value (OR = 1.0). Based on these results, thyroid disease is not significantly associated (ie, OR is not significantly greater than 1) with sporadic frontotemporal dementia (Choice C). Therefore, the students' conclusion is incorrect.
(Choice A) Wider CIs lead to less precise estimates. The width of the CI by itself does not determine statistical significance, which depends on whether the CI includes the null value.
(Choice B) The students concluded that there is a statistically (rather than a clinically) significant association between sporadic frontotemporal dementia and thyroid disease. However, the statistical evidence shows that the association was not significant; therefore, the students' conclusion is incorrect.
(Choice D) There is not enough information given to determine whether a power calculation was performed. A low statistical power may explain the lack of statistical significance for the association. Regardless, the association was not significant, and therefore the students' conclusion is incorrect.
Educational objective:
An odds ratio (OR) >1 indicates that the exposure is associated with an increase in the odds of an outcome. A confidence interval that excludes the null value (OR = 1) is statistically significant.
Explanation:
This case-control study evaluated the association between sporadic frontotemporal dementia and thyroid disease in 80 patients with sporadic frontotemporal dementia and 160 age and sex surrogate informant matched controls. The results of the study showed that thyroid disease was associated with frontotemporal dementia with an odds ratio (OR) of 2.5 and a 95% confidence interval (CI): 0.9-7.9.
The OR is a measure of association between an exposure to a risk factor and an outcome, usually defined as the odds of an exposure in cases divided by the odds of the same exposure in controls. The OR may also be defined as the odds of outcome among exposed patients relative to nonexposed patients. These OR definitions are mathematically equivalent.
OR = (odds of outcome in exposed group) / (odds of outcome in nonexposed group)
An OR > 1.0 indicates that the exposure is associated with an increase in odds of outcome.
The CI of an OR indicates, with a certain confidence level, whether a given OR is statistically different from the null value (OR = 1.0). A CI that excludes the null value is statistically significant (at that confidence level).
In this study, the 95% CI includes the null value (OR = 1.0). Based on these results, thyroid disease is not significantly associated (ie, OR is not significantly greater than 1) with sporadic frontotemporal dementia (Choice C). Therefore, the students' conclusion is incorrect.
(Choice A) Wider CIs lead to less precise estimates. The width of the CI by itself does not determine statistical significance, which depends on whether the CI includes the null value.
(Choice B) The students concluded that there is a statistically (rather than a clinically) significant association between sporadic frontotemporal dementia and thyroid disease. However, the statistical evidence shows that the association was not significant; therefore, the students' conclusion is incorrect.
(Choice D) There is not enough information given to determine whether a power calculation was performed. A low statistical power may explain the lack of statistical significance for the association. Regardless, the association was not significant, and therefore the students' conclusion is incorrect.
Educational objective:
An odds ratio (OR) >1 indicates that the exposure is associated with an increase in the odds of an outcome. A confidence interval that excludes the null value (OR = 1) is statistically significant.
3
A 65-year-old woman with a medical history significant for tobacco use, hypertension, and laparoscopic cholecystectomy is brought to the operating room for a lumbar discectomy. She is placed in the prone position. General anesthesia is induced with propofol and rocuronium, and the patient is intubated without complications. Anesthesia is maintained with sevoflurane. Five minutes later, prior to incision, the ventilator sounds an alarm. Peak pressures have increased to >40 mm Hg, and end-tidal CO2 has decreased from 30 to 20 mm Hg. Blood pressure is 90/60 mm Hg and pulse is 114/min. On examination, the patient is sedated and paralyzed. Heart sounds are rapid and regular. Bilateral wheezing is noted on auscultation of the lungs. What is the next step in management?
A)Administer albuterol and proceed with surgery
B)Examine the skin under the surgical drapes
C)Place the patient in the reverse Trendelenburg position
D)Reposition the endotracheal tube
A)Administer albuterol and proceed with surgery
B)Examine the skin under the surgical drapes
C)Place the patient in the reverse Trendelenburg position
D)Reposition the endotracheal tube
B
Explanation:
This patient's hypotension, elevated peak pressures (eg, bronchospasm), and decreased end-tidal CO2 (eg, decreased cardiac output and CO2 delivery to the lungs) shortly after anesthetic induction are concerning for anaphylaxis. Anaphylaxis is classically caused by an acute IgE-mediated release of inflammatory mediators (eg, histamine) in response to an allergen. In the perioperative setting, the most common allergens are neuromuscular-blocking agents (eg, rocuronium), antibiotics, skin antisepsis products (eg, povidone-iodine, chlorhexidine), and blood products.
caused
Because anaphylaxis is a clinical diagnosis that depends on history and physical examination, the diagnosis can be challenging in surgical patients for several reasons, including the following:
Patients' inability to communicate symptoms
Ongoing physiologic stress, volume shifts, and medication effects, initially attributed to shock
Concealment of skin findings under surgical drapes
If there is concern for anaphylaxis, the next step is thorough physical examination, especially inspection under the surgical drapes for cutaneous signs (eg, rash, flushing), which are present in most patients. Once the diagnosis is made, epinephrine should be promptly administered.
(Choice A) Albuterol may help relieve bronchospasm. Unlike epinephrine, it does not improve hypotension and prevent impending circulatory collapse. This patient's hypotension and ventilatory issues should be completely investigated and addressed prior to proceeding with surgery.
(Choice C) Reverse Trendelenburg positioning tilts the body so that the head is elevated and the feet are lowered. However, this (or any upright) posture increases the risk of cardiac arrest in anaphylaxis by decreasing venous return and ventricular filling in the setting of ongoing peripheral vasodilation. Instead, patients should be placed supine with the feet elevated to increase venous return.
Reverse Trendelenburg positioning
(Choice D) Malpositioning of the endotracheal tube into a mainstem bronchus can cause increased peak pressures (ie, the smaller radius increases resistance) and hypoxemia (eg, from contralateral lung atelectasis). However, this typically causes unilaterally absent breath sounds (vs bilateral breath sounds [wheezing]).
Educational objective:
Anaphylaxis is a clinical diagnosis that can be difficult to recognize in surgical patients. Early recognition is dependent on thorough physical examination (eg, inspecting skin under the surgical drapes).
References:
Anaphylaxis during the perioperative period.
(http://www.ncbi.nlm.nih.gov/pubmed/25885604)
Explanation:
This patient's hypotension, elevated peak pressures (eg, bronchospasm), and decreased end-tidal CO2 (eg, decreased cardiac output and CO2 delivery to the lungs) shortly after anesthetic induction are concerning for anaphylaxis. Anaphylaxis is classically caused by an acute IgE-mediated release of inflammatory mediators (eg, histamine) in response to an allergen. In the perioperative setting, the most common allergens are neuromuscular-blocking agents (eg, rocuronium), antibiotics, skin antisepsis products (eg, povidone-iodine, chlorhexidine), and blood products.
caused
Because anaphylaxis is a clinical diagnosis that depends on history and physical examination, the diagnosis can be challenging in surgical patients for several reasons, including the following:
Patients' inability to communicate symptoms
Ongoing physiologic stress, volume shifts, and medication effects, initially attributed to shock
Concealment of skin findings under surgical drapes
If there is concern for anaphylaxis, the next step is thorough physical examination, especially inspection under the surgical drapes for cutaneous signs (eg, rash, flushing), which are present in most patients. Once the diagnosis is made, epinephrine should be promptly administered.
(Choice A) Albuterol may help relieve bronchospasm. Unlike epinephrine, it does not improve hypotension and prevent impending circulatory collapse. This patient's hypotension and ventilatory issues should be completely investigated and addressed prior to proceeding with surgery.
(Choice C) Reverse Trendelenburg positioning tilts the body so that the head is elevated and the feet are lowered. However, this (or any upright) posture increases the risk of cardiac arrest in anaphylaxis by decreasing venous return and ventricular filling in the setting of ongoing peripheral vasodilation. Instead, patients should be placed supine with the feet elevated to increase venous return.
Reverse Trendelenburg positioning
(Choice D) Malpositioning of the endotracheal tube into a mainstem bronchus can cause increased peak pressures (ie, the smaller radius increases resistance) and hypoxemia (eg, from contralateral lung atelectasis). However, this typically causes unilaterally absent breath sounds (vs bilateral breath sounds [wheezing]).
Educational objective:
Anaphylaxis is a clinical diagnosis that can be difficult to recognize in surgical patients. Early recognition is dependent on thorough physical examination (eg, inspecting skin under the surgical drapes).
References:
Anaphylaxis during the perioperative period.
(http://www.ncbi.nlm.nih.gov/pubmed/25885604)
4
A 6-year-old boy is brought to the clinic for influenza vaccination in September. He has been healthy and has no nasal congestion, rhinorrhea, or other symptoms. The patient had 2 episodes of otitis media during infancy and has mild intermittent asthma treated with inhaled albuterol as needed. He has no other respiratory problems and takes no other medications. His older brother had cystic fibrosis and recently died at age 10 from a severe influenza infection; the patient's sweat test was negative. The patient has no medication allergies but has developed a splotchy, itchy red rash to egg-containing products in the past. Eggs have since been excluded from his diet. He has no history of other reactions to egg or to immunizations. Vital signs and physical examination are normal. Which of the following is the best next step in management of this patient?
A)Administer inactivated intramuscular influenza vaccine
B)Administer live-attenuated intranasal influenza vaccine
C)Do not administer influenza vaccine
D)Order radioallergosorbent testing
E)Refer for allergy consultation before administering any influenza vaccine
A)Administer inactivated intramuscular influenza vaccine
B)Administer live-attenuated intranasal influenza vaccine
C)Do not administer influenza vaccine
D)Order radioallergosorbent testing
E)Refer for allergy consultation before administering any influenza vaccine

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
5
A 13-year-old girl is brought to the emergency department by paramedics due to difficulty breathing that started 30 minutes ago. She was at an amusement park with her family when she was stung by a bee on her left ear. The patient experienced shortness of breath; itching; and a raised, red rash on her face and neck minutes after the sting. Medical history includes asthma that is well controlled on budesonide. Blood pressure is 80/40 mm Hg, pulse is 144/min, and respirations are 28/min. Pulse oximetry shows 92% on a nonrebreather mask. The patient is in obvious distress. The oropharynx is patent and without swelling. On auscultation of the lungs, severe bilateral wheezing is present. Heart sounds are rapid without murmurs. There are multiple raised erythematous papules on her face, neck, and upper chest. The patient's vital signs normalize, and symptoms resolve completely an hour after a single dose of epinephrine and nebulized albuterol. What is the appropriate disposition for this patient?
A)Admit to hospital for desensitization
B)Admit to hospital for observation
C)Discharge home now with epinephrine autoinjector only
D)Discharge home now with epinephrine autoinjector plus antihistamine
E)Discharge home now with epinephrine autoinjector plus corticosteroid
A)Admit to hospital for desensitization
B)Admit to hospital for observation
C)Discharge home now with epinephrine autoinjector only
D)Discharge home now with epinephrine autoinjector plus antihistamine
E)Discharge home now with epinephrine autoinjector plus corticosteroid

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
6
A randomized controlled study of chronically sleep-deprived (<6.5 hr per night), morbidly obese subjects examined whether sleep extension is associated with weight loss and metabolic and endocrinal improvements. The intervention consisted of education regarding sleep hygiene and a gradual change to subjects' bedtimes to earlier in the evening. Participants underwent general screening at visit 1 with collection of baseline parameters; then, 2 months later, at visit 2, subjects were randomized into either an intervention group or a comparison group. Researchers evaluated several parameters, including sleep duration, sleepiness, and sleep quality. The following results were reported: Note: Data is reported as mean ± standard deviation.
*p < 0.05.
1 ESS (Epworth Sleepiness Scale [daytime sleepiness]) >10 = sleepy.
2 PSQI (Pittsburgh Sleep Quality Index [subjective sleep quality]) >5 = abnormal.
There were statistically significant differences in all 3 parameters between visit 1 and visit 2. Which of the following is the best explanation for the difference between findings at the screening and randomization visits?
A)Allocation bias
B)Confounding bias
C)Hawthorne effect
D)Placebo effect
E)Selection bias
*p < 0.05.
1 ESS (Epworth Sleepiness Scale [daytime sleepiness]) >10 = sleepy.
2 PSQI (Pittsburgh Sleep Quality Index [subjective sleep quality]) >5 = abnormal.
There were statistically significant differences in all 3 parameters between visit 1 and visit 2. Which of the following is the best explanation for the difference between findings at the screening and randomization visits?
A)Allocation bias
B)Confounding bias
C)Hawthorne effect
D)Placebo effect
E)Selection bias

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
7
A 40-year-old male is brought to the emergency room with confusion, lethargy, and decreased strength in his left arm. He is HIV-positive. He was diagnosed several months ago, but he refused any kind of therapy. His most recent CD4 cell count was 40/μL. A lumbar puncture is performed, but cerebral spinal fluid findings and cytology are inconclusive. A CT scan reveals a well-defined small focal lesion in the right cerebral hemisphere. Biopsy findings are consistent with primary CNS lymphoma. You decide to proceed with radiation therapy and corticosteroids, and to institute HAART. Which of the following is the best prognostic sign for this patient's condition?
A)The stage of the lymphoma
B)Decrease in EBV DNA in CSF
C)Increase in soluble B-cell marker in CSF
D)Increase in CD4 count
E)Rapid response to radiation therapy
A)The stage of the lymphoma
B)Decrease in EBV DNA in CSF
C)Increase in soluble B-cell marker in CSF
D)Increase in CD4 count
E)Rapid response to radiation therapy

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
8
A 25-year-old man comes to the emergency department after being stung by a wasp on his right arm 30 minutes ago. He reports generalized itching and mild local pain. He has no other medical conditions. Temperature is 36.7 C (98.1 F), blood pressure is 122/81 mm Hg, pulse is 108/min, and respirations are 22/min. Pulse oximetry is 94% on room air. Examination shows a 2 × 2 cm, erythematous, elevated, warm, and mildly tender area on the right arm. Multiple wheals are visible on the trunk and extremities. There is no tongue swelling or stridor. Bilateral wheezes are present on lung auscultation. The remainder of the examination is normal. Which of the following is the most appropriate next step in management of this patient?
A)Inhaled albuterol
B)Intramuscular epinephrine
C)Intravenous diphenhydramine
D)Intravenous methylprednisolone
E)Oral hydroxyzine
A)Inhaled albuterol
B)Intramuscular epinephrine
C)Intravenous diphenhydramine
D)Intravenous methylprednisolone
E)Oral hydroxyzine

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
9
A 16-year-old boy is brought to the office by his mother for a routine well visit. The patient has been doing well in school and has not been in the office over the past year for any sick visits. His mother says, "My son has had a girlfriend for the last few months, and I wonder if boys can receive the human papillomavirus vaccine. I am friends with his girlfriend's mother and heard that she received the vaccine a few years ago." The patient takes no daily medications and has no known drug allergies. The mother leaves the room for the examination, and the patient says that he is considering vaginal intercourse with his girlfriend. His parents have talked with him about abstinence and the importance of using a condom if having sex. The patient was sexually active with a previous girlfriend and used condoms every time. He is not sexually active with males and has never been tested for sexually transmitted infections. There is no family history of cancer. Physical examination shows no skin lesions, including in the genital area. The penis is circumcised with no visible discharge. The testes are descended bilaterally with no erythema or masses. Counseling about the prevention of pregnancy and sexually transmitted infections is provided. Which of the following is the most appropriate recommendation about the human papillomavirus vaccine in this patient?
A)The patient is beyond the recommended age for administering the vaccine
B)The risk for infection and the need for vaccination are low because the patient uses condoms
C)The vaccine is not recommended due to the patient's prior sexual activity
D)The vaccine is recommended to reduce the risk for anogenital cancers
E)The vaccine should be given to prevent male factor infertility
A)The patient is beyond the recommended age for administering the vaccine
B)The risk for infection and the need for vaccination are low because the patient uses condoms
C)The vaccine is not recommended due to the patient's prior sexual activity
D)The vaccine is recommended to reduce the risk for anogenital cancers
E)The vaccine should be given to prevent male factor infertility

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
10
A pharmaceutical company plans to conduct a study to evaluate the efficacy of the addition of a novel conjugated anti-CD22 monoclonal antibody (mAb) to frontline therapy in adults age 18-39 with newly diagnosed precursor B-cell acute lymphoblastic leukemia (ALL). Researchers will assess the adverse reactions associated with treatment with the anti-CD22 mAb. A total of 1,200 patients newly diagnosed with CD22 positive B-cell ALL will be randomized to either frontline chemotherapy or intravenous infusion of the mAb given on days 1, 8, and 15. All participants will undergo bone marrow aspirate and biopsy on day 28. The study's primary outcome measure will be event-free survival, and its secondary outcome will include disease-free survival, overall survival, and complete response. Which of the following best describes this type of study?
A)Preclinical study
B)Phase I clinical trial
C)Phase II clinical trial
D)Phase III clinical trial
E)Phase IV clinical trial
A)Preclinical study
B)Phase I clinical trial
C)Phase II clinical trial
D)Phase III clinical trial
E)Phase IV clinical trial

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
11
A 56-year-old woman in the emergency department waiting room develops shortness of breath and generalized itching. She was eating a cookie when the symptoms started. The patient is allergic to peanuts and believes the cookie contained them. She has a history of emphysema and a 20-pack-year smoking history. Temperature is 36.7 C (98.1 F), blood pressure is 88/60 mm Hg, pulse is 124/min, and respirations are 26/min. Pulse oximetry is 92% on room air. The patient is using the accessory muscles of her neck and shoulder girdle and is exhaling through pursed lips. There is no tongue swelling or stridor. Bilateral wheezes are present on lung auscultation. Skin examination is shown in the exhibit.  The patient is given an intramuscular injection of epinephrine. Ten minutes later, there is no significant change in her condition. Which of the following is the best next step in management of this patient?
The patient is given an intramuscular injection of epinephrine. Ten minutes later, there is no significant change in her condition. Which of the following is the best next step in management of this patient?
A)Inhaled albuterol
B)Intramuscular epinephrine
C)Intravenous diphenhydramine
D)Intravenous methylprednisolone
E)Subcutaneous epinephrine
 The patient is given an intramuscular injection of epinephrine. Ten minutes later, there is no significant change in her condition. Which of the following is the best next step in management of this patient?
The patient is given an intramuscular injection of epinephrine. Ten minutes later, there is no significant change in her condition. Which of the following is the best next step in management of this patient?A)Inhaled albuterol
B)Intramuscular epinephrine
C)Intravenous diphenhydramine
D)Intravenous methylprednisolone
E)Subcutaneous epinephrine

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
12
A 32-year-old Caucasian female presents to your office with persistent cough and shortness of breath. She has had three episodes of pneumonia over the last year. She had severe sinusitis one year ago, and an episode of bloody diarrhea that required hospitalization and IV antibiotic therapy six months ago. She does not smoke or consume alcohol. She denies any illicit drug use. She is currently not taking any medications. All her immunizations are up-to-date. Her blood pressure is 130/80 mmHg and heart rate is 90/min. Physical examination reveals fine crackles over the right lower lung lobe. No lower extremity edema is present. Neck palpation does not reveal any lymph node enlargement. The chest x-ray shows right lower lobe infiltrates and left upper lobe fibrosis. The ECG reveals non-specific ST segment and T wave changes. What is the best next step in the management of this patient?
A)Measurement of serum alpha-1-antitrypsin level
B)Methacholine challenge test
C)Quantitative measurement of serum Ig levels
D)Sweat chloride test
E)Ventilation/perfusion lung scan
A)Measurement of serum alpha-1-antitrypsin level
B)Methacholine challenge test
C)Quantitative measurement of serum Ig levels
D)Sweat chloride test
E)Ventilation/perfusion lung scan

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
13
A 35-year-old man is brought to the emergency department after cutting his finger with a rusty knife while doing yard work. It is a deep cut, and his wife had immediately applied a pressure dressing to stop the bleeding. His immunization status is unknown. The patient last saw his doctor about 10 years ago, and cannot recall if he received all of his childhood vaccinations. He has a deep laceration on the palmar aspect of his right middle finger. Cleaning of the wound and other wound-care measures are initiated. Which of the following is the best next step in management of this patient?
A)Send the patient home; no immunization
B)Tetanus immune globulin and tetanus toxoid
C)Tetanus immune globulin only
D)Tetanus toxoid only
A)Send the patient home; no immunization
B)Tetanus immune globulin and tetanus toxoid
C)Tetanus immune globulin only
D)Tetanus toxoid only

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
14
A 5-year-old boy is brought to the office for his annual well-child visit. The boy was briefly hospitalized a month ago for an asthma exacerbation, which was treated with albuterol and oral corticosteroids. He has been well since then except for a runny nose and cough for the past 2 days. He takes an inhaled corticosteroid daily and albuterol as needed, most recently 3 weeks ago. The patient lives at home with his mother, who is 38 weeks pregnant, and his father and 2-year-old sister. He recently started kindergarten and is doing well. Temperature is 36.7 C (98 F). The patient is tracking along the 40th and 60th percentiles for weight and height, respectively. Physical examination shows a well-appearing boy who speaks clearly in full sentences, counts to 12, and can hop on one foot. The lungs are clear to auscultation, and the remainder of the examination is unremarkable. He is scheduled to receive the second dose of measles-mumps-rubella (MMR) vaccine today. The parents say, "After his first MMR shot a few years ago, he had a fever up to 39.4 C (103 F), and we almost took him to the emergency department." Which of the following is the most appropriate next step in management of this patient?
A)Administer acetaminophen followed by MMR vaccine today
B)Administer MMR vaccine today
C)Ask if the patient has a history of egg allergy
D)Delay MMR vaccine until after the mother's delivery
E)Delay MMR vaccine until upper respiratory symptoms resolve
A)Administer acetaminophen followed by MMR vaccine today
B)Administer MMR vaccine today
C)Ask if the patient has a history of egg allergy
D)Delay MMR vaccine until after the mother's delivery
E)Delay MMR vaccine until upper respiratory symptoms resolve

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
15
A 45-year-old woman with a history of chronic menorrhagia is hospitalized for an elective hysterectomy. Her preoperative hemoglobin is 7 g/dL. She is transfused with 2 units of packed red blood cells. Two hours after starting the transfusion, the patient reports chills and malaise. Her temperature is 38.8 C (102 F), blood pressure is 120/76 mm Hg, pulse is 100/min, and respirations are 18/min. The transfusion is stopped, and she receives acetaminophen. Direct antiglobulin test and plasma free hemoglobin level are negative. Urinalysis is within normal limits. The reaction resolves 6 hours after the transfusion began. Which of the following actions could have prevented this reaction?
A)Careful cross-matching of blood
B)Leukoreduction
C)Using whole blood
D)Warming blood
E)Washing cells
A)Careful cross-matching of blood
B)Leukoreduction
C)Using whole blood
D)Warming blood
E)Washing cells

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
16
A 68-year-old man undergoing hemodialysis is being evaluated due to "difficulty breathing and chest tightness." He has not had any chest pain. The patient was feeling well when he arrived at his hemodialysis appointment. He was started on hemodialysis 15 minutes ago after a heparin flush; an intravenous iron infusion was started 5 minutes ago for iron deficiency anemia. Medical history is significant for end-stage renal disease due to uncontrolled hypertension, a small pericardial effusion, and small, bilateral pleural effusions. He has been on hemodialysis treatment for the past year. Temperature is 35.6 C (96.1 F), blood pressure is 90/60 mm Hg, pulse is 112/min, and respirations are 24/min. Pulse oximetry is 93% on room air. The patient is alert but in mild distress. Conjunctivae are pale. Lungs sounds are decreased at both bases. Bilateral wheezing is noted on auscultation of the lungs. Heart sounds are slightly muffled and rapid but without murmurs or rubs. Abdomen is soft and nontender. Skin is flushed. Mild, bilateral pitting pedal edema is present. What is the most likely cause of this patient's symptoms?
A)Acute myocardial infarction
B)Air embolism
C)Anaphylaxis
D)Pericardial tamponade
E)Pulmonary embolism
A)Acute myocardial infarction
B)Air embolism
C)Anaphylaxis
D)Pericardial tamponade
E)Pulmonary embolism

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
17
A group of rheumatologists wants to investigate 8 candidate rheumatoid arthritis (RA) susceptibility loci to identify whether single nucleotide polymorphisms (SNPs) are associated with RA in a given population. Eight SNPs (MTHFR C677T, MTHFR A1298C, TGFβ1 T869C, TNFB A252G, VDR ApaI, VDR BsmI, VDR FokI, VDR TaqI) are tested by genotyping patients with RA (n = 105) and unrelated patients without RA (n = 80) as controls. Which of the following is the most appropriate null hypothesis for this study?
A)Odds ratio is equal to 1
B)Odds ratio is not equal to 1
C)Relative risk is equal to 1
D)Relative risk is not equal to 1
A)Odds ratio is equal to 1
B)Odds ratio is not equal to 1
C)Relative risk is equal to 1
D)Relative risk is not equal to 1

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
18
A randomized study assigned patients with sickle cell anemia and silent stroke to either monthly transfusion therapy (transfusion group of 110 patients) or usual care (observation group of 105 patients). An excerpt of the study results is provided below: Which of the following adverse event estimates is most subject to selection bias?
A)Acute chest syndrome
B)Avascular hip necrosis
C)Headache
D)Iron overload
E)Vasoocclusive pain
A)Acute chest syndrome
B)Avascular hip necrosis
C)Headache
D)Iron overload
E)Vasoocclusive pain

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
19
A 64-year-old man comes to the emergency department complaining of facial swelling. He has not had such symptoms before and has no associated itching or rash. The patient's medical problems include type 2 diabetes mellitus, hypertension, and coronary artery disease. He had a myocardial infarction 7 years ago. He was recently diagnosed with congestive heart failure with systolic dysfunction. The patient's medications include ramipril, metoprolol, furosemide, spironolactone, aspirin, glyburide, and simvastatin. Physical examination shows prominent lip and tongue swelling without stridor. His symptoms subside within 24 hours after he is admitted. Which of the following is the best statement concerning the management of this patient?
A)Lisinopril can be substituted for ramipril because there is a low chance of recurrence with a different angiotensin-converting-enzyme inhibitor.
B)Losartan can be substituted for ramipril because angiotensin receptor blockers do not affect the kinin system and have a low risk for angioedema.
C)Losartan can be substituted for ramipril because the 2 drugs are antigenically distinct and do not cross react.
D)Ramipril can be continued because the risk of recurrent angioedema is very low and the benefits outweigh the risk.
E)Ramipril can be continued if combined with diphenhydramine.
A)Lisinopril can be substituted for ramipril because there is a low chance of recurrence with a different angiotensin-converting-enzyme inhibitor.
B)Losartan can be substituted for ramipril because angiotensin receptor blockers do not affect the kinin system and have a low risk for angioedema.
C)Losartan can be substituted for ramipril because the 2 drugs are antigenically distinct and do not cross react.
D)Ramipril can be continued because the risk of recurrent angioedema is very low and the benefits outweigh the risk.
E)Ramipril can be continued if combined with diphenhydramine.

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
20
A 4-month-old boy is brought to the office for a well-child visit. The boy is rolling over and cooing. He reaches for toys and mouths them frequently. He is breastfed exclusively and takes a multivitamin with iron. Last week, the patient was diagnosed with acute otitis media and croup, which were treated with a 10-day course of amoxicillin and a single dose of dexamethasone. He is currently on day 6 of antibiotics and is no longer irritable or coughing. His last fever was 4 days ago. The patient lives at home with his parents and sister age 3. His sister has a seizure disorder of unclear etiology that is well controlled on antiepileptic medication. Temperature is 36.7 C (98.1 F). Physical examination is normal for his age. The infant is scheduled to receive several immunizations today as part of the recommended schedule. The parents express concern about their son receiving the diphtheria-tetanus-acellular pertussis vaccination. The father says, "After he got his shots the first time, he had a fever of 103 and was so fussy that we had to take him to the urgent care clinic to make sure he was okay. I'm not sure I can go through that again." Based on this child's history, which of the following is the most appropriate step regarding DTaP administration in this patient?
A)Immunization is contraindicated due to his reaction to the first dose
B)Immunization is contraindicated due to his sister's seizure disorder
C)Immunization should be given today despite his history
D)Immunization should be postponed as he recently received steroids
E)Immunization should be postponed until antibiotic therapy is complete
A)Immunization is contraindicated due to his reaction to the first dose
B)Immunization is contraindicated due to his sister's seizure disorder
C)Immunization should be given today despite his history
D)Immunization should be postponed as he recently received steroids
E)Immunization should be postponed until antibiotic therapy is complete

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
21
An open-label randomized trial is conducted to compare a new nonsteroidal anti-inflammatory agent (AG) and low-dose colchicine for the treatment of gout flares in primary care. A total of 400 adults with gout flares were randomized 1:1 to AG for 7 days or low-dose colchicine three times per day for 4 days. The primary outcome was change in pain intensity from baseline measured over the first 7 days. At Day 7 follow-up, about 25% of participants in the low-dose colchicine group had switched treatment to AG, and about 15% of participants in the low-dose colchicine group had stopped treatment altogether. The primary investigator decided to preserve the original randomization for the data analysis. Which of the following describes the data analysis approach adopted by the primary investigator?
A)Correlation analysis
B)Intention-to-treat analysis
C)Per-protocol analysis
D)Regression analysis
E)Stratified analysis
A)Correlation analysis
B)Intention-to-treat analysis
C)Per-protocol analysis
D)Regression analysis
E)Stratified analysis

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
22
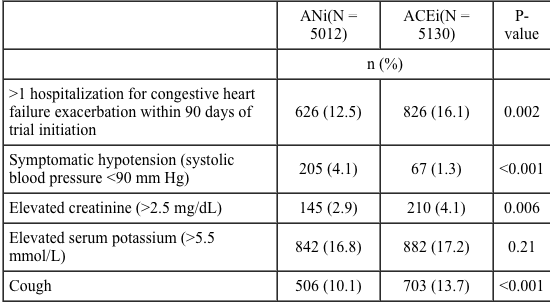
An 84-year-old man comes to the physician with persistent dyspnea despite being treated with optimal medical therapy for congestive heart failure with low left ventricular ejection fraction. A recently published randomized clinical trial compared an angiotensin-neprilysin inhibitor (ANi) to an angiotensin-converting enzyme inhibitor (ACEi) in patients who have heart failure with a reduced ejection fraction. The following results were reported:
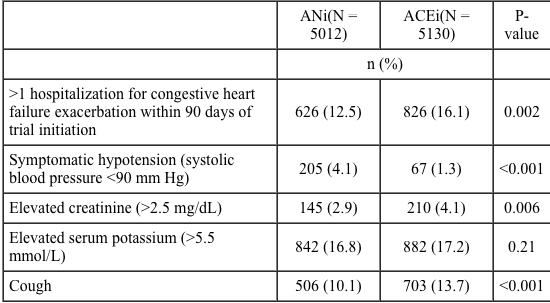 Which of the following would be of most concern when switching from an ACEi to an ANi?
Which of the following would be of most concern when switching from an ACEi to an ANi?
A)Dangerous hyperkalemia
B)Increased hospitalizations for heart failure
C)Uncomfortable cough
D)Unsafe drop in blood pressure
E)Worsening renal function
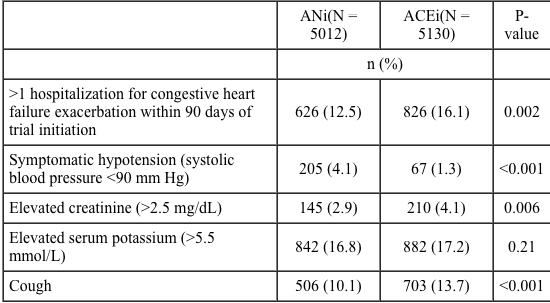 Which of the following would be of most concern when switching from an ACEi to an ANi?
Which of the following would be of most concern when switching from an ACEi to an ANi?A)Dangerous hyperkalemia
B)Increased hospitalizations for heart failure
C)Uncomfortable cough
D)Unsafe drop in blood pressure
E)Worsening renal function

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
23
A retrospective, matched-cohort study is conducted to examine the effect of medical care provided by overnight physicians on the outcomes of their scheduled elective procedures performed during the day. Patients undergoing 1 of 5 elective daytime procedures performed by a physician who worked overnight were matched to patients undergoing the same procedure by the same physician on a day when the physician did not work overnight. The study outcome was a composite of patient death and complications. The study reported that the risk of the composite outcome was higher in patients who underwent a daytime procedure performed by a physician who had worked overnight compared to patients who underwent a procedure performed by a physician who had not worked overnight (22% vs. 20%, p = 0.04). Based on these results, what is the approximate percentage of deaths and complications that can be attributed to the physician having worked overnight before the scheduled elective procedures during the day?
A)1)1
B)9)1
C)22
D)50
A)1)1
B)9)1
C)22
D)50

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
24
An 84-year-old man comes to the physician with persistent dyspnea despite being treated with optimal medical therapy for congestive heart failure with low left ventricular ejection fraction. A recently published randomized clinical trial compared an angiotensin-neprilysin inhibitor (ANi) to an angiotensin-converting enzyme inhibitor (ACEi) in patients who have heart failure with a reduced ejection fraction. The following results were reported: 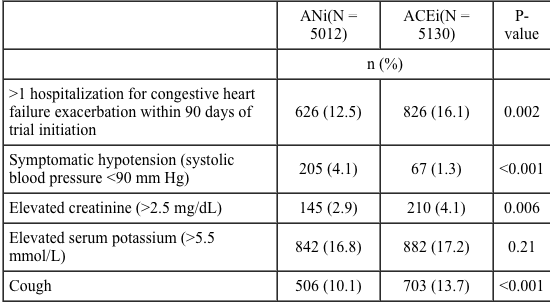 The investigators also reported the following results for patients in the angiotensin-neprilysin inhibitor (ANi) and angiotensin-converting enzyme inhibitor (ACEi) groups:
The investigators also reported the following results for patients in the angiotensin-neprilysin inhibitor (ANi) and angiotensin-converting enzyme inhibitor (ACEi) groups:
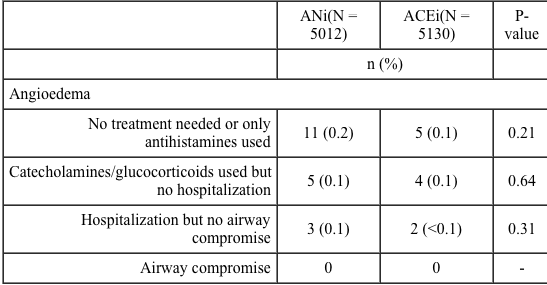 Which of the following is the best interpretation of these results
Which of the following is the best interpretation of these results
A)The interpretation of the results is confounded by the placebo effect
B)The study results reassure that there is no danger of drug-induced angioedema with the new drug due to the absence of airway compromise
C)There is a higher number of angioedema events with the new drug, warranting a larger randomized clinical trial to investigate safety
D)There is a higher number of angioedema events with the new drug, warranting postmarketing surveillance if the drug is approved
E)There is a small but statistically significant increase in the rate of angioedema with the new drug
 The investigators also reported the following results for patients in the angiotensin-neprilysin inhibitor (ANi) and angiotensin-converting enzyme inhibitor (ACEi) groups:
The investigators also reported the following results for patients in the angiotensin-neprilysin inhibitor (ANi) and angiotensin-converting enzyme inhibitor (ACEi) groups: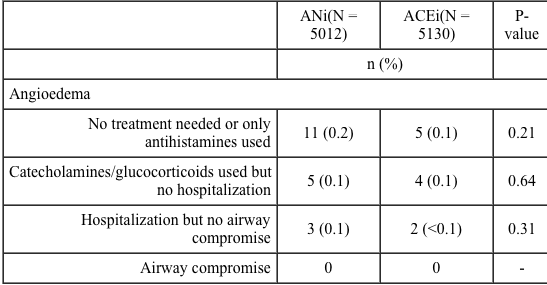 Which of the following is the best interpretation of these results
Which of the following is the best interpretation of these resultsA)The interpretation of the results is confounded by the placebo effect
B)The study results reassure that there is no danger of drug-induced angioedema with the new drug due to the absence of airway compromise
C)There is a higher number of angioedema events with the new drug, warranting a larger randomized clinical trial to investigate safety
D)There is a higher number of angioedema events with the new drug, warranting postmarketing surveillance if the drug is approved
E)There is a small but statistically significant increase in the rate of angioedema with the new drug

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
25
A 35-year-old man comes to the emergency department due to 2 days of fever and dysuria. He has a history of paraplegia as the result of a gunshot wound 5 years ago that required surgical intervention. He takes narcotics for chronic pain that has developed since the surgery. The patient is bedbound and practices intermittent urinary self-catheterization. He has had multiple admissions for recurrent urinary tract infections; urine cultures have grown multidrug-resistant organisms requiring intravenous antibiotic therapy in the past. He most recently completed a course of antibiotics a week ago. The patient says, "It feels like my urinary tract infection is coming back-I was just done with antibiotics and was hoping I would get a break!" He reports that every 5 years of life in his current state of health are equivalent to 1 year of life in full health. Which of the following measures is best described by this value?
A)Disability-adjusted life years
B)Quality-adjusted life years
C)Standard disability weight
D)Years lived with disability
E)Years of life lost
A)Disability-adjusted life years
B)Quality-adjusted life years
C)Standard disability weight
D)Years lived with disability
E)Years of life lost

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
26
A study was conducted to identify factors associated with rebleeding in patients admitted to the hospital with upper gastrointestinal hemorrhage. The medical charts of 2,488 patients were analyzed retrospectively, and a logistic regression analysis was conducted to identify potential risk factors for rebleeding. An excerpt of study results is shown below. 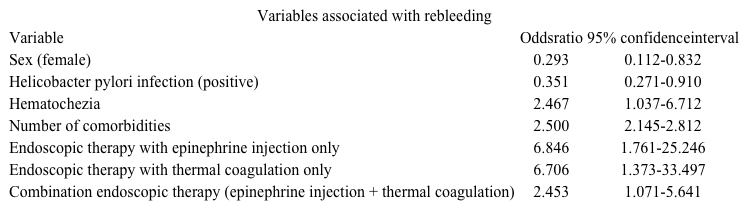 No missing data points regarding the type of endoscopic therapy received, comorbidities, or Heliobacter pylori status were reported in the study. Which of the following is the best interpretation of the study results?
No missing data points regarding the type of endoscopic therapy received, comorbidities, or Heliobacter pylori status were reported in the study. Which of the following is the best interpretation of the study results?
A)Endoscopic therapy with epinephrine injection increases the odds of controlling rebleeding
B)The average number of comorbidities in the group of patients who rebleed is 2.5
C)The odds of hematochezia are significantly higher among female patients than among male patients
D)The odds of rebleeding are about 65% lower among patients who are H pylori-positive compared to patients who are H pylori-negative
E)The odds ratio for rebleeding among patients who undergo combination endoscopic therapy represents strong evidence of causation
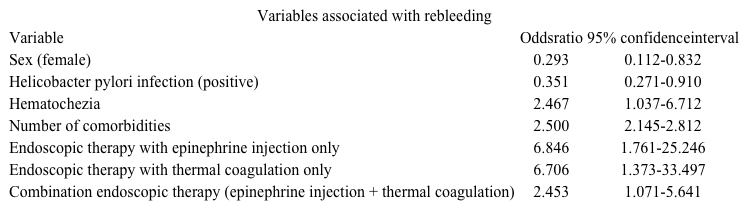 No missing data points regarding the type of endoscopic therapy received, comorbidities, or Heliobacter pylori status were reported in the study. Which of the following is the best interpretation of the study results?
No missing data points regarding the type of endoscopic therapy received, comorbidities, or Heliobacter pylori status were reported in the study. Which of the following is the best interpretation of the study results?A)Endoscopic therapy with epinephrine injection increases the odds of controlling rebleeding
B)The average number of comorbidities in the group of patients who rebleed is 2.5
C)The odds of hematochezia are significantly higher among female patients than among male patients
D)The odds of rebleeding are about 65% lower among patients who are H pylori-positive compared to patients who are H pylori-negative
E)The odds ratio for rebleeding among patients who undergo combination endoscopic therapy represents strong evidence of causation

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
27
A 32-year-old woman, gravida 2 para 1, comes to the office for a routine prenatal visit. The patient had a postpartum hemorrhage (PPH) after her first pregnancy and is worried about the possibility of PPH after her scheduled repeat cesarean delivery. She read about the effectiveness of prophylactic tranexamic acid in reducing the risk of hemorrhage after scheduled cesarean delivery and wants to discuss the results. The outcomes of the study were PPH, clinical and laboratory (blood samples at day 2) measurements of postpartum blood loss, and several adverse events after scheduled cesarean delivery at ≥34 weeks gestation. Patients received intravenous infusion of a uterotonic agent and either tranexamic acid or saline placebo within 3 minutes after cesarean delivery. A summary of the results is shown in the table below. 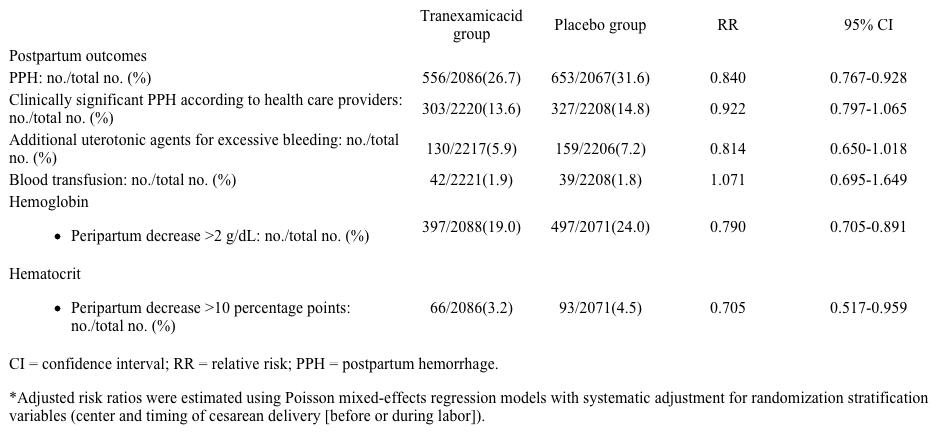 Based on the study results, which of the following conclusions is strongly justified?
Based on the study results, which of the following conclusions is strongly justified?
A)Tranexamic acid is associated with an increased risk of blood transfusions
B)Tranexamic acid significantly reduced the risk of all postpartum study outcomes except the need for blood transfusions
C)The risk of peripartum hemoglobin decrease >2 g/dL is about 80% lower in the tranexamic acid group compared to the placebo group
D)The risk of PPH is significantly reduced by 16% when tranexamic acid is used as a prophylactic compared to placebo
E)There is no significant difference in postpartum outcomes between treatment groups
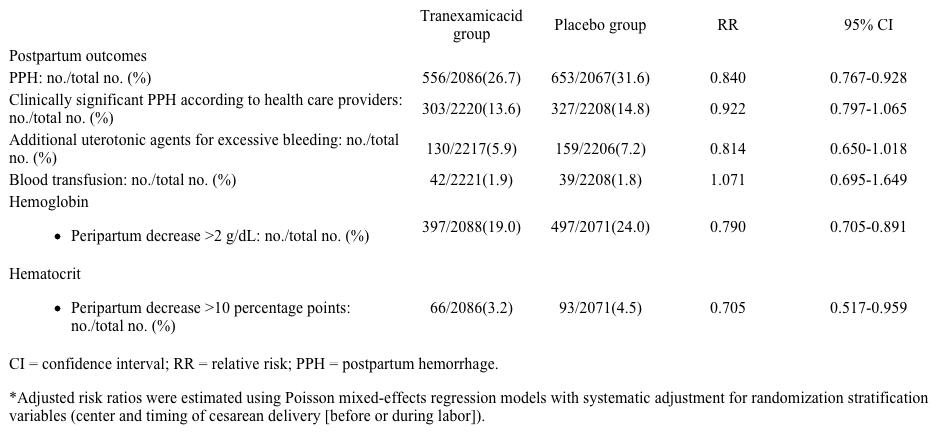 Based on the study results, which of the following conclusions is strongly justified?
Based on the study results, which of the following conclusions is strongly justified?A)Tranexamic acid is associated with an increased risk of blood transfusions
B)Tranexamic acid significantly reduced the risk of all postpartum study outcomes except the need for blood transfusions
C)The risk of peripartum hemoglobin decrease >2 g/dL is about 80% lower in the tranexamic acid group compared to the placebo group
D)The risk of PPH is significantly reduced by 16% when tranexamic acid is used as a prophylactic compared to placebo
E)There is no significant difference in postpartum outcomes between treatment groups

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
28
A 59-year-old man comes to the office for follow-up. He has a history of hypertension for which he takes 2 antihypertensive agents. The patient has no other cardiovascular problems and does not smoke. On examination, his blood pressure is 145/90 mm Hg and BMI is 25.4 kg/m2. The remainder of the examination is unremarkable. Laboratory studies show elevated fasting lipid levels, including LDL cholesterol. His 10-year risk of cardiovascular events is calculated as 10%, and a discussion regarding moderate or intensive statin therapy is initiated. The patient has read that statins may cause diabetes and asks if there is an even more increased risk with intensive compared to moderate statin therapy. Based on the abstract, what was the pooled odds ratio of major cardiovascular events among participants on intensive compared to moderate statin therapy?
A)0)33
B)0)76
C)0)85
D)1)12
E)1)30
A)0)33
B)0)76
C)0)85
D)1)12
E)1)30

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
29
A new, randomized, placebo-controlled trial studied the association between treatment with 250,000 IU cholecalciferol for 4 months following hip fracture surgery and incidence of falls. Results showed that at month 4 after surgery, 7 (6.3%) patients in the treatment group reported >1 falls compared to 23 (21.2%) in the placebo group (p < 0.01); there was a relative risk reduction of 70.3%. Treatment with 250,000 IU cholecalciferol for 4 months costs $100 per patient. Based on this information, how much would it cost to treat enough patients after hip surgery with 250,000 IU cholecalciferol to prevent >1 falls during the first 4 months of therapy?
A)$142
B)$300
C)$671
D)$1430
E)$6300
A)$142
B)$300
C)$671
D)$1430
E)$6300

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
30
A study examines the role of different tumor markers or their combinations in diagnosing pancreatic cancer in patients with a solid lesion in the pancreatic head. The following table is reported: Based on the study results, a patient with a solid lesion in the pancreatic head is most likely to be free of pancreatic cancer if which of the following tests or combinations is negative?
A)Marker 1
B)Marker 2
C)Marker 3
D)Parallel combination
E)Serial combination
A)Marker 1
B)Marker 2
C)Marker 3
D)Parallel combination
E)Serial combination

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
31
A 69-year-old man with chronic kidney disease comes to the office to discuss options for dialysis. The patient wishes to choose the dialysis modality that will allow him to live the longest. The following Kaplan-Meier survival curve is obtained from a prospective study on the survival of 1800 patients who began dialysis with either hemodialysis (HD) or peritoneal dialysis (PD) and were followed for 5 years. The event of interest was death while on dialysis. 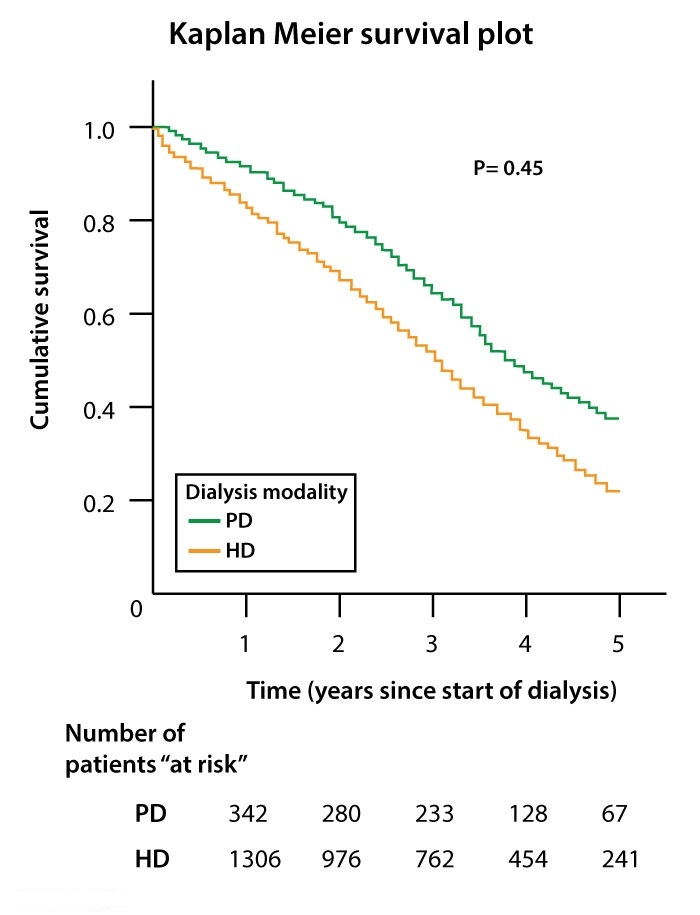 Based on the findings of this study, which dialysis option offers improved survival?
Based on the findings of this study, which dialysis option offers improved survival?
A)HD, as median survival was greater than for PD
B)HD, as survival was greater at end of study than for PD
C)HD or PD, as survival was not significantly different
D)PD, as median survival was greater than for HD
E)PD, as survival was greater at end of study than for HD
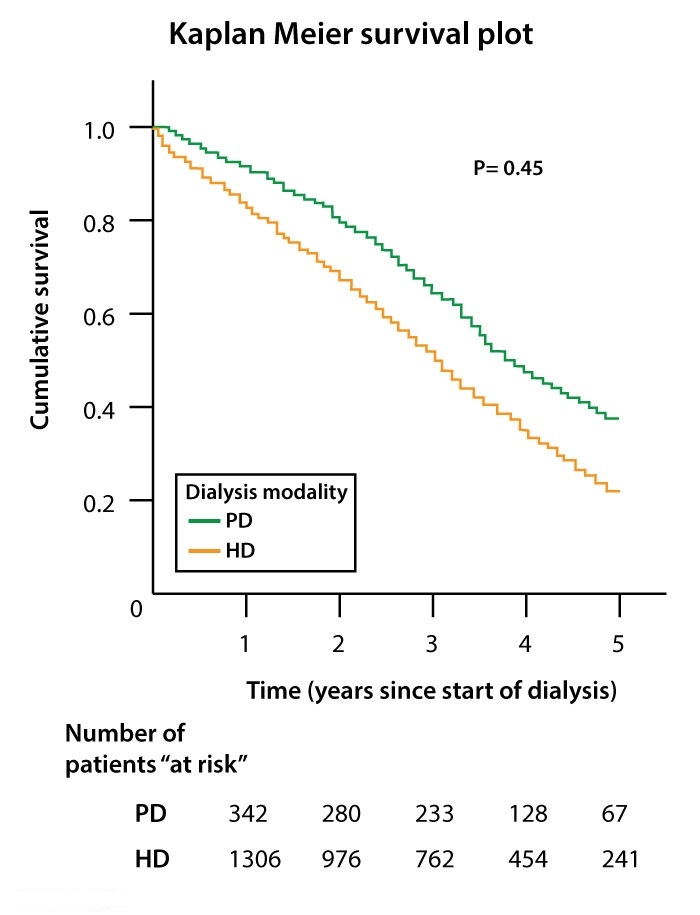 Based on the findings of this study, which dialysis option offers improved survival?
Based on the findings of this study, which dialysis option offers improved survival?A)HD, as median survival was greater than for PD
B)HD, as survival was greater at end of study than for PD
C)HD or PD, as survival was not significantly different
D)PD, as median survival was greater than for HD
E)PD, as survival was greater at end of study than for HD

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
32
A randomized controlled trial is conducted to evaluate the safety and efficacy of monotherapy with a new disease-modifying antirheumatic drug (DMARD) after switching from methotrexate versus continuing methotrexate in patients with inadequate response to methotrexate. The study enrolled adults (age ≥18) who fulfilled the American College of Rheumatology (ACR)-European League Against Rheumatism (EULAR) classification criteria for rheumatoid arthritis. The investigators defined monotherapy with the new DMARD as effective if the treatment resulted in a 20% improvement in the ACR criteria (ACR20) at week 14. In designing the study, the researchers set the probability of wrongly finding that DMARD monotherapy after switching from methotrexate is more effective than continuing methotrexate as 1%, and they set the probability of wrongly finding that the effectiveness of the two therapies is the same as 5%. Which of the following is the most accurate estimate of the statistical power in this study?
A)1%
B)5%
C)20%
D)95%
E)99%
A)1%
B)5%
C)20%
D)95%
E)99%

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
33
A study evaluated predictors of adverse outcomes in geriatric patients admitted to the hospital with a hip fracture requiring surgery. The study compared an old multidimensional score (Model 1) with a new classification system (Model 2). The following results were reported: 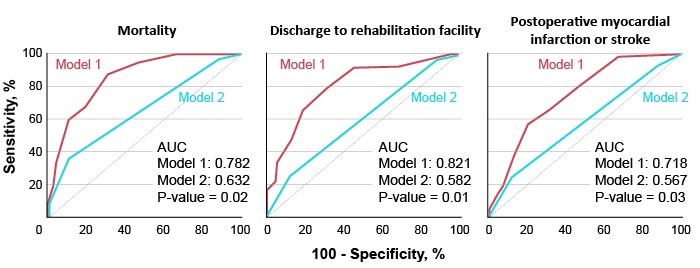 AUC = area under the curve
AUC = area under the curve
Which of the following is the best statement about the study results?
A)Model 1 is less sensitive than Model 2 in predicting discharge to rehabilitation facility
B)Model 1 outperforms Model 2 for mortality, discharge to rehabilitation facility, and postoperative myocardial infarction or stroke
C)Model 1 outperforms Model 2 for mortality only
D)Model 1 predicts postoperative myocardial infarction or stroke more accurately than mortality
E)Model 2 should not be used in clinical practice
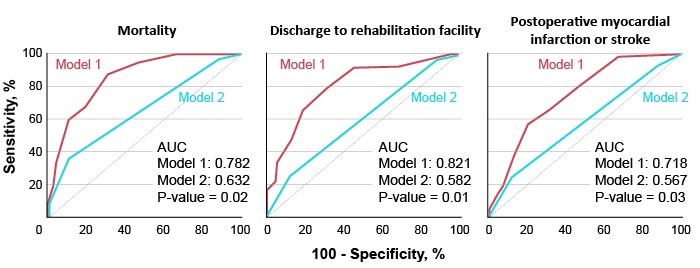 AUC = area under the curve
AUC = area under the curveWhich of the following is the best statement about the study results?
A)Model 1 is less sensitive than Model 2 in predicting discharge to rehabilitation facility
B)Model 1 outperforms Model 2 for mortality, discharge to rehabilitation facility, and postoperative myocardial infarction or stroke
C)Model 1 outperforms Model 2 for mortality only
D)Model 1 predicts postoperative myocardial infarction or stroke more accurately than mortality
E)Model 2 should not be used in clinical practice

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
34
A case-control study evaluated the association between long-term use of a heartburn medication and bladder and colon cancer. The study enrolled 130 patients with bladder cancer, 130 patients with colon cancer, and 230 patients matched by age and sex with no history of cancer. All study participants were interviewed and their medical records reviewed for past long-term use of the heartburn medication. Long-term use of the heartburn medication was found in 30 (23.1%) patients with bladder cancer, in 28 (21.5%) patients with colon cancer, and in 30 (13.0%) patients with no history of cancer. Based on these results, which of the following is the closest interpretation of the odds ratio (OR) of long-term use of the heartburn medication in patients with bladder cancer relative to patients with no history of cancer?
A)Equal odds of long-term use of heartburn medication in both groups, with OR = 1
B)Higher odds among patients with history of bladder cancer, with OR = 1.5
C)Higher odds among patients with history of bladder cancer, with OR = 2.0
D)Lower odds among patients with history of bladder cancer, with OR = 0.25
E)Lower odds among patients with history of bladder cancer, with OR = 0.5
A)Equal odds of long-term use of heartburn medication in both groups, with OR = 1
B)Higher odds among patients with history of bladder cancer, with OR = 1.5
C)Higher odds among patients with history of bladder cancer, with OR = 2.0
D)Lower odds among patients with history of bladder cancer, with OR = 0.25
E)Lower odds among patients with history of bladder cancer, with OR = 0.5

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
35
As part of a study on treatment of uncomplicated cellulitis, outpatients age >12 seeking care at the emergency department with cellulitis and no wound, purulent drainage, or abscess were randomly assigned to either cephalexin plus trimethoprim-sulfamethoxazole for 7 days (n = 85) or cephalexin plus placebo for 7 days (n = 87). The primary outcome was clinical cure, defined as absence of fever and more than minimal erythema, swelling, or tenderness (days 14-21). A total of 24 patients in the cephalexin plus trimethoprim-sulfamethoxazole group and 18 patients in the cephalexin plus placebo group did not complete treatment as prescribed or failed to complete the test-of-clinical-cure visit; they were categorized as noncompliant patients. The principal investigator of the study wanted to conduct a per-protocol analysis of the data. Which of the following describes how the data pertaining to noncompliance should be treated to conduct such an analysis?
A)Conduct separate analyses for compliant and noncompliant participants
B)Exclude the 18 noncompliant participants in the placebo group from analysis
C)Exclude the 24 noncompliant participants in the trimethoprim-sulfamethoxazole group from analysis
D)Exclude the 42 noncompliant participants from analysis
E)Keep all 42 noncompliant participants in their respective groups for analysis
A)Conduct separate analyses for compliant and noncompliant participants
B)Exclude the 18 noncompliant participants in the placebo group from analysis
C)Exclude the 24 noncompliant participants in the trimethoprim-sulfamethoxazole group from analysis
D)Exclude the 42 noncompliant participants from analysis
E)Keep all 42 noncompliant participants in their respective groups for analysis

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
36
A study examined the role of a humanized monoclonal antibody (mAb) that binds soluble forms of amyloid in treating Alzheimer disease. Patients were randomly assigned to a mAb injection or placebo group for 14 months. The outcomes included changes in cognitive performance assessed by different scores at week 72 compared to baseline. Higher scores indicate worse impairment. The following numbers were reported for patients with mild and moderate Alzheimer disease. 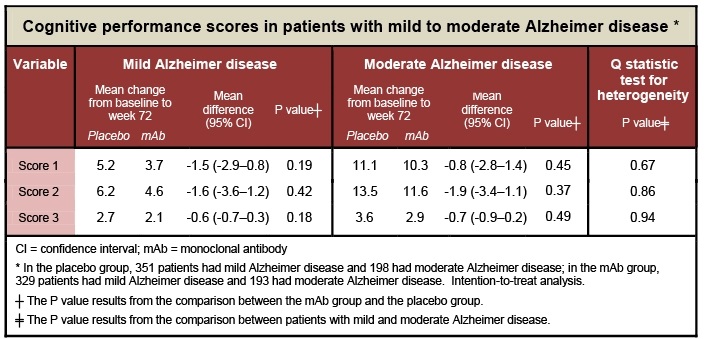 Which of the following is the most accurate interpretation of these study results?
Which of the following is the most accurate interpretation of these study results?
A)mAb therapy effectively slowed the process of mild and moderate Alzheimer disease
B)mAb therapy was more effective in patients with mild Alzheimer disease
C)mAb therapy was more effective in patients with moderate Alzheimer disease
D)Patients with mild Alzheimer disease had a sharper decline in all cognitive performance scores
E)There was no differential response to mAb therapy depending on Alzheimer disease severity
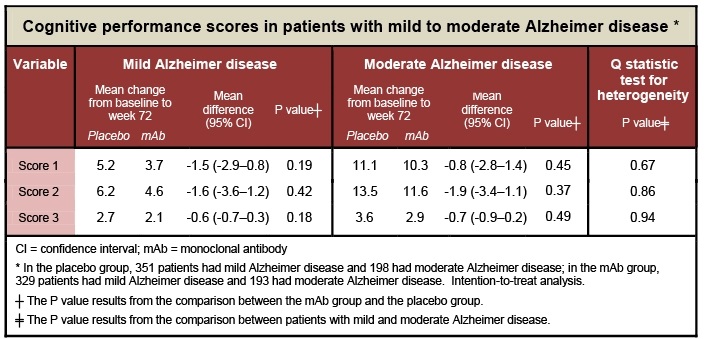 Which of the following is the most accurate interpretation of these study results?
Which of the following is the most accurate interpretation of these study results?A)mAb therapy effectively slowed the process of mild and moderate Alzheimer disease
B)mAb therapy was more effective in patients with mild Alzheimer disease
C)mAb therapy was more effective in patients with moderate Alzheimer disease
D)Patients with mild Alzheimer disease had a sharper decline in all cognitive performance scores
E)There was no differential response to mAb therapy depending on Alzheimer disease severity

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
37
A group of cardiologists hypothesized that a new ACE inhibitor improves outcomes among patients with left ventricular dysfunction whether they have heart failure or not. The cardiologists assessed the role of the new ACE inhibitor in patients who were at high risk for cardiovascular events but who did not have left ventricular dysfunction or heart failure. A total of 8,560 high-risk patients (age ≥55) with evidence of vascular disease or diabetes plus one other cardiovascular risk factor but with no known history of heart failure were randomly assigned at a ratio of 1:1 to receive the new ACE inhibitor or placebo for a mean of 5 years. The primary outcome was death from cardiovascular causes. A total of 261 patients assigned to receive the new ACE inhibitor (6.1%) died from cardiovascular causes, compared to 346 patients assigned to receive placebo (8.1% percent) (relative risk = 0.75; p < 0.05). Which of the following conclusions can be drawn from these results?
A)A 95% confidence interval for the relative risk reported by the study would exclude the null value
B)The new ACE inhibitor reduced the rate of death from cardiovascular causes by 75%
C)The rate of death from cardiovascular causes was 25% higher among patients assigned to placebo
D)The treatment had no effect on the rate of death from cardiovascular causes
A)A 95% confidence interval for the relative risk reported by the study would exclude the null value
B)The new ACE inhibitor reduced the rate of death from cardiovascular causes by 75%
C)The rate of death from cardiovascular causes was 25% higher among patients assigned to placebo
D)The treatment had no effect on the rate of death from cardiovascular causes

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
38
A study evaluated the accuracy of using midstream urine (MSU) culture to identify the causative pathogen in patients with uncomplicated cystitis. Women ages 18-49 with symptoms of cystitis provided MSU specimens for culture. The investigators also collected urine by means of a urethral catheter for culture, which served as the gold standard for confirming the causative pathogen. Bacterial growth was determined in colony forming units per mL. Correlation coefficients (r) were calculated for several organisms by comparing the logarithm of bacterial growth in urethral catheter specimens to that of bacterial growth in MSU specimens. The following plots were reported: 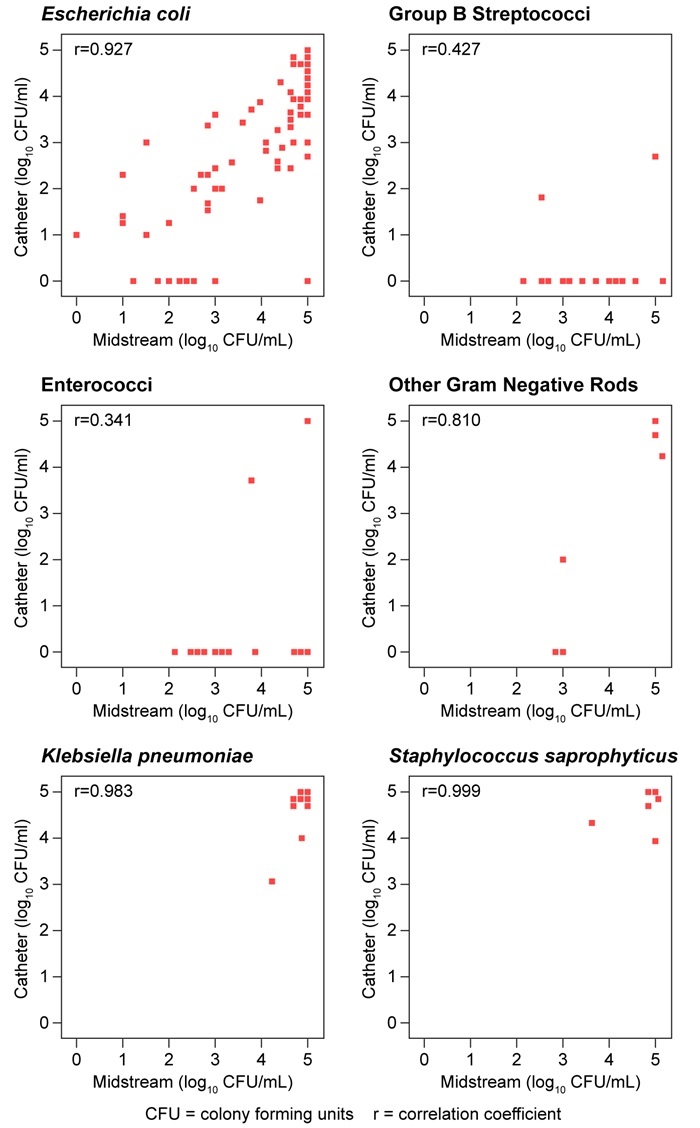 Which of the following organisms identified by MSU most likely has the lowest positive predictive value in revealing the causative pathogen for cystitis?
Which of the following organisms identified by MSU most likely has the lowest positive predictive value in revealing the causative pathogen for cystitis?
A)Enterococci
B)Escherichia coli
C)Group B streptococci
D)Klebsiella pneumoniae
E)Staphylococcus saprophyticus
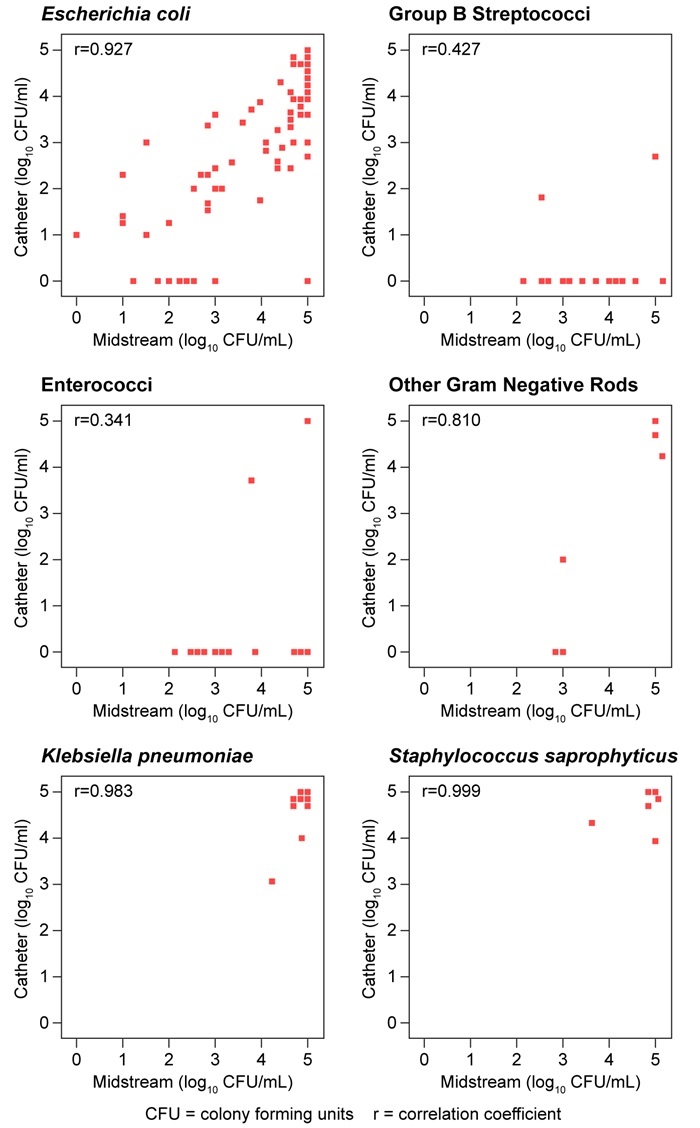 Which of the following organisms identified by MSU most likely has the lowest positive predictive value in revealing the causative pathogen for cystitis?
Which of the following organisms identified by MSU most likely has the lowest positive predictive value in revealing the causative pathogen for cystitis?A)Enterococci
B)Escherichia coli
C)Group B streptococci
D)Klebsiella pneumoniae
E)Staphylococcus saprophyticus

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
39
A 59-year-old man comes to the office for follow-up. He has a history of hypertension for which he takes 2 antihypertensive agents. The patient has no other cardiovascular problems and does not smoke. On examination, his blood pressure is 145/90 mm Hg and BMI is 25.4 kg/m2. The remainder of the examination is unremarkable. Laboratory studies show elevated fasting lipid levels, including LDL cholesterol. His 10-year risk of cardiovascular events is calculated as 10%, and a discussion regarding moderate or intensive statin therapy is initiated. The patient has read that statins may cause diabetes and asks if there is an even more increased risk with intensive compared to moderate statin therapy.
Based on the abstract results with regard to incident diabetes, what is the approximate number needed to harm over 1 year for intensive compared to moderate statin therapy?
A)2
B)7
C)50
D)140
E)500
Based on the abstract results with regard to incident diabetes, what is the approximate number needed to harm over 1 year for intensive compared to moderate statin therapy?
A)2
B)7
C)50
D)140
E)500

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
40
A study of patients with metastatic renal cell carcinoma (RCC) compared the effectiveness of standard chemotherapy to a novel tyrosine kinase inhibitor (TKI) with activity against vascular endothelial growth factor in progression-free survival (primary end point) as first-line treatment. Tumor response was significant in both groups at final follow-up (p < 0.05). The Kaplan-Meier survival curve for overall survival is shown below. 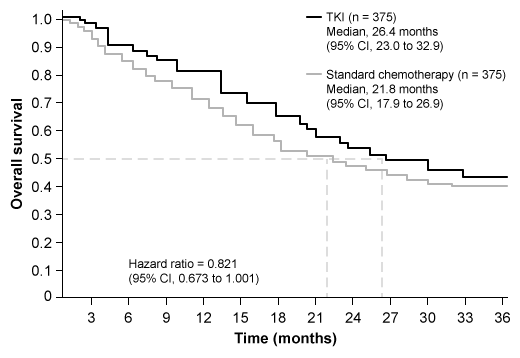 Treatment-related adverse events such as diarrhea, nausea, vomiting, hypertension, hand-foot syndrome, asthenia, leukopenia, neutropenia, thrombocytopenia, lymphopenia, and increased lipase and uric acid occurred more frequently in the TKI group than in the standard chemotherapy group (p < 0.05). Based on the findings of this study, which of the following conclusions is justified?
Treatment-related adverse events such as diarrhea, nausea, vomiting, hypertension, hand-foot syndrome, asthenia, leukopenia, neutropenia, thrombocytopenia, lymphopenia, and increased lipase and uric acid occurred more frequently in the TKI group than in the standard chemotherapy group (p < 0.05). Based on the findings of this study, which of the following conclusions is justified?
A)Either treatment can be recommended because there is no significant difference in outcomes between the 2 groups
B)Neither treatment should be recommended because there is no significant difference in outcomes between groups
C)Standard chemotherapy should be recommended because it is associated with lower rates of treatment-related adverse events
D)TKI therapy should be recommended because its use resulted in longer overall survival estimates
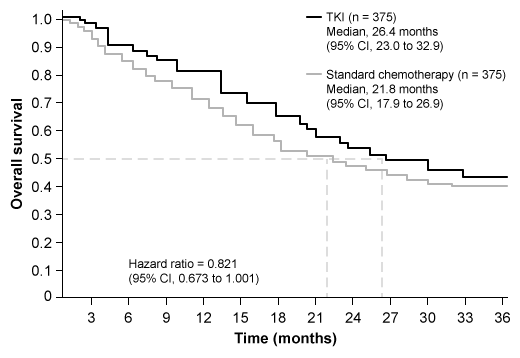 Treatment-related adverse events such as diarrhea, nausea, vomiting, hypertension, hand-foot syndrome, asthenia, leukopenia, neutropenia, thrombocytopenia, lymphopenia, and increased lipase and uric acid occurred more frequently in the TKI group than in the standard chemotherapy group (p < 0.05). Based on the findings of this study, which of the following conclusions is justified?
Treatment-related adverse events such as diarrhea, nausea, vomiting, hypertension, hand-foot syndrome, asthenia, leukopenia, neutropenia, thrombocytopenia, lymphopenia, and increased lipase and uric acid occurred more frequently in the TKI group than in the standard chemotherapy group (p < 0.05). Based on the findings of this study, which of the following conclusions is justified?A)Either treatment can be recommended because there is no significant difference in outcomes between the 2 groups
B)Neither treatment should be recommended because there is no significant difference in outcomes between groups
C)Standard chemotherapy should be recommended because it is associated with lower rates of treatment-related adverse events
D)TKI therapy should be recommended because its use resulted in longer overall survival estimates

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
41
A biomedical research company creates 2 similar real-time, nondestructive cancer diagnostic devices (X and Y) in the form of a pen. The pens are applied to the tissue surface for a few seconds, during which time each pen releases a single water droplet onto the tissue. The water droplet, which picks up small biomolecules from the tissue, is then sucked back into the pen and transferred via tubing to a mass spectrometer. The spectrometer performs a quick molecular analysis and determines whether the tissue is normal (noncancerous) or abnormal (cancerous). The devices allow surgeons to know which tissue to remove and which not to remove. The performance of Devices X and Y was compared using the same samples of tissue. The biomedical research company reported that, compared to Device Y, Device X is better at identifying cancerous tissue as abnormal but worse at identifying noncancerous tissue as normal. Based on this information, which of the following conclusions about the diagnostic devices must be true?
A)Device X has a higher accuracy than Device Y
B)Device X has a higher false-positive rate than Device Y
C)Device X has a higher positive predictive value than Device Y
D)Device X has a higher specificity than Device Y
E)There is not enough information to draw a conclusion
A)Device X has a higher accuracy than Device Y
B)Device X has a higher false-positive rate than Device Y
C)Device X has a higher positive predictive value than Device Y
D)Device X has a higher specificity than Device Y
E)There is not enough information to draw a conclusion

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
42
A 68-year-old man is hospitalized after coronary artery bypass grafting surgery. The patient has a history of coronary artery disease treated with stenting of the right coronary artery several years ago. Medical history also includes hypertension, type 2 diabetes mellitus, and hypercholesterolemia. Over the past 6 months, the patient has had worsening angina, and cardiac catheterization revealed 80% stenosis of the left main artery and restenosis of the right coronary artery. Echocardiography showed a left ventricular ejection fraction of 40% with no valvular abnormalities. A 2-vessel coronary artery bypass grafting with a left internal mammary to the left anterior descending artery and a saphenous vein graft to the right coronary artery was performed. The intraoperative course was uncomplicated, and the patient was extubated 24 hours later. On the third postoperative day, the patient developed atrial fibrillation. He is hemodynamically stable with adequate urine output and good control of the postoperative pain. Serum electrolytes are within normal limits. The patient becomes concerned about the postoperative arrhythmia. Which of the following is the most accurate statement about this patient's atrial fibrillation?
A)It is likely due to reperfusion and intravenous magnesium should help.
B)It is likely ischemia related and further testing is needed to ensure graft patency.
C)It is likely to resolve only with cardioversion and there is low risk of recurrence.
D)It is likely to spontaneously convert to sinus rhythm within a few days.
E)It is unlikely to cause significant postoperative complications.
A)It is likely due to reperfusion and intravenous magnesium should help.
B)It is likely ischemia related and further testing is needed to ensure graft patency.
C)It is likely to resolve only with cardioversion and there is low risk of recurrence.
D)It is likely to spontaneously convert to sinus rhythm within a few days.
E)It is unlikely to cause significant postoperative complications.

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
43
A 74-year-old hospitalized woman is seen for preoperative medical evaluation. The patient was admitted due to a right ankle injury after stepping off a curb and falling. She did not hit her head or lose consciousness during the event. The patient has had no recent chest pain, dyspnea, palpitation, or syncope. Prior to the injury, she was able to walk 1-2 blocks on a flat level and climb a flight of stairs without difficulty. Medical history is significant for hypertension, paroxysmal atrial fibrillation, osteoporosis, and mild cognitive impairment. Medications are amlodipine, metoprolol, rivaroxaban, alendronate, and vitamin D supplements. The patient does not use tobacco, alcohol, or illicit drugs. Blood pressure is 136/88 mm Hg and pulse is 88/min and irregular. Physical examination shows clear lungs and no heart murmurs. Right ankle x-rays reveal a bimalleolar fracture. ECG shows atrial fibrillation with normal ventricular rate. Blood cell count, serum chemistry studies, prothrombin time, and activated partial thromboplastin time are within normal limits. Orthopedic consultation has been obtained, and an operative repair of the fracture is planned in the next 48 hours. In addition to rivaroxaban discontinuation, which of the following is the most appropriate preoperative recommendation regarding this patient's arrhythmia?
A)Begin bridging heparin and postpone surgery for 5 days
B)Perform external electrical cardioversion
C)Proceed with surgery with no additional intervention
D)Stop metoprolol and administer flecainide
E)Switch metoprolol to amiodarone
A)Begin bridging heparin and postpone surgery for 5 days
B)Perform external electrical cardioversion
C)Proceed with surgery with no additional intervention
D)Stop metoprolol and administer flecainide
E)Switch metoprolol to amiodarone

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
44
A 68-year-old man comes to the emergency department due to 12 hours of worsening abdominal pain, nausea, and vomiting. The patient has had intermittent abdominal discomfort and nausea over the past several months but not to this severity. He has had no diarrhea, and his most recent bowel movement was 1 day ago. The patient has no known medical conditions and takes no medications. He has smoked a pack of cigarettes daily for 30 years and drinks 1 or 2 alcoholic beverages daily. Temperature is 38.5 C (101.3 F), blood pressure is 106/64 mm Hg, pulse is 112/min, and respirations are 18/min. On physical examination, the patient appears to be in discomfort and is diaphoretic. The abdomen is tender and rigid throughout. Bowel sounds are absent. Abdominal imaging shows free air under the diaphragm. Intravenous fluids and empiric antibiotics are started, and surgical consultation is obtained. While being prepared for laparotomy, the patient develops new-onset atrial fibrillation with a ventricular rate of 118/min. The patient reports no palpitations, chest pain, or dyspnea. Blood pressure is 110/70 mm Hg. Which of the following is the best next step in management of this patient?
A)Achieve a ventricular rate <90/min prior to surgery using digoxin therapy
B)Achieve sinus rhythm prior to surgery using flecainide therapy
C)Achieve sinus rhythm prior to surgery using transesophageal echocardiography-guided electrical cardioversion
D)Administer a beta blocker for rate control and proceed with surgery without other intervention
E)Obtain transthoracic echocardiography and proceed with surgery only if there are no abnormalities
A)Achieve a ventricular rate <90/min prior to surgery using digoxin therapy
B)Achieve sinus rhythm prior to surgery using flecainide therapy
C)Achieve sinus rhythm prior to surgery using transesophageal echocardiography-guided electrical cardioversion
D)Administer a beta blocker for rate control and proceed with surgery without other intervention
E)Obtain transthoracic echocardiography and proceed with surgery only if there are no abnormalities

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
45
A 76-year-old man is admitted to the hospital with nausea, vomiting, and generalized abdominal distension. He has a long-standing history of type 2 diabetes mellitus. His medical follow-up has been poor. Physical examination and diagnostic workup are consistent with a complicated small-bowel obstruction. He undergoes exploratory laparotomy with no operative complications and is extubated postoperatively in the surgical intensive care unit. A few hours after extubation, the patient experiences sudden onset of chest discomfort, nausea, and marked diaphoresis. Temperature is 36.1 C (97 F), blood pressure is 84/50 mm Hg, pulse is 32/min, and respirations are 26/min. Examination shows minimal crackles at both bases. There are no murmurs on cardiac examination. Fingerstick glucose level is 150 mg/dL. ECG shows sinus bradycardia with 3-mm ST-segment elevations in leads II, III, and aVF. Immediate chest x-ray shows increased interstitial markings bilaterally. Intravenous normal saline infusion is started and intravenous atropine is administered without significant improvement. Which of the following is the most appropriate next step in management of this patient?
A)Intravenous heparin infusion
B)Low-dose dobutamine infusion
C)Norepinephrine infusion
D)Temporary cardiac pacing
E)Thrombolytic therapy
A)Intravenous heparin infusion
B)Low-dose dobutamine infusion
C)Norepinephrine infusion
D)Temporary cardiac pacing
E)Thrombolytic therapy

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
46
A 65-year-old man is brought to the emergency department with a 2-hour history of sharp, stabbing chest pain under his sternum. The patient was working outside in the yard when the symptoms started. The pain reached its maximum intensity within a few minutes and is now radiating to his upper back and shoulders. His medical history is significant for hypertension for the past 10 years. The patient has smoked 1.5 packs of cigarettes daily for the last 40 years. Blood pressure is 185/104 mm Hg in the right arm and 120/62 mm Hg in the left arm, pulse is 106/min and regular, and respirations are 18/min. Lungs are clear to auscultation bilaterally. Cardiovascular examination reveals a regular heart rhythm with an early diastolic murmur heard at the right sternal border. ECG shows sinus tachycardia and T-wave inversion in leads V5 and V6. Bedside transesophageal echocardiogram in the emergency department confirms ascending aortic dissection with extension into the left subclavian artery. In addition to pain control, what is the best next step in management of this patient?
A)Aspirin
B)Eptifibatide
C)Esmolol
D)Hydralazine
E)Sodium nitroprusside
A)Aspirin
B)Eptifibatide
C)Esmolol
D)Hydralazine
E)Sodium nitroprusside

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
47
A 60-year-old man is found to have an incidental 3.5-cm abdominal aortic aneurysm on an imaging study. He has no associated symptoms. Past medical history is significant for hypertension, type 2 diabetes, hypercholesterolemia, and hypothyroidism. His medications include aspirin, metformin, glipizide, chlorthalidone, lisinopril, atorvastatin, and levothyroxine. The patient has a 40-pack-year smoking history and continues to smoke 1-2 packs a day. He drinks 3 or 4 glasses of wine daily. His blood pressure is 160/90 mm Hg and pulse is 80/min. Cardiopulmonary examination is within normal limits. Laboratory results are as follows: 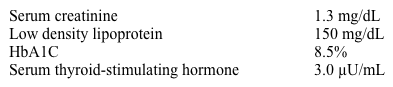 Which of the following interventions would most decrease the likelihood of expansion of this patient's aortic aneurysm?
Which of the following interventions would most decrease the likelihood of expansion of this patient's aortic aneurysm?
A)Aggressive diabetes management
B)Improved blood pressure control
C)Moderation of alcohol intake
D)Optimized hyperlipidemia treatment
E)Smoking cessation
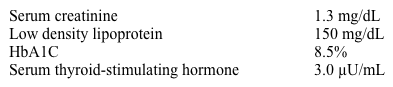 Which of the following interventions would most decrease the likelihood of expansion of this patient's aortic aneurysm?
Which of the following interventions would most decrease the likelihood of expansion of this patient's aortic aneurysm?A)Aggressive diabetes management
B)Improved blood pressure control
C)Moderation of alcohol intake
D)Optimized hyperlipidemia treatment
E)Smoking cessation

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
48
A 33-year-old, previously healthy woman is brought to the emergency department in severe respiratory distress. The patient's shortness of breath began abruptly 2 days ago and has progressively worsened. Over the past 6 months she has had loss of appetite, loose stools, and lightheadedness. Temperature is 38.6 C (101.5 F), blood pressure is 178/102 mm Hg, pulse is 120/min, and respirations are 38/min. Pulse oximetry is 86% on nonrebreather mask. Examination shows marked respiratory distress with intercostal and supraclavicular retractions. The skin is diaphoretic and warm. Cardiopulmonary examination reveals diffuse rales, an S3, and a 2/6 systolic ejection murmur over the left sternal border. The extremities have 1+ pitting edema bilaterally. The patient is placed on positive airway pressure ventilation with improvement in oxygen saturation to 94%. ECG shows sinus tachycardia. Chest x-ray reveals a mildly enlarged cardiac silhouette with pulmonary vascular congestion. Echocardiography shows pulmonary hypertension, left atrial enlargement, and a left ventricular ejection fraction of 75%; there are no wall motion abnormalities. Troponin I is 0.06 ng/mL (normal: <0.04 ng/mL). Which of the following is the most appropriate diagnostic step in management of this patient?
A)Antinuclear antibodies
B)Coronary angiography
C)CT pulmonary angiography
D)Serum TSH
E)Viral antibody titers
A)Antinuclear antibodies
B)Coronary angiography
C)CT pulmonary angiography
D)Serum TSH
E)Viral antibody titers

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
49
A 55-year-old man comes to the emergency department due to sudden onset of retrosternal chest pain. The pain began 10 hours ago and has been mostly constant, although he describes it as "being bad and then getting a little better." The patient has had no lightheadedness, syncope, or shortness of breath. ECG shows normal sinus rhythm with 2-mm ST-segment elevation in leads V2 to V5. He is taken emergently for cardiac catheterization and undergoes percutaneous coronary intervention with stent placement to the left anterior descending artery. After the procedure, the ST-segment changes improve and he has complete resolution of the chest pain. On the third night, just prior to discharge, he calls for the nurse due to the sudden onset of sharp, retrosternal chest pain. The patient first noticed the pain while turning around in bed; it worsens with deep breathing. Temperature is 37.8 C (100 F), blood pressure is 134/80 mm Hg, heart rate is 108/min, and respirations are 22/min. Physical examination reveals regular heart sounds and clear lung fields. There is a scratchy sound heard during ventricular systole along the left sternal border. Abdominal palpation reveals no localized tenderness. ECG shows sinus tachycardia with Q waves and T-wave inversion in leads V2 to V5.
Which of the following is the most likely cause of this patient's recurrent symptoms?
A)Acute myocardial infarction
B)Acute pericarditis
C)Dressler syndrome
D)Left ventricular aneurysm
E)Recurrent myocardial ischemia
Which of the following is the most likely cause of this patient's recurrent symptoms?
A)Acute myocardial infarction
B)Acute pericarditis
C)Dressler syndrome
D)Left ventricular aneurysm
E)Recurrent myocardial ischemia

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
50
An 11-month-old girl is brought to the pediatrician by her parents for a follow-up visit. The patient was recently diagnosed with a rare multisystemic syndromic disorder characterized by cognitive impairment, deafness, skeletal abnormalities, and coarse facial features. The disorder occurs in ~1 in 100,000 births, and the underlying cause is unknown. The parents ask about factors that may have contributed to the development of the rare disorder. Which of the following types of study designs would be most appropriate to address the parents' question?
A)Case-control study
B)Case report
C)Case series
D)Cohort study
E)Cross-sectional study
A)Case-control study
B)Case report
C)Case series
D)Cohort study
E)Cross-sectional study

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
51
A 66-year-old woman with systolic left ventricular dysfunction comes to the emergency department due to dizziness, palpitations, and shortness of breath. The symptoms started 2 days ago and have become progressively worse. Her cardiologist prescribed an extra dose of oral furosemide yesterday, but her symptoms did not improve. Six weeks ago, she was admitted for acute decompensated heart failure that was thought to be precipitated by atrial fibrillation. The patient underwent electrical cardioversion and was diuresed with marked symptomatic improvement. She has a history of atrial fibrillation, hypertension, type 2 diabetes mellitus, coronary artery disease, ischemic cardiomyopathy with a 30% ejection fraction, and osteoarthritis. She underwent coronary artery bypass grafting 5 years ago. Her current medications include low-dose aspirin, metoprolol, lisinopril, rosuvastatin, long-acting insulin, rivaroxaban, furosemide, and ibuprofen as needed. The patient has been adherent to her medical regimen. She does not use tobacco or alcohol. Temperature is 36.7 C (98 F), blood pressure is 126/82 mm Hg, pulse is 132/min and irregular, and respirations are 19/min. Physical examination reveals bibasilar crackles on auscultation. There are irregularly irregular heart sounds with no audible murmurs. There is 1+ symmetric peripheral edema. ECG shows atrial fibrillation with rapid ventricular response. Serum creatinine level is 0.8 mg/dL. After initial treatment, electrical cardioversion is planned. Which of the following is the most appropriate medication for long-term management of this patient?
A)Amiodarone
B)Flecainide
C)Ranolazine
D)Valsartan
E)Verapamil
A)Amiodarone
B)Flecainide
C)Ranolazine
D)Valsartan
E)Verapamil

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
52
A 55-year-old man comes to the emergency department due to sudden onset of retrosternal chest pain. The pain began 10 hours ago and has been mostly constant, although he describes it as "being bad and then getting a little better." The patient has had no lightheadedness, syncope, or shortness of breath. ECG shows normal sinus rhythm with 2-mm ST-segment elevation in leads V2 to V5. He is taken emergently for cardiac catheterization and undergoes percutaneous coronary intervention with stent placement to the left anterior descending artery. After the procedure, the ST-segment changes improve and he has complete resolution of the chest pain. On the third night, just prior to discharge, he calls for the nurse due to the sudden onset of sharp, retrosternal chest pain. The patient first noticed the pain while turning around in bed; it worsens with deep breathing. Temperature is 37.8 C (100 F), blood pressure is 134/80 mm Hg, heart rate is 108/min, and respirations are 22/min. Physical examination reveals regular heart sounds and clear lung fields. There is a scratchy sound heard during ventricular systole along the left sternal border. Abdominal palpation reveals no localized tenderness. ECG shows sinus tachycardia with Q waves and T-wave inversion in leads V2 to V5. Which of the following is the most appropriate next step in management of this patient?
A)High-dose aspirin
B)Immediate cardiothoracic surgical referral
C)Naproxen plus colchicine
D)Oral glucocorticoids
E)Urgent cardiac catheterization
A)High-dose aspirin
B)Immediate cardiothoracic surgical referral
C)Naproxen plus colchicine
D)Oral glucocorticoids
E)Urgent cardiac catheterization

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
53
A 70-year-old man is brought to the emergency department by his wife after an episode of syncope while working in his garden. He regained consciousness immediately and initially refused to go to the hospital saying, "I feel fine." The patient has never experienced syncope before. According to his wife, he has always been physically active but lately has had increased fatigability; he seems to work less in the garden and spends more time indoors watching television. Medical history is significant for type 2 diabetes mellitus and gout. His only current medication is metformin. He is a lifetime nonsmoker and does not drink alcohol. Blood pressure is 100/80 mm Hg and pulse is 90/min. BMI is 28 kg/m2. Both carotid pulses are delayed. Lungs are clear on auscultation. A harsh crescendo-decrescendo murmur is heard at the base of the heart. The second heart sound is soft with an inaudible A2 component. There is no peripheral edema. ECG shows normal sinus rhythm, left ventricular hypertrophy, and secondary ST-segment and T-wave changes. Echocardiography shows concentric left ventricular hypertrophy with severe calcification of the aortic valve. The estimated aortic valve area is 0.78 cm2 and the mean transvalvular gradient is 50 mm Hg. Laboratory studies show normal complete blood count and serum creatinine of 0.8 mg/dL. Which of the following is the best statement about this patient's condition?
A)Aortic valve replacement is associated with marked reduction in mortality
B)Balloon valvulotomy is preferred due to better long-term prognosis
C)Balloon valvulotomy is preferred due to low procedural morbidity
D)Conservative treatment should be tried before offering an intervention
E)The patient's onset of symptoms has minimal bearing on his prognosis
A)Aortic valve replacement is associated with marked reduction in mortality
B)Balloon valvulotomy is preferred due to better long-term prognosis
C)Balloon valvulotomy is preferred due to low procedural morbidity
D)Conservative treatment should be tried before offering an intervention
E)The patient's onset of symptoms has minimal bearing on his prognosis

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
54
A 44-year-old man comes to the urgent care clinic due to palpitations. The current episode started 2 hours ago and feels like "fluttering in the chest." He has no chest pain, orthopnea, dizziness, syncope, or shortness of breath. The patient has had similar episodes in the past 6 months, but they usually last less than an hour and resolve spontaneously. He cannot identify any clear-cut precipitating factor for these episodes. He has a history of migraines and kidney stones. The patient does not use tobacco, alcohol, or illicit drugs. His family history is significant for liver cancer and renal failure. He works in an office and his lifestyle is mainly sedentary. On initial evaluation, he appears comfortable. Blood pressure is 124/82 mm Hg and pulse is 122/min. Oxygen saturation is 99% on room air. BMI is 31 kg/m2. Cardiac auscultation reveals no murmurs. The patient's lungs are clear to auscultation and there is no peripheral edema. ECG shows atrial fibrillation with a rapid ventricular response. Complete blood count, basic metabolic panel, TSH level, and chest x-ray are normal. A transthoracic echocardiogram shows normal left ventricular size and function, mild enlargement of the left atrium, and no valvular abnormalities. The patient is given oral metoprolol and reports improvement of his symptoms after 2 hours. Repeat ECG shows normal sinus rhythm with a ventricular rate of 77/min at rest. There are no repolarization abnormalities and his QTc interval is 410 msec. In addition to oral metoprolol, which of the following is the most appropriate therapy for this patient?
A)Amiodarone
B)Anticoagulation
C)Digoxin
D)Diltiazem
E)Periodic follow-up only
A)Amiodarone
B)Anticoagulation
C)Digoxin
D)Diltiazem
E)Periodic follow-up only

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
55
A 6-year-old boy is brought to the office by his mother for an annual physical examination. He has had no recent illnesses but has had intermittent pain in his legs during his soccer games for the past 3 months. The patient had no trauma preceding the onset of leg pain, has no numbness or tingling, and is able to walk without a limp. He was born at 38 weeks gestation via a spontaneous vaginal delivery with no complications. The patient has met all developmental milestones, and all of his immunizations are up to date. His father was recently diagnosed with hypertension at age 55, but there is no other significant family history. Temperature is 36.1 C (97 F), blood pressure is 135/88 mm Hg in the right upper extremity, pulse is 110/min, respirations are 24/min, and pulse oximetry is 98% on room air. Weight and height are at the 25th and 50th percentiles, respectively, for age. Physical examination shows a well-appearing boy who has no dysmorphic features and who smiles and fully cooperates. The lungs are clear to auscultation. Heart rate and rhythm are normal. A 2/6 continuous murmur is heard over the left interscapular area. The lower extremities have no swelling, erythema, or tenderness. Further evaluation would most likely show which of the following findings?
A)Digital clubbing
B)Hepatomegaly
C)Lower extremity hypotension
D)Parasternal heave
E)Pulsus paradoxus
A)Digital clubbing
B)Hepatomegaly
C)Lower extremity hypotension
D)Parasternal heave
E)Pulsus paradoxus

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
56
A 55-year-old man comes to the emergency department with palpitations that began earlier this morning. He was having tea when he suddenly started to experience fluttering in his chest. He tried walking around and taking deep breaths, but the feeling did not subside. The patient has previously felt his "'heart skipping a beat" but had never sustained palpitations as he did today. He has no lightheadedness, blurry vision, muscle weakness, chest pain, or shortness of breath. The patient has hypertension that is well controlled with valsartan and amlodipine. He does not use tobacco, alcohol, or illicit drugs. He has no drug allergies. His father had a stroke at age 65 and his mother has congestive heart failure. On initial evaluation, the patient appears anxious and in mild discomfort due to palpitations. Blood pressure is 140/80 mm Hg and respirations are 19/min. Jugular venous pressure is estimated at 2 cm H2O. Cardiac auscultation reveals no murmurs. Lungs are clear to auscultation. The abdomen is soft, nontender, and non-distended. Neurologic examination shows no abnormalities. The patient is placed on a telemetry monitor, and a 12-lead ECG is performed. What is the most appropriate next step in management of this patient?
A)Adenosine
B)Amiodarone
C)Clopidogrel
D)Digoxin
E)Metoprolol
A)Adenosine
B)Amiodarone
C)Clopidogrel
D)Digoxin
E)Metoprolol

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
57
A 56-year-old man comes to the emergency department due to chest pain that occurred at home. He was watching television when he developed left-sided chest pain described as dull and pressure-like. The pain progressively worsened and radiated to the throat but spontaneously resolved within 20 minutes. During the past week, the patient had 2 similar episodes with exertion at his job as a construction worker. He has had no palpitations, syncope, shortness of breath, or diaphoresis. He has a history of hypertension treated with lisinopril and is a lifetime nonsmoker. Family history is significant for stroke at a young age in a paternal uncle. The patient is currently free of chest pain and comfortable. Blood pressure is 150/80 mm Hg and pulse is 78/min. Physical examination is otherwise unremarkable. ECG shows sinus rhythm with T-wave inversion in leads V5 and V6. Chest x-ray is normal. Cardiac troponin I level is normal (<0.012 ng/dL). Aspirin, metoprolol, atorvastatin, clopidogrel, and subcutaneous enoxaparin are initiated. Eight hours later, he is still without chest pain. ECG is unchanged and repeat troponin I level is normal. Which of the following is the best next step in management of this patient?
A)Discharge home with prescriptions for aspirin, metoprolol, and atorvastatin
B)Obtain coronary calcium scan
C)Obtain exercise stress test
D)Perform coronary angiography within 24 hours
E)Provide reassurance and discharge home with no new medications
A)Discharge home with prescriptions for aspirin, metoprolol, and atorvastatin
B)Obtain coronary calcium scan
C)Obtain exercise stress test
D)Perform coronary angiography within 24 hours
E)Provide reassurance and discharge home with no new medications

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
58
A 21-year-old man is seen in the clinic for a routine checkup. He is a cyclist and was asked by his trainer to see a physician due to a "slow heartbeat." The patient describes intense physical activity in preparation for tournaments and has no symptoms. Specifically, he has no chest pain, shortness of breath, lightheadedness, presyncope, or syncope. His family history is unremarkable. He does not take any medications or use performance-enhancing drugs. Blood pressure is 123/72 mm Hg and pulse is 46/min. No cardiac murmurs are heard in the supine or upright positions. There are no additional heart sounds. The lungs are clear on auscultation. Pulses are full and symmetric, and there is no peripheral edema. ECG shows sinus bradycardia at 48/min. The PR interval is prolonged at 250 msec, consistent with first-degree atrioventricular block. QRS complexes are normal with no repolarization abnormalities, and QTc interval duration is normal at 400 msec. Which of the following is the best next step in management of this patient?
A)24-hour ECG monitoring
B)Blood testing for performance-enhancing drugs
C)Reassurance and routine care
D)Transthoracic echocardiogram
E)Treadmill exercise testing
A)24-hour ECG monitoring
B)Blood testing for performance-enhancing drugs
C)Reassurance and routine care
D)Transthoracic echocardiogram
E)Treadmill exercise testing

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
59
A 23-year-old man is evaluated for a murmur discovered at a health fair. His past medical history is insignificant, and he feels well with no cardiac symptoms. The patient plays soccer and jogs regularly. His immediate family is healthy. Blood pressure is 122/70 mm Hg and pulse is 72/min. A 2/6 midsystolic murmur is heard at the left sternal border. The femoral pulses are full, and there is no brachial-femoral pulse delay. Echocardiography shows bicuspid aortic valve with a mildly increased gradient and no dilation of the aortic root. Which of the following is the best next step in management of this patient?
A)Angiography to rule out coronary artery anomaly
B)Aortic valve replacement
C)Balloon valvuloplasty
D)Doppler ultrasound for renal artery stenosis
E)First-degree relative screening with echocardiography
A)Angiography to rule out coronary artery anomaly
B)Aortic valve replacement
C)Balloon valvuloplasty
D)Doppler ultrasound for renal artery stenosis
E)First-degree relative screening with echocardiography

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
60
A 74-year-old woman is admitted to the hospital for an episode of paroxysmal atrial fibrillation that caused palpitations and dizziness. She is started on metoprolol and amiodarone. Her past medical history is also significant for recurrent deep venous thrombosis 6 months ago. The patient has been on chronic anticoagulation therapy with a stable dose of warfarin since then. Her primary care physician checks her International Normalized Ratio every month; it is 2.6 at the time of admission. Echocardiogram shows left atrial enlargement and left ventricular ejection fraction of 45%. She feels well the following day and is ready for discharge. Which of the following is the best management for this patient's anticoagulation?
A)Continue current dose of warfarin and recheck International Normalized Ratio in 2 weeks
B)Decrease warfarin dose by 25%
C)Double the dose of warfarin
D)Increase warfarin dose by 25%
E)Stop warfarin and recheck International Normalized Ratio in 1 week
A)Continue current dose of warfarin and recheck International Normalized Ratio in 2 weeks
B)Decrease warfarin dose by 25%
C)Double the dose of warfarin
D)Increase warfarin dose by 25%
E)Stop warfarin and recheck International Normalized Ratio in 1 week

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
61
A 62-year-old woman comes to the physician due to chest and epigastric discomfort over the last 6 months. She feels dull chest pressure while walking uphill at a fast pace. The patient says, "It is unusual. I feel this pressure only once in a while, even when doing the same thing. Sometimes it is worse when I walk fast after a heavy meal." She has a history of nonulcer dyspepsia and acid reflux disease and occasionally takes over-the-counter omeprazole. She has no shortness of breath, palpitations, lightheadedness, lower extremity swelling, or syncope. The patient is physically active and has a very hectic social lifestyle. Medical history includes "borderline" hypertension and anxiety disorder. She stopped taking antihypertensive medications 5 years ago. She is a lifetime nonsmoker. The patient does not use alcohol or illicit drugs. Her mother suffered a stroke at age 70 and her father died of prostate cancer. Blood pressure is 145/90 mm Hg and pulse is 80/min and regular. BMI is 29 kg/m2. No heart murmurs are heard on cardiac auscultation. There are no carotid bruits. The lungs are clear and the rest of the physical examination is unremarkable. Resting ECG shows normal sinus rhythm, normal voltage, and T-wave flattening in leads V5 and V6. Laboratory studies show fasting blood glucose of 102 mg/dL and LDL cholesterol of 110 mg/dL. Which of the following is most appropriate management for this patient's chest pain?
A)Initiate antihypertensive therapy with no diagnostic testing
B)Obtain a dobutamine echocardiogram
C)Obtain an exercise ECG
D)Obtain exercise myocardial perfusion imaging
E)Proceed with coronary angiography
A)Initiate antihypertensive therapy with no diagnostic testing
B)Obtain a dobutamine echocardiogram
C)Obtain an exercise ECG
D)Obtain exercise myocardial perfusion imaging
E)Proceed with coronary angiography

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
62
A 55-year-old man with type 2 diabetes mellitus and hypertension comes to the physician with exertional chest pain over the last 3 months that has worsened recently. He reports chest pain, occasionally accompanied by diaphoresis, after walking one block. His medications include low-dose aspirin, metoprolol, rosuvastatin, insulin detemir, and nitroglycerin as needed. Cardiac catheterization shows proximal left anterior descending artery stenosis of 90%, right coronary artery stenosis of 85%, and left circumflex artery stenosis of 75%. His left ventricular ejection fraction is 45%. His hemoglobin A1C is 7.8% and LDL cholesterol is 110 mg/dL. What is the most appropriate management for this patient?
A)Coronary artery bypass grafting surgery
B)Improvement of glycemic control, ranolazine, and follow-up in 6 months
C)Niacin, amlodipine, and follow-up in 6 months
D)Percutaneous coronary intervention using bare metal stents
E)Percutaneous coronary intervention using drug-eluting stents
A)Coronary artery bypass grafting surgery
B)Improvement of glycemic control, ranolazine, and follow-up in 6 months
C)Niacin, amlodipine, and follow-up in 6 months
D)Percutaneous coronary intervention using bare metal stents
E)Percutaneous coronary intervention using drug-eluting stents

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
63
A 55-year-old woman comes to the office due to exertional dyspnea for 3 months. The patient has had no chest pain. Medical history is significant for hypertension and chronic kidney disease. Medications include furosemide, amlodipine, and lisinopril. The patient has never smoked cigarettes. Temperature is 37 C (98.6 F), blood pressure is 128/80 mm Hg, and pulse is 80/min. Oxygen saturation is 98% on room air. BMI is 27 kg/m2. There is no jugular venous distension. Cardiopulmonary examination is normal. Trace bilateral pedal edema is present. Laboratory studies are as follow: 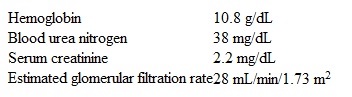 ECG is unremarkable. Chest x-ray reveals clear lung fields. Which of the following is the most appropriate next step in management of this patient?
ECG is unremarkable. Chest x-ray reveals clear lung fields. Which of the following is the most appropriate next step in management of this patient?
A)CT pulmonary angiography
B)Erythropoiesis-stimulating agent
C)Hemodialysis
D)Pulmonary function testing
E)Stress echocardiography
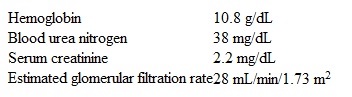 ECG is unremarkable. Chest x-ray reveals clear lung fields. Which of the following is the most appropriate next step in management of this patient?
ECG is unremarkable. Chest x-ray reveals clear lung fields. Which of the following is the most appropriate next step in management of this patient?A)CT pulmonary angiography
B)Erythropoiesis-stimulating agent
C)Hemodialysis
D)Pulmonary function testing
E)Stress echocardiography

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
64
A 32-year-old man is evaluated for syncope. The patient passed out once briefly when playing basketball and experienced no post-syncopal symptoms. Over the last year, he has tired easily and becomes short of breath when climbing 3-4 flights of stairs. The patient takes lansoprazole for acid reflux. In the past, a physician had told him that his blood pressure is "borderline." The patient smokes half a pack of cigarettes a day. His paternal uncle died suddenly at age 30. Blood pressure is 152/90 mm Hg and pulse is 90/min. A 2/6 midsystolic murmur is heard at the left sternal border and accentuates on standing. Lungs are clear to auscultation. Echocardiography shows left atrial enlargement, interventricular septal thickness of 2 cm (normal <1.1 cm), and posterior left ventricular wall thickness of 0.9 cm (normal <1.1 cm). Left ventricular ejection fraction is 75%. There is systolic anterior motion of the mitral valve. At rest, peak instantaneous left ventricular outflow gradient is 30 mm Hg and increases to 45 mm Hg with Valsalva. Which of the following is the most appropriate next step in management of this patient?
A)Alcohol septal ablation
B)Hypertension control with lisinopril
C)Implantable cardioverter-defibrillator
D)Intensive weight loss program
E)Tilt table testing
A)Alcohol septal ablation
B)Hypertension control with lisinopril
C)Implantable cardioverter-defibrillator
D)Intensive weight loss program
E)Tilt table testing

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
65
A 51-year-old man comes to the office for a follow-up visit. He has no concerns. His medical conditions include type 2 diabetes mellitus, hypertension, and obesity. The patient does not use tobacco, alcohol, or illicit drugs. His mother and maternal grandfather also had diabetes. His current medications include aspirin, glyburide, metformin, and lisinopril. Blood pressure is 144/79 mm Hg and pulse is 88/min. Weight is 120 kg (265 lb). Examination shows no abnormalities. Laboratory results are as follows: 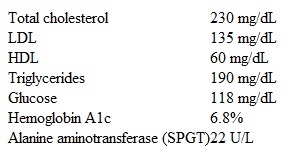 Which of the following is the most appropriate therapy to prevent atherosclerotic cardiovascular disease in this patient?
Which of the following is the most appropriate therapy to prevent atherosclerotic cardiovascular disease in this patient?
A)Exercise alone
B)Gemfibrozil
C)Niacin
D)Orlistat
E)Rosuvastatin
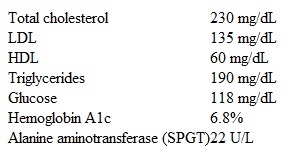 Which of the following is the most appropriate therapy to prevent atherosclerotic cardiovascular disease in this patient?
Which of the following is the most appropriate therapy to prevent atherosclerotic cardiovascular disease in this patient?A)Exercise alone
B)Gemfibrozil
C)Niacin
D)Orlistat
E)Rosuvastatin

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
66
A 76-year-old Caucasian male comes to see you in the office. He complains that he has visible and palpable tortuous swelling on both of his lower legs. It is associated with mild leg heaviness and cramping, especially in the evening. His symptoms are worse with prolonged standing, and improve with leg elevation. He has a past medical history of hypertension, hyperlipidemia, benign prostatic hyperplasia, and degenerative joint disease of both knees. On examination of his lower legs, you notice a few scattered palpable veins consistent with a diagnosis of varicose veins. There is no edema, chronic skin hyperpigmentation, or leg ulcers. Peripheral pulses are full and equal on both sides. Which of the following is the most appropriate next step in the management of this patient?
A)Leg elevation and compression stockings
B)Injection sclerotherapy with saline
C)Injection sclerotherapy with saline and local anesthetic
D)Surgical ligation and stripping
E)External laser therapy
A)Leg elevation and compression stockings
B)Injection sclerotherapy with saline
C)Injection sclerotherapy with saline and local anesthetic
D)Surgical ligation and stripping
E)External laser therapy

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
67
A 63-year-old man with hypertension comes to the clinic for follow-up. He was last seen a year ago and has been maintained on amlodipine for the past 3 years. The patient has no symptoms and describes good exercise tolerance. He takes rosuvastatin for hyperlipidemia. The patient does not use tobacco, alcohol, or illicit drugs. Blood pressure is 132/78 mm Hg, and pulse is 82/min and regular. Oxygen saturation is 99%. Examination reveals a 2/6 ejection-type systolic murmur at the right second intercostal space. The patient's lungs are clear, and there is no peripheral edema. ECG shows normal sinus rhythm with nonspecific T wave abnormalities. He is referred for an echocardiogram, which reveals mild aortic sclerosis and left ventricular dilation with an ejection fraction of 35%. There are no regional wall motion abnormalities. Cardiac stress test is negative for ischemia. Which of the following is the best management for this patient?
A)Initiate angiotensin system inhibitor
B)Initiate digoxin
C)Initiate low-dose diuretic
D)Initiate spironolactone
E)Reassure and follow up in 6 months
A)Initiate angiotensin system inhibitor
B)Initiate digoxin
C)Initiate low-dose diuretic
D)Initiate spironolactone
E)Reassure and follow up in 6 months

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
68
A 62-year-old woman comes to the office due to episodic tightness over her anterior chest for the past 6 months. It sometimes occurs while the patient is walking or climbing stairs, but several episodes have occurred while sitting at her desk at work, which she attributes to stress. The discomfort usually lasts 5-10 minutes and feels like muscle cramps. She has had no shortness of breath, palpitations, lightheadedness, syncope, or lower-extremity swelling. The patient has a history of diet-controlled diabetes mellitus diagnosed 20 years ago and anxiety disorder. She takes low-dose aspirin, lisinopril, and atorvastatin. She is a lifetime nonsmoker and drinks 1 or 2 glasses of wine during social gatherings. The patient has no known drug allergies. Her father was diagnosed with a myocardial infarction at age 60, and her mother died from a hemorrhagic stroke. Blood pressure is 125/80 mm Hg and pulse is 72/min. BMI is 29 kg/m2. Physical examination shows no abnormalities. ECG shows normal sinus rhythm with no abnormal repolarization changes. Serum creatinine is 1.1 mg/dL and hemoglobin A1c is 6.5%. Lipid panel shows LDL of 134 mg/dL and HDL of 45 mg/dL. The patient undergoes exercise stress testing. She exercises for 8 minutes without chest discomfort, and exercise ECG shows no abnormal ST-segment changes. Which of the following should be communicated to the patient regarding her stress testing results?
A)They are inconclusive because you have diabetes.
B)They are likely a false negative because you are on medical therapy.
C)They are nondiagnostic because you are female.
D)They indicate that coronary artery disease is very unlikely.
E)They indicate that you have a low risk for cardiac events in the near future.
A)They are inconclusive because you have diabetes.
B)They are likely a false negative because you are on medical therapy.
C)They are nondiagnostic because you are female.
D)They indicate that coronary artery disease is very unlikely.
E)They indicate that you have a low risk for cardiac events in the near future.

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
69
A 3-week-old male infant with Down's syndrome is brought by his parents to your office due to feeding difficulties. According to the mother, the infant becomes short of breath and his face turns blue during feeding, and when he cries. On chest auscultation, there is a harsh holosystolic murmur heard best over the lower left sternal border. There are no rales or wheezing over the lung fields. In the long run, this infant is at increased risk of developing which of the following?
A)Coronary artery disease
B)Diabetes mellitus
C)Acute leukemia
D)Osteosarcoma
E)Parkinson's disease
A)Coronary artery disease
B)Diabetes mellitus
C)Acute leukemia
D)Osteosarcoma
E)Parkinson's disease

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
70
A 38-year-old woman comes to the physician for a routine checkup. She has no current complaints. The patient's past medical history is significant for hypertension and type 2 diabetes mellitus. Her medications include low-dose hydrochlorothiazide, lisinopril, metformin, and glyburide. She smokes 1/2 pack of cigarettes daily and drinks alcohol occasionally. Her last menstrual period was 2 weeks ago. Blood pressure is 130/85 mm Hg and pulse is 85/min. The patient's body mass index is 32 kg/m2. The remainder of the physical examination is within normal limits. Her fasting blood glucose is 120 mg/dL and HbA1C level is 6.7%. Which of the following factors is the most significant predictor of future cardiovascular events in this patient?
A)Age
B)Alcohol consumption
C)Diabetes mellitus
D)Gender
E)Hypertension F)Obesity
G)Smoking
A)Age
B)Alcohol consumption
C)Diabetes mellitus
D)Gender
E)Hypertension F)Obesity
G)Smoking

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
71
A 62-year-old man with hypertension and heart failure comes to the office for follow-up 2 weeks after hospital discharge for acute decompensated heart failure. The patient becomes short of breath after walking 1 block or climbing a flight of stairs but does not have orthopnea, cough, or hemoptysis. Current medications include metoprolol succinate, sacubitril-valsartan, furosemide, and spironolactone. Blood pressure is 128/76 mm Hg and pulse is 80/min. Oxygen saturation is 95% on room air. Jugular venous pressure is estimated at 8 cm H2O. Lungs are clear to auscultation, and an S3 is heard at the apex. There is trace peripheral edema. Echocardiography shows left ventricular ejection fraction of 30%, mild mitral regurgitation, and mild pulmonary hypertension. The patient's serum creatinine is 1.2 mg/dL, and serum potassium is 5.0 mEq/L. Which of the following is the best additional therapy for this patient?
A)ACE inhibitor
B)Dihydropyridine calcium channel blocker
C)Endothelin receptor antagonist
D)Phosphodiesterase-5 inhibitor
E)Sodium-glucose cotransporter-2 inhibitor
A)ACE inhibitor
B)Dihydropyridine calcium channel blocker
C)Endothelin receptor antagonist
D)Phosphodiesterase-5 inhibitor
E)Sodium-glucose cotransporter-2 inhibitor

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
72
A 39-year-old man comes to the emergency department due to an episode of chest pain. He says, "I had dinner and 2 hours later started to get this discomfort in the middle of the chest. It felt dull and annoying." The pain lasted for 2 hours, waxed and waned in intensity, and did not radiate. The patient did not have any back pain, dyspnea, palpitations, or lightheadedness, and has never had similar pain episodes. After the pain subsided, his wife insisted that he go to the emergency department. Currently, he has no pain or discomfort and wants to return home. The patient does have occasional heartburn and takes over-the-counter antacids. Medical history is otherwise unremarkable. The patient has smoked a pack of cigarettes a day for the past 10 years. He does not drink alcohol or use illicit drugs. He has no known medication allergies. His father died suddenly in his sleep at age 55. His older brother is healthy. Blood pressure is 138/86 mm Hg and pulse is 89/min and regular. BMI is 28 kg/m2. There are no heart murmurs or additional sounds. No carotid bruits are heard. Abdominal examination is unremarkable. ECG shows normal sinus rhythm with nonspecific T-wave changes in leads II and III. Chest x-ray is normal. Which of the following is the best next step in management of this patient?
A)Obtain D-dimer level
B)Obtain troponin I level
C)Order treadmill exercise stress test
D)Prescribe lansoprazole and advise outpatient follow-up
E)Refer for coronary angiography
A)Obtain D-dimer level
B)Obtain troponin I level
C)Order treadmill exercise stress test
D)Prescribe lansoprazole and advise outpatient follow-up
E)Refer for coronary angiography

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
73
A 47-year-old man is brought to the emergency department after being injured by a lightning strike 10 minutes ago. He was playing tennis when a thunderstorm suddenly developed. He was struck by cloud-to-ground lightning and thrown several feet by the force of the bolt. Bystanders initiated chest compressions immediately. Emergency medical services arrived within 5 minutes and found the patient in cardiac arrest. On examination, his pupils are dilated and unresponsive to light. The electrical rhythm appears to be asystole. Which of the following is the most appropriate next step in management?
A)Attempt defibrillation
B)Continue chest compressions
C)Give patient amiodarone
D)Give patient atropine
E)Stop resuscitation
A)Attempt defibrillation
B)Continue chest compressions
C)Give patient amiodarone
D)Give patient atropine
E)Stop resuscitation

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
74
A 66-year-old woman comes to the office to follow up for heart failure. Four weeks ago, she was diagnosed with new onset heart failure with reduced ejection fraction of 30%. At that time, ECG showed normal sinus rhythm, narrow QRS complexes, and T-wave inversion in the lateral leads. Coronary angiogram revealed no significant coronary artery disease. She is feeling better except for mild exertional fatigue. The patient typically uses 2 pillows to sleep and gets up once at night to urinate. She has no lightheadedness. Her only other medical condition is type 2 diabetes mellitus. Current medical therapy is sacubitril-valsartan, metoprolol succinate, and furosemide. Blood pressure is 109/60 mm Hg, pulse is 62/min, and respirations are 12/min. Pulse oximetry shows 98% on room air. Examination shows normal jugular venous pressure, clear lungs, and a 2/6 pansystolic murmur at the apex. The abdomen is soft and nontender. She has no peripheral edema. Laboratory results are as follows: 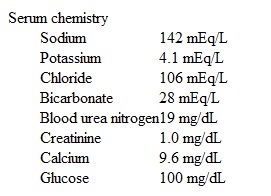 Which of the following is the most appropriate next step in pharmacotherapy management of this patient?
Which of the following is the most appropriate next step in pharmacotherapy management of this patient?
A)Add spironolactone to current regimen
B)Add lisinopril to current regimen
C)Add metolazone to current regimen
D)Decrease metoprolol succinate dose
E)Discontinue furosemide
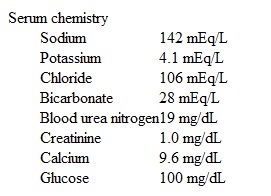 Which of the following is the most appropriate next step in pharmacotherapy management of this patient?
Which of the following is the most appropriate next step in pharmacotherapy management of this patient?A)Add spironolactone to current regimen
B)Add lisinopril to current regimen
C)Add metolazone to current regimen
D)Decrease metoprolol succinate dose
E)Discontinue furosemide

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
75
A 3-week-old male infant with Down's syndrome is brought by his parents to your office due to feeding difficulties. According to the mother, the infant becomes short of breath and his face turns blue during feeding, and when he cries. On chest auscultation, there is a harsh holosystolic murmur heard best over the lower left sternal border. There are no rales or wheezing over the lung fields.
Which of the following is the most useful test for diagnostic evaluation?
A)Chest radiograph
B)EKG
C)Hyperoxia test
D)Echocardiography
E)Cardiac catheterization
Which of the following is the most useful test for diagnostic evaluation?
A)Chest radiograph
B)EKG
C)Hyperoxia test
D)Echocardiography
E)Cardiac catheterization

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
76
A 64-year-old man comes to the office due to shortness of breath for the last 6 months. He describes his lifestyle as active but says, "I can't catch my breath when I walk fast or climb the stairs. Six months ago, I felt completely fine." He has no symptoms at rest or at night, and he has had no palpitations, chest pain, lightheadedness, syncope, or lower extremity swelling. The patient has a history of hypertension and diet-controlled type 2 diabetes mellitus. He also takes over-the-counter antacid for occasional heartburn. He is a lifetime nonsmoker and drinks beer over the weekend. The patient has no family history of heart attacks or sudden cardiac death, but his grandfather had a stroke in his 60s. Blood pressure is 149/86 mm Hg and pulse is 88/min and regular. Oxygen saturation is 97% on room air. Lungs are clear on auscultation. No heart murmurs are heard. There is no peripheral edema. ECG shows normal sinus rhythm, voltage criteria for left ventricular hypertrophy, and T-wave inversion in leads V5 and V6. Creatinine is 0.9 mg/dL and complete blood count is unremarkable. Echocardiogram shows a dilated left ventricle with ejection fraction of 38%. Which of the following is the best next step in management of this patient?
A)24-hour Holter monitoring
B)Ambulatory monitoring of blood pressure
C)Beta-natriuretic peptide and troponin I levels
D)Cardiac stress test
E)Polysomnography
A)24-hour Holter monitoring
B)Ambulatory monitoring of blood pressure
C)Beta-natriuretic peptide and troponin I levels
D)Cardiac stress test
E)Polysomnography

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
77
A 62-year-old man is brought to the emergency department due to shortness of breath, chest pain, and palpitations that started earlier today. For the past month, he has had intermittent palpitations accompanied by shortness of breath. This time the symptoms persisted and he called 911. Medical problems include hypertension, obesity, chronic obstructive pulmonary disease, myocardial infarction, and carotid artery stenosis. The patient underwent coronary artery bypass grafting surgery 4 years ago. He follows up with a cardiologist twice a year, and there has been no recent change in his medical regimen. He is an ex-smoker and consumes no alcohol. He has no known drug allergies. On initial evaluation in the emergency department, he appears uncomfortable and tachypneic. Immediate ECG shows atrial fibrillation with a rapid ventricular response (140-150/min), narrow QRS complexes, and T-wave inversion in leads V4 to V6. The patient is connected to a cardiac monitor. While the team is securing intravenous access, the patient becomes unresponsive. He has no palpable pulses over the major arteries. The cardiac monitor continues to show a narrow-complex tachycardia consistent with atrial fibrillation. Which of the following is the most appropriate next step in management of this patient?
A)Administer intravenous adenosine
B)Administer intravenous thrombolytics
C)Initiate chest compressions
D)Prepare for rapid defibrillation
E)Prepare for rapid synchronized cardioversion
A)Administer intravenous adenosine
B)Administer intravenous thrombolytics
C)Initiate chest compressions
D)Prepare for rapid defibrillation
E)Prepare for rapid synchronized cardioversion

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
78
A 62-year-old man comes to the office due to shortness of breath for the past 6 months. The patient, who describes his symptoms as progressive, has difficulty walking a block without becoming out of breath. He experiences chest tightness and midline "squeezing" that is relieved after 5 minutes of rest. He also has fatigue and poor sleep but no palpitations, orthopnea, cough, or syncope. His other medical problems include hypertension and gastroesophageal reflux disease. His medications are hydrochlorothiazide and ranitidine. The patient has smoked a pack of cigarettes daily for 35 years and drinks 1 or 2 beers daily. His father has high blood pressure and had a stroke in his 60s, and his mother died of breast cancer. On physical examination, the patient appears comfortable at rest. Blood pressure is 136/78 mm Hg and pulse is 84/min and regular. BMI is 41 kg/m2. No cardiac murmurs are heard. The lungs are clear on auscultation. There is trace edema of the lower extremities bilaterally. Resting ECG shows normal sinus rhythm with no ST-segment or T-wave abnormalities. Exercise stress testing is performed and reveals a 1-mm ST depression in ECG leads I, aVL, V5, and V6 at minimal exertion. The patient is started on aspirin, atorvastatin, and metoprolol and counseled on smoking cessation. Which of the following is the most appropriate next step in management of this patient?
A)Follow up in 4 weeks to evaluate the response to therapy
B)Obtain cardiac CT for coronary artery calcium scoring
C)Obtain dobutamine stress echocardiography
D)Perform pulmonary function testing
E)Schedule percutaneous coronary angiography
A)Follow up in 4 weeks to evaluate the response to therapy
B)Obtain cardiac CT for coronary artery calcium scoring
C)Obtain dobutamine stress echocardiography
D)Perform pulmonary function testing
E)Schedule percutaneous coronary angiography

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
79
A 63-year-old man comes to the office due to shortness of breath on mild exertion over the last 6 months. He has no chest pain, syncope, palpitations, or weight loss. The patient has ischemic cardiomyopathy, and he underwent coronary artery bypass grafting a year ago. He is receiving guideline-based optimal pharmacotherapy for heart failure. He appears comfortable at rest with no significant respiratory distress. Blood pressure is 122/80 mm Hg and pulse is 62/min and regular. Oxygen saturation is 96% on room air. S3 is heard at the apex. Scattered bibasilar crackles are heard at the lung bases. Abdominal examination is unremarkable. There is 1+ lower extremity edema bilaterally. Laboratory results are as follows: 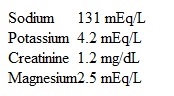 Transthoracic echocardiography shows left ventricular dilation with a left ventricular ejection fraction of 25%. Which of the following ECG findings would be an indication for further management in this patient?
Transthoracic echocardiography shows left ventricular dilation with a left ventricular ejection fraction of 25%. Which of the following ECG findings would be an indication for further management in this patient?
A)Deep Q waves in leads V1-V4
B)First-degree atrioventricular block with a PR interval of 230 msec
C)Left axis deviation
D)Left bundle branch block with a QRS complex duration of 160 msec
E)QTc interval prolongation to 480 msec
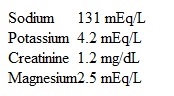 Transthoracic echocardiography shows left ventricular dilation with a left ventricular ejection fraction of 25%. Which of the following ECG findings would be an indication for further management in this patient?
Transthoracic echocardiography shows left ventricular dilation with a left ventricular ejection fraction of 25%. Which of the following ECG findings would be an indication for further management in this patient?A)Deep Q waves in leads V1-V4
B)First-degree atrioventricular block with a PR interval of 230 msec
C)Left axis deviation
D)Left bundle branch block with a QRS complex duration of 160 msec
E)QTc interval prolongation to 480 msec

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck
80
A 68-year-old white male with a history of paroxysmal atrial fibrillation, hypertension, and hypercholesterolemia is brought to the physician's office by his daughter because of nausea, anorexia, and confusion. His daughter states that he was admitted at an outside hospital two weeks ago because of uncontrolled hypertension and palpitations. He was started on a new medication. Prior to the recent hospitalization, he was taking digoxin, warfarin, simvastatin, and hydrochlorothiazide. His physical examination shows an irregular heart rate, but is otherwise unremarkable. His blood pressure is 130/80 mmHg, pulse rate is 50/minute and irregular, temperature 37.2C (99F), and respirations are 14/minute. Which of the following is the most likely medication that is contributing to his symptoms?
A)Atenolol
B)Enalapril
C)Clonidine
D)Valsartan
E)Verapamil
A)Atenolol
B)Enalapril
C)Clonidine
D)Valsartan
E)Verapamil

Unlock Deck
Unlock for access to all 1121 flashcards in this deck.
Unlock Deck
k this deck



