Deck 16: Diseases of the Liver Gallbladder and Exocrine Pancreas
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question

Unlock Deck
Sign up to unlock the cards in this deck!
Unlock Deck
Unlock Deck
1/80
Play
Full screen (f)
Deck 16: Diseases of the Liver Gallbladder and Exocrine Pancreas
1
Which treatment is used in the management of both hepatitis B and hepatitis C?
A) neomycin
B) spironolactone
C) prednisone
D) interferon
E) famotidine
A) neomycin
B) spironolactone
C) prednisone
D) interferon
E) famotidine
D
2
Bile salts aid in the absorption of fatty acids through the formation of which substance?
A) micelles
B) chylomicrons
C) acetyl CoA
D) prothrombin
E) mucoproteins
A) micelles
B) chylomicrons
C) acetyl CoA
D) prothrombin
E) mucoproteins
A
3
Which of the following statements best describes hepatobiliary scintigraphy?
A) A noninvasive test produces cross-section images of parts of the body.
B) A gamma camera takes pictures of a radioactive compound as the bile moves through the liver, bile ducts, gallbladder, and small intestine.
C) An endoscope is inserted down the throat, through the stomach, and into the small intestine to view internal structures.
D) A noninvasive X-ray produces three-dimensional pictures of parts of the body.
E) The patient is injected with a small amount of radioactive material that is absorbed by the gallbladder, which is then stimulated to contract.
A) A noninvasive test produces cross-section images of parts of the body.
B) A gamma camera takes pictures of a radioactive compound as the bile moves through the liver, bile ducts, gallbladder, and small intestine.
C) An endoscope is inserted down the throat, through the stomach, and into the small intestine to view internal structures.
D) A noninvasive X-ray produces three-dimensional pictures of parts of the body.
E) The patient is injected with a small amount of radioactive material that is absorbed by the gallbladder, which is then stimulated to contract.
B
4
Which condition is most commonly associated with nonalcoholic steatohepatitis (NASH)?
A) obesity
B) high blood glucose
C) celiac disease
D) hypothyroidism
E) anorexia
A) obesity
B) high blood glucose
C) celiac disease
D) hypothyroidism
E) anorexia

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
5
Which of the following statements is true of alcoholism in older adults?
A) Approximately 20% of people over 65 abused alcohol.
B) Most adults become addicted to alcohol later in life in response to problems.
C) Older adults are even more susceptible to nutrient deficiencies when they abuse alcohol.
D) Most primary care providers identify alcohol abuse in older adults because of routine assessments.
E) Alcohol abuse among older adults is one of the most commonly identified problems of aging.
A) Approximately 20% of people over 65 abused alcohol.
B) Most adults become addicted to alcohol later in life in response to problems.
C) Older adults are even more susceptible to nutrient deficiencies when they abuse alcohol.
D) Most primary care providers identify alcohol abuse in older adults because of routine assessments.
E) Alcohol abuse among older adults is one of the most commonly identified problems of aging.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
6
Which type of hepatitis is most commonly transmitted through the fecal-oral route?
A) hepatitis A
B) hepatitis B
C) hepatitis C
D) hepatitis D
E) hepatitis E
A) hepatitis A
B) hepatitis B
C) hepatitis C
D) hepatitis D
E) hepatitis E

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
7
Which hormone is secreted by the delta cells of the islets of Langerhans?
A) thyroid stimulating hormone
B) luteinizing hormone
C) somatostatin
D) amylase
E) testosterone
A) thyroid stimulating hormone
B) luteinizing hormone
C) somatostatin
D) amylase
E) testosterone

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
8
Which medication is most commonly used in the treatment of hepatic encephalopathy?
A) manganese
B) tyramine
C) lactulose
D) octopamine
E) phenylethanolamine
A) manganese
B) tyramine
C) lactulose
D) octopamine
E) phenylethanolamine

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
9
Which factor in a laboratory test is most likely to be elevated in a patient with fatty liver?
A) serum albumin
B) glucose
C) red blood cells
D) cortisol
E) serum transaminase
A) serum albumin
B) glucose
C) red blood cells
D) cortisol
E) serum transaminase

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
10
Common manifestations of all types of hepatitis include jaundice, fatigue, vomiting, and:
A) epigastric pain
B) dark urine
C) diarrhea
D) generalized rash
E) dilated pupils
A) epigastric pain
B) dark urine
C) diarrhea
D) generalized rash
E) dilated pupils

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
11
The cause of fatty liver after alcohol ingestion is:
A) greater amounts of glucagon secretion and enhanced gluconeogenesis from amino acids
B) elevated tryptophan levels and the formation of serotonin
C) the increased availability of fatty acids in the liver
D) esterification of fatty acids
E) the increased production and absorption of ammonia
A) greater amounts of glucagon secretion and enhanced gluconeogenesis from amino acids
B) elevated tryptophan levels and the formation of serotonin
C) the increased availability of fatty acids in the liver
D) esterification of fatty acids
E) the increased production and absorption of ammonia

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
12
Increased destruction of red blood cells with rapid release of bilirubin into the blood is known as:
A) obstructive jaundice
B) bilirubin conjugation
C) post-hepatic jaundice
D) hemolytic jaundice
E) bilirubin dissection
A) obstructive jaundice
B) bilirubin conjugation
C) post-hepatic jaundice
D) hemolytic jaundice
E) bilirubin dissection

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
13
Ammonia is absorbed and transported in the intestinal venous blood to the liver, where it is metabolized into which substance?
A) amino acids
B) urea
C) fatty acids
D) glucose
E) glycogen
A) amino acids
B) urea
C) fatty acids
D) glucose
E) glycogen

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
14
The most common nutrient-drug interactions that occur with mycophenolate (purine synthesis inhibitor) are:
A) high cholesterol and hypertriglyceridemia
B) dyspepsia, abdominal pain, and diarrhea
C) hematochezia and iron deficiency anemia
D) muscle cramps, joint pain, and fever
E) headache, dizziness, and confusion
A) high cholesterol and hypertriglyceridemia
B) dyspepsia, abdominal pain, and diarrhea
C) hematochezia and iron deficiency anemia
D) muscle cramps, joint pain, and fever
E) headache, dizziness, and confusion

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
15
Hepatitis C is most commonly transmitted through which route?
A) exposure to blood or body fluids from an infected person
B) the fecal-oral route
C) excessive alcohol intake
D) contaminated drinking water
E) sewage
A) exposure to blood or body fluids from an infected person
B) the fecal-oral route
C) excessive alcohol intake
D) contaminated drinking water
E) sewage

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
16
Which organ stores bile that is produced in the liver?
A) pancreas
B) kidney
C) spleen
D) gallbladder
E) stomach
A) pancreas
B) kidney
C) spleen
D) gallbladder
E) stomach

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
17
When ascites is present, which nutrition modification is typically necessary?
A) low sodium
B) decreased fluid intake
C) increased vitamin K
D) low fiber
E) decreased protein
A) low sodium
B) decreased fluid intake
C) increased vitamin K
D) low fiber
E) decreased protein

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
18
A syndrome of impaired mental status and abnormal neuromuscular function that results from liver failure is known as:
A) hepatic stenosis
B) jaundice
C) hepatic encephalopathy
D) fulminant hepatitis
E) hepatomegaly
A) hepatic stenosis
B) jaundice
C) hepatic encephalopathy
D) fulminant hepatitis
E) hepatomegaly

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
19
At which level of serum bilirubin does the skin begin to appear jaundiced?
A) 1.0-1.1 mg/dL
B) 1.5-1.9 mg/dL
C) 2.1-2.4 mg/dL
D) 2.5-3.0 mg/dL
E) 3.3-3.5 mg/dL
A) 1.0-1.1 mg/dL
B) 1.5-1.9 mg/dL
C) 2.1-2.4 mg/dL
D) 2.5-3.0 mg/dL
E) 3.3-3.5 mg/dL

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
20
A patient with hepatic encephalopathy is being assessed according to the Adapted West Haven Criteria. The patient has marked somnolence, psychomotor agitation, and his speech is difficult to understand. At which stage of the disease is the patient?
A) 0
B) 1
C) 2
D) 3
E) 4
A) 0
B) 1
C) 2
D) 3
E) 4

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
21
Symptoms associated with acute pancreatitis include:
A) diarrhea, bloody stools, and abdominal cramping
B) epigastric pain and ascites
C) flatulence, diarrhea, and abdominal distention
D) fever and headache
E) abdominal pain, nausea, and vomiting
A) diarrhea, bloody stools, and abdominal cramping
B) epigastric pain and ascites
C) flatulence, diarrhea, and abdominal distention
D) fever and headache
E) abdominal pain, nausea, and vomiting

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
22
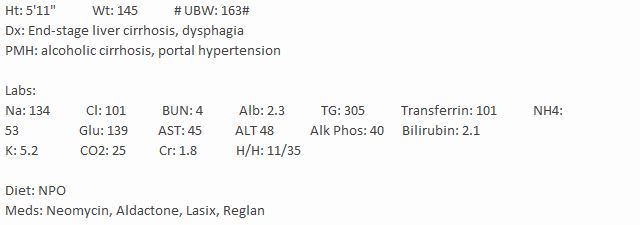
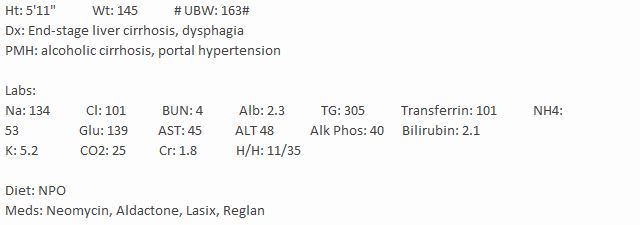
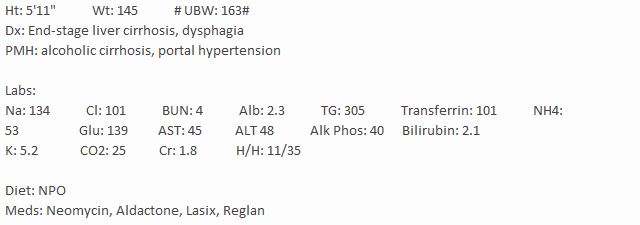
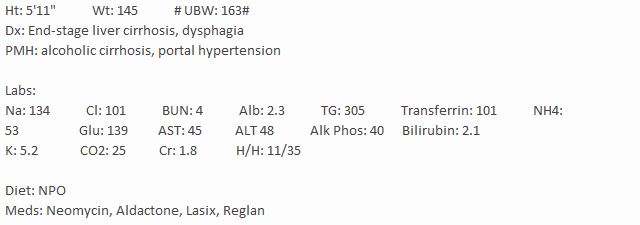
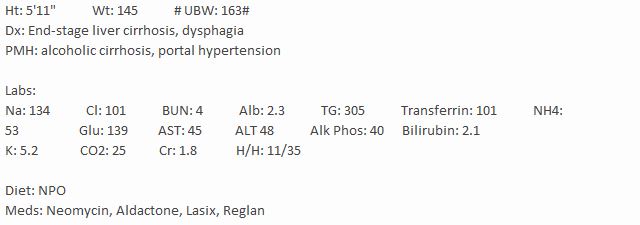
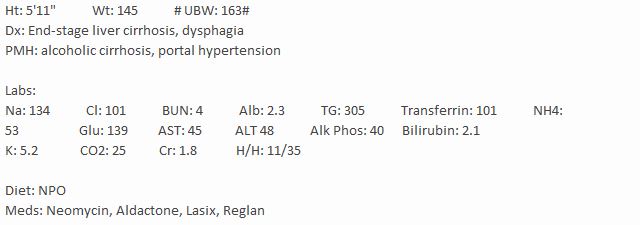
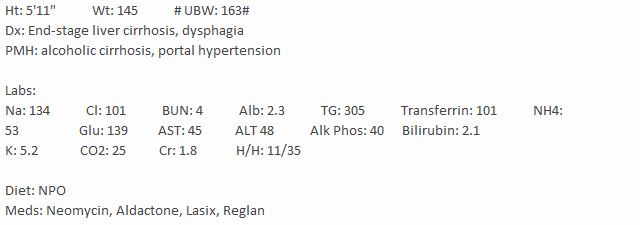
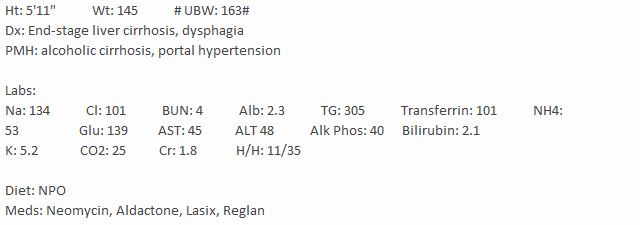
JB is a 53-year-old male who has recently divorced. He has experienced periods of depression and decreased appetite. His family reports a history of heavy drinking habits and a 15 kg weight loss. He was previously diagnosed with cirrhosis and portal hypertension. Paracentesis and TIPS procedures were performed. JB's condition seems to have worsened; he complains of stomach pains, nausea, and vomiting at times. His abdomen is sore to touch and feels swollen. JB has developed ascites and pedal edema. His urinary output has decreased, and he continues to lose weight. JB also complains of pain when swallowing food. Because of JB's persistent symptoms, he's been admitted to a hospital. A referral to the SLP for an MBS was also ordered and resulted in dysphagia for which pureed diet was recommended. On day 2, JB still complains of nausea and no per os intake has been reported. The MD prescribed a dietary consultation. An RD is required to assess the patient and recommend alternate means of nutrition support, currently NPO.
The RD recommends sodium restriction because of JB's ascites. How much sodium should the RD initially recommend to JB each day?
A) 500 mg/day
B) 1000 mg/day
C) 2000 mg/day
D) 3000 mg/day
E) 3500 mg/day
The RD recommends sodium restriction because of JB's ascites. How much sodium should the RD initially recommend to JB each day?
A) 500 mg/day
B) 1000 mg/day
C) 2000 mg/day
D) 3000 mg/day
E) 3500 mg/day

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
23
The most common cause of cirrhosis in the United States is:
A) alcohol abuse
B) hepatitis B
C) nonalcoholic fatty liver disease
D) hepatitis C
E) biliary colic
A) alcohol abuse
B) hepatitis B
C) nonalcoholic fatty liver disease
D) hepatitis C
E) biliary colic

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
24
A patient with hepatic encephalopathy is being assessed according to the Adapted West Haven Criteria. The patient is unable to perform easy mental tests and is awake but inattentive. The patient's speech is difficult to understand. Identify the stage of encephalopathy that has these characteristics.
A) 0
B) 1
C) 2
D) 3
E) 4
A) 0
B) 1
C) 2
D) 3
E) 4

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
25
Astrocytes are the specialized phagocytic cells of the reticuloendothelial system found on the luminal surface of the hepatic sinusoids.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
26
JB is a 53-year-old male who has recently divorced. He has experienced periods of depression and decreased appetite. His family reports a history of heavy drinking habits and a 15 kg weight loss. He was previously diagnosed with cirrhosis and portal hypertension. Paracentesis and TIPS procedures were performed. JB's condition seems to have worsened; he complains of stomach pains, nausea, and vomiting at times. His abdomen is sore to touch and feels swollen. JB has developed ascites and pedal edema. His urinary output has decreased, and he continues to lose weight. JB also complains of pain when swallowing food. Because of JB's persistent symptoms, he's been admitted to a hospital. A referral to the SLP for an MBS was also ordered and resulted in dysphagia for which pureed diet was recommended. On day 2, JB still complains of nausea and no per os intake has been reported. The MD prescribed a dietary consultation. An RD is required to assess the patient and recommend alternate means of nutrition support, currently NPO.
How much protein consumption will the registered dietitian recommend to JB?
A) 0.8-1.0 g/kg
B) 1.0-1.1 g/kg
C) 1.2-1.5 g/kg
D) 1.8-2.0 g/kg
E) 2.0-2.2 g/kg
How much protein consumption will the registered dietitian recommend to JB?
A) 0.8-1.0 g/kg
B) 1.0-1.1 g/kg
C) 1.2-1.5 g/kg
D) 1.8-2.0 g/kg
E) 2.0-2.2 g/kg

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
27
What complication most commonly occurs with folate deficiency?
A) reduced bone formation and mineralization
B) villus shortening in the intestine
C) retrograde amnesia
D) ataxia and sensory neuropathy
E) pancreatic insufficiency
A) reduced bone formation and mineralization
B) villus shortening in the intestine
C) retrograde amnesia
D) ataxia and sensory neuropathy
E) pancreatic insufficiency

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
28
JB is a 53-year-old male who has recently divorced. He has experienced periods of depression and decreased appetite. His family reports a history of heavy drinking habits and a 15 kg weight loss. He was previously diagnosed with cirrhosis and portal hypertension. Paracentesis and TIPS procedures were performed. JB's condition seems to have worsened; he complains of stomach pains, nausea, and vomiting at times. His abdomen is sore to touch and feels swollen. JB has developed ascites and pedal edema. His urinary output has decreased, and he continues to lose weight. JB also complains of pain when swallowing food. Because of JB's persistent symptoms, he's been admitted to a hospital. A referral to the SLP for an MBS was also ordered and resulted in dysphagia for which pureed diet was recommended. On day 2, JB still complains of nausea and no per os intake has been reported. The MD prescribed a dietary consultation. An RD is required to assess the patient and recommend alternate means of nutrition support, currently NPO.
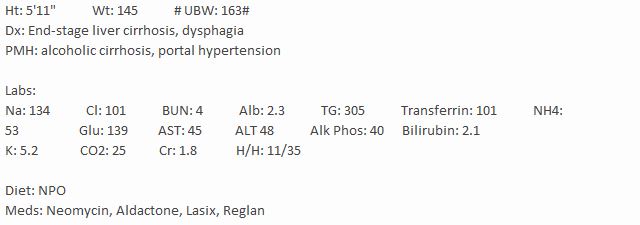
Because of JB's history of alcohol abuse, he is most likely at risk of which nutrient deficiency?
A) potassium
B) vitamin A
C) sodium
D) vitamin B6
E) vitamin E
Because of JB's history of alcohol abuse, he is most likely at risk of which nutrient deficiency?
A) potassium
B) vitamin A
C) sodium
D) vitamin B6
E) vitamin E

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
29
JB is a 53-year-old male who has recently divorced. He has experienced periods of depression and decreased appetite. His family reports a history of heavy drinking habits and a 15 kg weight loss. He was previously diagnosed with cirrhosis and portal hypertension. Paracentesis and TIPS procedures were performed. JB's condition seems to have worsened; he complains of stomach pains, nausea, and vomiting at times. His abdomen is sore to touch and feels swollen. JB has developed ascites and pedal edema. His urinary output has decreased, and he continues to lose weight. JB also complains of pain when swallowing food. Because of JB's persistent symptoms, he's been admitted to a hospital. A referral to the SLP for an MBS was also ordered and resulted in dysphagia for which pureed diet was recommended. On day 2, JB still complains of nausea and no per os intake has been reported. The MD prescribed a dietary consultation. An RD is required to assess the patient and recommend alternate means of nutrition support, currently NPO.
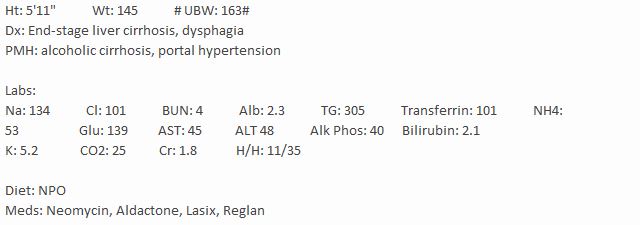
How would the registered dietitian determine JB's caloric needs in this situation?
A) 15-20 kcal/kg IBW
B) 20-25 kcal/kg IBW
C) 25-30 kcal/kg IBW
D) 30-35 kcal/kg current body weight
E) 35-40 kcal/kg current body weight
How would the registered dietitian determine JB's caloric needs in this situation?
A) 15-20 kcal/kg IBW
B) 20-25 kcal/kg IBW
C) 25-30 kcal/kg IBW
D) 30-35 kcal/kg current body weight
E) 35-40 kcal/kg current body weight

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
30
Wernicke-Korsakoff syndrome is associated with excessive alcohol intake and a deficiency of which nutrient?
A) thiamin
B) vitamin B12
C) vitamin D
D) folate
E) vitamin B6
A) thiamin
B) vitamin B12
C) vitamin D
D) folate
E) vitamin B6

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
31
Which condition is commonly associated with chronic pancreatitis?
A) celiac disease
B) anorexia
C) diabetes
D) renal failure
E) atrial fibrillation
A) celiac disease
B) anorexia
C) diabetes
D) renal failure
E) atrial fibrillation

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
32
Alcohol causes increased urinary excretion of which nutrient?
A) folate
B) vitamin B12
C) magnesium
D) chloride
E) sodium
A) folate
B) vitamin B12
C) magnesium
D) chloride
E) sodium

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
33
JB is a 53-year-old male who has recently divorced. He has experienced periods of depression and decreased appetite. His family reports a history of heavy drinking habits and a 15 kg weight loss. He was previously diagnosed with cirrhosis and portal hypertension. Paracentesis and TIPS procedures were performed. JB's condition seems to have worsened; he complains of stomach pains, nausea, and vomiting at times. His abdomen is sore to touch and feels swollen. JB has developed ascites and pedal edema. His urinary output has decreased, and he continues to lose weight. JB also complains of pain when swallowing food. Because of JB's persistent symptoms, he's been admitted to a hospital. A referral to the SLP for an MBS was also ordered and resulted in dysphagia for which pureed diet was recommended. On day 2, JB still complains of nausea and no per os intake has been reported. The MD prescribed a dietary consultation. An RD is required to assess the patient and recommend alternate means of nutrition support, currently NPO.
Following the paracentesis, the nutritionist might recommend what component to the nutrition prescription?
A) vitamin B12
B) protein
C) hypertonic fluid
D) vitamin D
E) potassium
Following the paracentesis, the nutritionist might recommend what component to the nutrition prescription?
A) vitamin B12
B) protein
C) hypertonic fluid
D) vitamin D
E) potassium

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
34
Identify the enzyme that hydrolyzes interior peptide bonds to form polypeptides.
A) lipase
B) amylase
C) chymotrypsin
D) ribonuclease
E) renin
A) lipase
B) amylase
C) chymotrypsin
D) ribonuclease
E) renin

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
35
When steatorrhea associated with pancreatitis occurs, what intervention should follow?
A) administration of pancreatic digestive enzymes
B) early initiation (within 48 hours) of enteral nutrition
C) a low-carbohydrate nutrition prescription with modest protein
D) calcium supplements along with a multivitamin
E) fluid and sodium restriction
A) administration of pancreatic digestive enzymes
B) early initiation (within 48 hours) of enteral nutrition
C) a low-carbohydrate nutrition prescription with modest protein
D) calcium supplements along with a multivitamin
E) fluid and sodium restriction

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
36
Which nutrition intervention is appropriate for a patient with an acute attack of cholangitis?
A) a low-fat diet
B) decreased fluid intake
C) supplementation with vitamin B6
D) enteral nutrition
E) increased carbohydrate intake
A) a low-fat diet
B) decreased fluid intake
C) supplementation with vitamin B6
D) enteral nutrition
E) increased carbohydrate intake

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
37
Nutrition interventions for a client with alcoholic hepatitis include a diet that is:
A) low in carbohydrates
B) high in saturated fat
C) low in artificial sugars
D) low in protein
E) high in carbohydrates
A) low in carbohydrates
B) high in saturated fat
C) low in artificial sugars
D) low in protein
E) high in carbohydrates

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
38
The recommended daily protein intake for a patient with alcoholic hepatitis would be:
A) 0.5-0.8 grams/kilogram
B) 0.8-1.0 grams/kilogram
C) 1.0-1.5 grams/kilogram
D) 1.5-2.0 grams/kilogram
E) 2.5-3.0 grams/kilogram
A) 0.5-0.8 grams/kilogram
B) 0.8-1.0 grams/kilogram
C) 1.0-1.5 grams/kilogram
D) 1.5-2.0 grams/kilogram
E) 2.5-3.0 grams/kilogram

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
39
Which type of food would the dietitian most likely recommend to a patient with nonalcoholic fatty liver disease (NAFLD)?
A) whole yogurt
B) lean pork
C) egg noodles
D) corn chips
E) chocolate milk
A) whole yogurt
B) lean pork
C) egg noodles
D) corn chips
E) chocolate milk

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
40
The liver receives blood from two sources: the hepatic portal vein and the hepatic artery.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
41
_______________ is a manifestation of thiamin deficiency usually seen in individuals suffering from alcoholism.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
42
Standard medical treatments for hepatic encephalopathy are primarily directed at reducing the amount of circulating ammonia.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
43
Forty percent of acute pancreatitis cases are due to a gallstone passing into the bile duct and temporarily lodging at the sphincter of Oddi.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
44
The basic functional unit of the liver is the _______________, which is a cylindrical structure several millimeters in length and 0.8-2 mm in diameter.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
45
_______________ is defined as the replacement of functional hepatocytes by fibrotic cells.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
46
Red blood cells, alkaline phosphatase, and serum glucose are generally elevated with hepatitis.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
47
_______________ or steatosis occurs in about 25-30% of the general U.S. population and 90% of chronic alcohol abusers.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
48
_______________ presents as small, brief, intermittent movements of individual fingers and may be seen in patients with hepatic encephalopathy.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
49
The pancreas is the only organ of the body that has both _______________ and _______________ functions.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
50
The hepatic duct descends to the right for a few inches and is then joined by the cystic duct from the gallbladder to form the _______________.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
51
The _______________ is a surgical procedure for ascites that reroutes blood flow to the liver and reduces pressure in all auxiliary veins.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
52
The most common clinical sign of fatty liver is _______________.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
53
Ethanol and acetaldehyde have a hepatotoxic effect that interferes with metabolism and activation of vitamins by liver cells.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
54
Prolonged parenteral nutrition and short bowel syndrome can cause biliary stasis and therefore increase the risk of gallstones.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
55
The most common causes of cirrhosis are chronic HCV and alcoholism, and 95% of heavy drinkers develop the disease.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
56
Withdrawal of fluid from the abdomen via a catheter, often used as treatment for ascites, is called _______________.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
57
The hepatotoxic alcohol threshold at which ALD may develop is 20 g (two drinks) daily for men.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
58
_______________ causes a liver disorder that is uncommon in the United States and requires HBV to replicate.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
59
Autodigestion of the pancreas is prevented by storing the digestive enzymes in their inactive forms as zymogens.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
60
_______________ is a form of toxic liver injury associated with chronic ethanol consumption.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
61
Explain why malnutrition is prominent in a patient with alcoholism or alcoholic hepatitis.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
62
Define the functions of the gallbladder.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
63
Describe the major functions of the pancreas.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
64
A patient's eligibility to be placed on the waiting list for a liver transplant is determined based on the _______________ scoring system.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
65
_______________ is an inflammation of the biliary ducts, usually secondary to obstruction of the common bile duct leading to infection.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
66
The liver is the source of bile, but bile's composition is further modified by the _______________.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
67
An estimated dosage range would be _______________ IU of lipase per meal for a patient with chronic pancreatitis.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
68
Describe the possible complications associated with thiamin deficiency in a patient with alcohol dependency.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
69
Which surgical procedure is used to detect and remove bile duct stones?
A) magnetic resonance cholangiopancreatography
B) percutaneous transhepatic cholangiography
C) hepatobiliary scintigraphy
D) magnetic resonance imaging
E) endoscopic retrograde cholangiopancreatography
A) magnetic resonance cholangiopancreatography
B) percutaneous transhepatic cholangiography
C) hepatobiliary scintigraphy
D) magnetic resonance imaging
E) endoscopic retrograde cholangiopancreatography

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
70
Small crystals of cholesterol on the surface of the inflamed mucosa of the gallbladder act as _______________ (points of origin) for further precipitation of cholesterol, and the crystals grow larger and larger.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
71
Give three examples of possible nutrition diagnoses associated with acute hepatitis.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
72
Describe the differences between hepatitis A, B, and C, including their methods of transmission, clinical manifestations, and modes of treatment.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
73
Describe the differences between acute and chronic pancreatitis, including causes, manifestations, and nutrition intervention.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
74
When a gallstone passes from the gallbladder through the cystic duct and lodges in the common bile duct or in the head of the pancreas, the condition is called _______________.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
75
Describe a basic nutrition assessment for a patient with gallbladder disease.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
76
Briefly describe the impairment of neurotransmission involved with hepatic encephalopathy.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
77
List three different causes of cirrhosis found in the United States.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
78
Which group of people is most commonly infected with chronic hepatitis B virus in the United States?
A) Native Americans
B) Hispanic/Latinos
C) Caucasians
D) African Americans
E) Pacific Islanders
A) Native Americans
B) Hispanic/Latinos
C) Caucasians
D) African Americans
E) Pacific Islanders

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
79
Fat malabsorption with chronic pancreatitis results in _______________.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
80
_______________ is the formation of calculi within the gallbladder or biliary duct system.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck



