Deck 14: Diseases of the Upper Gastrointestinal Tract
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
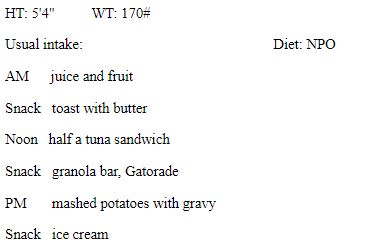
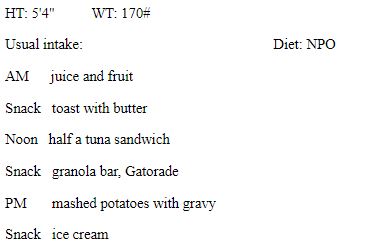
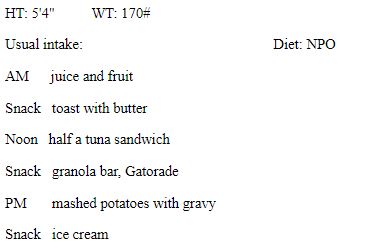
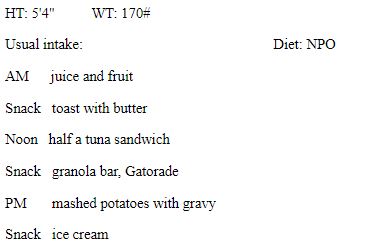
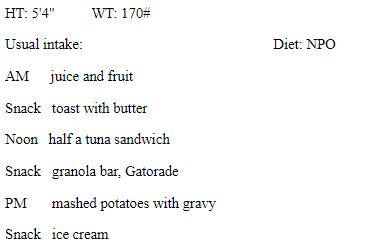
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question

Unlock Deck
Sign up to unlock the cards in this deck!
Unlock Deck
Unlock Deck
1/80
Play
Full screen (f)
Deck 14: Diseases of the Upper Gastrointestinal Tract
1
The control of gastric secretions is accomplished through complementary actions of the nervous and endocrine systems and involves four major chemical messengers: acetylcholine, histamine, gastrin, and:
A) serotonin
B) nitric oxide
C) somatostatin
D) neurotensin
E) norepinephrine
A) serotonin
B) nitric oxide
C) somatostatin
D) neurotensin
E) norepinephrine
C
2
What is an example of a nutrition intervention recommended for stomatitis?
A) increase intake of carbonated beverages
B) consume no more than 2 alcoholic drinks per day
C) avoid extremes of hot or cold food temperatures
D) use alcohol-based mouth rinses to keep the mouth clean
E) avoid oral glutamine supplements
A) increase intake of carbonated beverages
B) consume no more than 2 alcoholic drinks per day
C) avoid extremes of hot or cold food temperatures
D) use alcohol-based mouth rinses to keep the mouth clean
E) avoid oral glutamine supplements
C
3
Which is considered a true statement regarding hiatal hernia?
A) Most cases of hiatal hernia are considered type 2 (rolling).
B) Symptoms of hiatal hernia are similar to those of Crohn's disease.
C) Incidence of hiatal hernia decreases with age.
D) Pregnancy may increase the risk of hiatal hernia.
E) Surgery for hiatal hernia involves Roux-en-Y gastric bypass.
A) Most cases of hiatal hernia are considered type 2 (rolling).
B) Symptoms of hiatal hernia are similar to those of Crohn's disease.
C) Incidence of hiatal hernia decreases with age.
D) Pregnancy may increase the risk of hiatal hernia.
E) Surgery for hiatal hernia involves Roux-en-Y gastric bypass.
D
4
Which activity may increase the risk of development of dental caries?
A) drinking liquid while eating
B) eating whole grain bread
C) chewing sugarless gum
D) sipping sugared beverages for prolonged periods
E) consuming fresh fruit
A) drinking liquid while eating
B) eating whole grain bread
C) chewing sugarless gum
D) sipping sugared beverages for prolonged periods
E) consuming fresh fruit

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
5
Which of the following statements best describes the pharyngeal phase of swallowing?
A) It is the phase in which the involuntary swallowing reflux begins and the bolus is carried through the pharynx to the top of the esophagus.
B) It is the phase in which there is a rapid passage of large amounts of food into the small intestine.
C) It is the phase in which esophageal peristalsis carries the bolus through the esophagus and LES and into the stomach.
D) It is the phase in which the tongue moves the bolus to the back of the throat.
E) It is the phase in which the food is chewed and made into a bolus by the tongue, teeth, and mandible.
A) It is the phase in which the involuntary swallowing reflux begins and the bolus is carried through the pharynx to the top of the esophagus.
B) It is the phase in which there is a rapid passage of large amounts of food into the small intestine.
C) It is the phase in which esophageal peristalsis carries the bolus through the esophagus and LES and into the stomach.
D) It is the phase in which the tongue moves the bolus to the back of the throat.
E) It is the phase in which the food is chewed and made into a bolus by the tongue, teeth, and mandible.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
6
Which of the following electrolytes are present in saliva?
A) potassium, sodium chloride, bicarbonate
B) sodium, calcium chloride, calcium
C) magnesium, iron, phosphate
D) phosphate, bicarbonate, potassium
E) iron, hydrogen chloride, magnesium
A) potassium, sodium chloride, bicarbonate
B) sodium, calcium chloride, calcium
C) magnesium, iron, phosphate
D) phosphate, bicarbonate, potassium
E) iron, hydrogen chloride, magnesium

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
7
What is an example of a change in gastrointestinal physiology that occurs with aging?
A) increased upper esophageal pressure
B) atrophy of the small intestine mucosa
C) enhanced excretion of hydrochloric acid in the stomach
D) increased incidences of diarrhea
E) overproduction of saliva in the mouth
A) increased upper esophageal pressure
B) atrophy of the small intestine mucosa
C) enhanced excretion of hydrochloric acid in the stomach
D) increased incidences of diarrhea
E) overproduction of saliva in the mouth

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
8
Which intervention is most appropriate for preventing "baby bottle tooth decay?"
A) taking a child to the dentist by the time he is 6 months old
B) weaning a child from the bottle by 24 months of age
C) removing a bottle from the child's mouth during sleep
D) brushing the baby's teeth at least once per week
E) offering juice instead of formula
A) taking a child to the dentist by the time he is 6 months old
B) weaning a child from the bottle by 24 months of age
C) removing a bottle from the child's mouth during sleep
D) brushing the baby's teeth at least once per week
E) offering juice instead of formula

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
9
The innermost layer of the esophagus is called the:
A) muscle layer
B) mucosa
C) adventitia
D) secretory layer
E) submucosa
A) muscle layer
B) mucosa
C) adventitia
D) secretory layer
E) submucosa

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
10
A jaw fracture that results in multiple pieces of bone is called a:
A) comminuted fracture
B) open fracture
C) closed fracture
D) incomplete fracture
E) complete fracture
A) comminuted fracture
B) open fracture
C) closed fracture
D) incomplete fracture
E) complete fracture

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
11
Which medication is classified as a proton pump inhibitor?
A) Mylanta
B) Gaviscon
C) Pepcid AC
D) Nexium
E) Reglan
A) Mylanta
B) Gaviscon
C) Pepcid AC
D) Nexium
E) Reglan

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
12
Inflammation of the oral mucosa that is often associated with fungal infections or with herpes-like viruses is called:
A) stomatitis
B) gingivitis
C) cheilosis
D) glossitis
E) xerostomia
A) stomatitis
B) gingivitis
C) cheilosis
D) glossitis
E) xerostomia

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
13
Food storage occurs primarily in which part of the stomach?
A) corpus
B) antrum
C) fundus
D) pyloric canal
E) cardia
A) corpus
B) antrum
C) fundus
D) pyloric canal
E) cardia

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
14
Identify the chemical messenger that stimulates the production of hydrochloric acid.
A) gastrin
B) histamine
C) somatostatin
D) acetylcholine
E) dopamine
A) gastrin
B) histamine
C) somatostatin
D) acetylcholine
E) dopamine

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
15
A dietitian is providing nutrition information to a patient with a jaw fracture who has had a maxillomandibular fixation. Which type of food would the dietitian most likely tell the client to avoid?
A) rye bread
B) 2% milk
C) bananas
D) pasta
E) soft-cooked eggs
A) rye bread
B) 2% milk
C) bananas
D) pasta
E) soft-cooked eggs

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
16
Saliva is produced in the mouth by three pairs of salivary glands: the parotid, submandibular, and:
A) occipital
B) sublingual
C) supramandibular
D) lingual
E) maxillary
A) occipital
B) sublingual
C) supramandibular
D) lingual
E) maxillary

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
17
Which of the following best describes a nutrition intervention for xerostomia?
A) using a dehumidifier at bedtime
B) avoiding sour and tart foods
C) adding extra sauces and gravies to foods
D) increasing intake of hot foods and fluids
E) limiting caffeine to three servings per day
A) using a dehumidifier at bedtime
B) avoiding sour and tart foods
C) adding extra sauces and gravies to foods
D) increasing intake of hot foods and fluids
E) limiting caffeine to three servings per day

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
18
Which is an example of a factor that contributes to lower esophageal sphincter incompetence?
A) renal artery stenosis
B) increased secretion of aldosterone
C) cardiomyopathy
D) cigarette smoking
E) increased secretion of cortisol
A) renal artery stenosis
B) increased secretion of aldosterone
C) cardiomyopathy
D) cigarette smoking
E) increased secretion of cortisol

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
19
A patient with dysphagia aspirates food approximately 10% of the time while eating and has no cough reflex. According to the Dysphagia Severity Scale, which level of severity would this patient be classified as having?
A) 2
B) 3
C) 4
D) 5
E) 6
A) 2
B) 3
C) 4
D) 5
E) 6

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
20
Hydrochloric acid and intrinsic factor are secreted in the stomach by:
A) the pylorus
B) histamine
C) somatostatin
D) parietal cells
E) mucous cells
A) the pylorus
B) histamine
C) somatostatin
D) parietal cells
E) mucous cells

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
21
A patient is has to undergo a procedure that involves passing a tube through the oral pharynx into the stomach. The barometric pressure is measured using a transducer. This procedure most accurately describes:
A) endoscopy
B) barium radiology study
C) esophageal manometry study
D) 24-hour pH monitoring
E) urea breath test
A) endoscopy
B) barium radiology study
C) esophageal manometry study
D) 24-hour pH monitoring
E) urea breath test

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
22
LK is a 40-year-old female s/p gastric resection 2 weeks ago due to a perforated ulcer from complicated PUD. Prior to her surgery, she was experiencing severe pain and had an upset stomach. She is now complaining of persistent diarrhea after she eats. 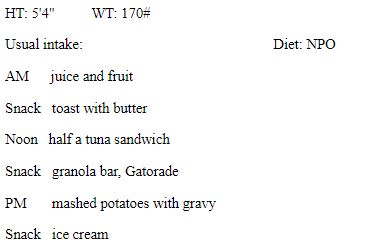
Which foods would the dietitian most likely recommend?
A) scrambled eggs
B) chocolate milk
C) sausage
D) red wine
E) peanut butter
Which foods would the dietitian most likely recommend?
A) scrambled eggs
B) chocolate milk
C) sausage
D) red wine
E) peanut butter

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
23
Which of the following is a possible cause of xerostomia?
A) lying on bed immediately after meals
B) eating frequent and large meals
C) rinsing the mouth with a saline solution
D) taking drugs for cancer treatment
E) adding extra sauces and gravies to foods
A) lying on bed immediately after meals
B) eating frequent and large meals
C) rinsing the mouth with a saline solution
D) taking drugs for cancer treatment
E) adding extra sauces and gravies to foods

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
24
Which type of food would most likely be recommended during gastroparesis?
A) whole oats
B) prune juice
C) cheese
D) sushi
E) buttermilk
A) whole oats
B) prune juice
C) cheese
D) sushi
E) buttermilk

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
25
The most common symptoms of gastroparesis are:
A) abdominal pain and hematemesis
B) nausea, vomiting, and postprandial fullness
C) abdominal distention, nausea, and flatulence
D) epigastric pain and blood in the stool
E) heartburn and food impaction
A) abdominal pain and hematemesis
B) nausea, vomiting, and postprandial fullness
C) abdominal distention, nausea, and flatulence
D) epigastric pain and blood in the stool
E) heartburn and food impaction

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
26
Major innervation for the enteric nervous system is supplied by parasympathetic and sympathetic fibers of the autonomic nervous system.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
27
LK is a 40-year-old female s/p gastric resection 2 weeks ago due to a perforated ulcer from complicated PUD. Prior to her surgery, she was experiencing severe pain and had an upset stomach. She is now complaining of persistent diarrhea after she eats. 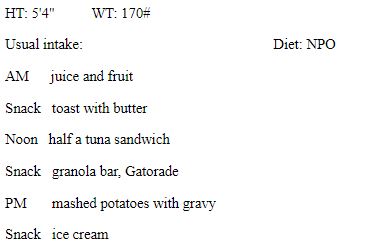
Which medication would most likely be prescribed for LK's condition?
A) clarithromycin
B) atorvastatin calcium
C) niacin
D) bevacizumab
E) amlodipine
Which medication would most likely be prescribed for LK's condition?
A) clarithromycin
B) atorvastatin calcium
C) niacin
D) bevacizumab
E) amlodipine

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
28
LK is a 40-year-old female s/p gastric resection 2 weeks ago due to a perforated ulcer from complicated PUD. Prior to her surgery, she was experiencing severe pain and had an upset stomach. She is now complaining of persistent diarrhea after she eats. 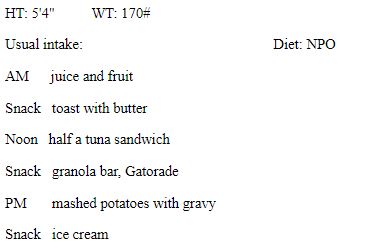
LK would most likely be at risk of which nutrient deficiency?
A) vitamin B6
B) niacin
C) iron
D) potassium
E) phosphorus
LK would most likely be at risk of which nutrient deficiency?
A) vitamin B6
B) niacin
C) iron
D) potassium
E) phosphorus

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
29
The most common symptom related to peptic ulcer disease is:
A) nausea
B) belching
C) epigastric pain
D) anorexia
E) vomiting
A) nausea
B) belching
C) epigastric pain
D) anorexia
E) vomiting

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
30
What describes an appropriate nutrition intervention for a patient following gastric surgery?
A) instruct the patient to lie down after eating
B) increase progression to solid food to avoid dumping syndrome
C) reduce intake from six meals per day to three
D) supplement with folate and vitamin B6
E) advise the patient to consume liquids with meals
A) instruct the patient to lie down after eating
B) increase progression to solid food to avoid dumping syndrome
C) reduce intake from six meals per day to three
D) supplement with folate and vitamin B6
E) advise the patient to consume liquids with meals

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
31
Which gastrointestinal condition is not associated with dysphagia?
A) dumping syndrome
B) achalasia
C) hiatal hernia
D) gastroparesis
E) GERD
A) dumping syndrome
B) achalasia
C) hiatal hernia
D) gastroparesis
E) GERD

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
32
Which of the following describes the purpose of vagotomy?
A) enlargement of the pyloric sphincter
B) elimination of the cholinergic stimulation of the stomach
C) treatment of the jejunum in the small intestine
D) lowering the pressure on the lower esophageal sphincter
E) measurement of the pressure in the small intestine before and after a meal
A) enlargement of the pyloric sphincter
B) elimination of the cholinergic stimulation of the stomach
C) treatment of the jejunum in the small intestine
D) lowering the pressure on the lower esophageal sphincter
E) measurement of the pressure in the small intestine before and after a meal

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
33
LK is a 40-year-old female s/p gastric resection 2 weeks ago due to a perforated ulcer from complicated PUD. Prior to her surgery, she was experiencing severe pain and had an upset stomach. She is now complaining of persistent diarrhea after she eats. 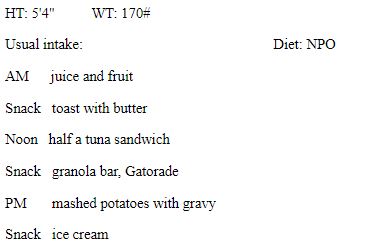 Which nutritional recommendation would be most appropriate for LK?
Which nutritional recommendation would be most appropriate for LK?
Avoiding all desserts and sweets
A) restricting foods that irritate the gastric mucosa
B) allowing plenty of fluids with meals
C) eating 1-3 large meals each day
D) supplementing with folate and magnesium
E) "How . . .?"
 Which nutritional recommendation would be most appropriate for LK?
Which nutritional recommendation would be most appropriate for LK?Avoiding all desserts and sweets
A) restricting foods that irritate the gastric mucosa
B) allowing plenty of fluids with meals
C) eating 1-3 large meals each day
D) supplementing with folate and magnesium
E) "How . . .?"

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
34
Which of the following describes the mechanism of action of metoclopramide in managing nausea?
A) blocking dopamine, which affects the vomiting center in the brain
B) increasing the effectiveness of other antiemetics
C) strengthening the pyloric sphincter to increase gastric emptying
D) reducing the effect of prostaglandins
E) blocking substance P in the brain, which has a direct effect on the vomiting center
A) blocking dopamine, which affects the vomiting center in the brain
B) increasing the effectiveness of other antiemetics
C) strengthening the pyloric sphincter to increase gastric emptying
D) reducing the effect of prostaglandins
E) blocking substance P in the brain, which has a direct effect on the vomiting center

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
35
The most common surgical procedure used for refractory GERD is:
A) a videofluoroscopy swallowing procedure
B) the Roux-en-Y procedure
C) a gastroduodenostomy
D) the Nissen fundoplication
E) a partial gastrectomy with a reconstruction
A) a videofluoroscopy swallowing procedure
B) the Roux-en-Y procedure
C) a gastroduodenostomy
D) the Nissen fundoplication
E) a partial gastrectomy with a reconstruction

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
36
Which is considered a symptom of gastroesophageal reflux in infants?
A) constipation
B) increased food intake
C) dry mucous membranes
D) irritability
E) diarrhea
A) constipation
B) increased food intake
C) dry mucous membranes
D) irritability
E) diarrhea

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
37
LK is a 40-year-old female s/p gastric resection 2 weeks ago due to a perforated ulcer from complicated PUD. Prior to her surgery, she was experiencing severe pain and had an upset stomach. She is now complaining of persistent diarrhea after she eats. 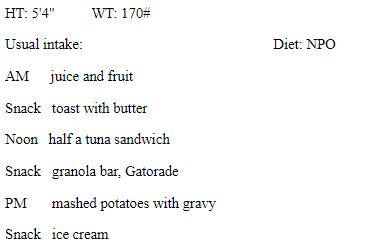
What is the most likely cause of LK's persistent diarrhea?
A) hiatal hernia
B) dumping syndrome
C) dehydration
D) gastroesophageal reflux
E) gastroparesis
What is the most likely cause of LK's persistent diarrhea?
A) hiatal hernia
B) dumping syndrome
C) dehydration
D) gastroesophageal reflux
E) gastroparesis

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
38
The gold standard for diagnosis of gastroparesis is the:
A) upper GI endoscopy
B) endoscopic retrograde cholangiopancreatography (ERCP)
C) endoscopic ultrasound
D) esophagography test
E) scintigraphic gastric emptying test
A) upper GI endoscopy
B) endoscopic retrograde cholangiopancreatography (ERCP)
C) endoscopic ultrasound
D) esophagography test
E) scintigraphic gastric emptying test

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
39
Which is a correct statement regarding late dumping syndrome?
A) It occurs 30-60 minutes after a meal.
B) It is especially common after eating protein.
C) It increases the risk of hypoglycemia.
D) It causes gas, cramping, and diarrhea.
E) It results in sweating, flushing, and dizziness.
A) It occurs 30-60 minutes after a meal.
B) It is especially common after eating protein.
C) It increases the risk of hypoglycemia.
D) It causes gas, cramping, and diarrhea.
E) It results in sweating, flushing, and dizziness.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
40
Which type of food would most likely be recommended during the recovery period after gastric surgery?
A) whole grains
B) potatoes without the skin
C) luncheon meat
D) chocolate milk
E) fruit juice
A) whole grains
B) potatoes without the skin
C) luncheon meat
D) chocolate milk
E) fruit juice

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
41
Medications called _______________, which act to block the effect of acetylcholine, reduce the amount of saliva production as a major side effect.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
42
There is a strong association between obesity and gastroesophageal reflux disease.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
43
Zollinger-Ellison (ZE) syndrome is similar in symptoms to PUD but is typically unresponsive to standard therapy.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
44
Dysgeusia is the complete inability to taste; it is also called "mouth blindness."

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
45
Major innervation for the enteric nervous system is supplied by parasympathetic and sympathetic fibers of the autonomic nervous system. Parasympathetic impulses are carried by the _______________.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
46
The post-gastrectomy diet encourages a well-balanced diet slightly higher in protein and fat.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
47
Control of gastric secretions is accomplished through complementary actions of the nervous and _______________ systems.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
48
For a patient with maxillomandibular fixation, all foods must be prepared so that each easily moves through a _______________.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
49
Several different types of bacteria commonly found in the mouth colonize the surface of the tooth to form plaque.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
50
Achalasia is a condition where the upper portion of the stomach protrudes through the esophagus into the thoracic cavity.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
51
The symptoms of eosinophilic esophagitis experienced by a patient depend on the phase of swallowing that is impaired.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
52
Medicines for high blood pressure and depression often are causes of xerostomia.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
53
The term _______________ refers to an individual without any teeth.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
54
_______________ is fissuring and scaling at the corners or angles of the mouth that may be a sign or symptom of riboflavin, folate, niacin, pyridoxine, vitamin B12, or iron deficiency.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
55
Partially digested food in a semi-fluid state that enters the stomach and small intestine is called _______________.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
56
The Nissen fundoplication for treatment of refractory GERD involves taking the fundus of the _______________ and wrapping it around the lower esophagus.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
57
_______________ ingested when teeth are developing is incorporated into the structure of the enamel and protects it against the action of acids.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
58
The outer layer, or _______________, of tissue for the esophagus is connective tissue and has no additional outer covering.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
59
Pharyngeal and esophageal phases of swallowing take only 3-5 minutes under normal conditions.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
60
Most medications are absorbed in the _______________.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
61
_______________ is the rupture of the esophagus, and a _______________ is a tear of the lower esophageal sphincter caused by forceful vomiting.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
62
For those individuals who are unable to safely swallow or consume adequate nutrition orally because of dysphagia, _______________ feedings should be considered.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
63
Explain manifestations, clinical diagnosis, and treatment interventions of gastroesophageal reflux among infants.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
64
Type A gastritis is a condition most often related to _______________.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
65
List the seven functions of saliva in the oral cavity.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
66
_______________ is an inflammatory condition characterized by infiltration of eosinophils within the esophageal mucosa.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
67
List three examples each of dietary factors that increase the risk of dental caries and those that decrease the risk of dental caries.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
68
_______________ is a motility disorder characterized by an absence of or weakened peristalsis within the esophagus.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
69
Describe the process of swallowing as food moves from the oral cavity to the stomach; include the processes of the four phases of swallowing.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
70
Name four different types of diagnostic procedures that may be used in identifying upper GI pathology.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
71
Describe the process of a focused assessment of the upper gastrointestinal tract for a client, including relevant measurements and subjective data.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
72
Name the four chemical messengers in the stomach that are used to control gastric secretions.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
73
Discuss nutrition therapy used for jaw fracture; include examples of recommended foods.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
74
_______________ involves ulcerations of the gastric or duodenal mucosa that penetrate the submucosa.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
75
The cephalic (head) phase refers to release of _______________ and _______________ when stimulated by tasting, smelling, or even seeing food.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
76
Selective _______________ is a surgical procedure that eliminates innervations from the vagus nerve to parietal cells, resulting in decreased acid production and a decreased response to gastrin.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
77
The purposes of mastication are to break food down into smaller pieces, to mix food with saliva, and:
A) to move food from the front of the mouth to the pharynx
B) to regulate speech patterns
C) to facilitate an immune reaction
D) to provide antibacterial protection
E) to stimulate taste buds
A) to move food from the front of the mouth to the pharynx
B) to regulate speech patterns
C) to facilitate an immune reaction
D) to provide antibacterial protection
E) to stimulate taste buds

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
78
Describe the purpose of the National Dysphagia Diet, and list examples of foods to include from each level.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
79
Describe clinical manifestations of GERD.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck
80
The dysplastic cellular changes associated with Barrett's esophagus are considered to be a precursor to _______________.

Unlock Deck
Unlock for access to all 80 flashcards in this deck.
Unlock Deck
k this deck



