Deck 4: Surgery
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question

Unlock Deck
Sign up to unlock the cards in this deck!
Unlock Deck
Unlock Deck
1/563
Play
Full screen (f)
Deck 4: Surgery
1
An 84-year-old woman comes to the office due to 2 months of bright red bleeding from the rectum. The patient also has intermittent crampy abdominal pain and a 6-kg (13.2-lb) unintentional weight loss. She reports no fevers, tenesmus, chest pain, palpitations, or vomiting. Medical history is significant for obesity and chronic kidney disease. Temperature is 37.6 C (99.7 F), blood pressure is 130/80 mm Hg, and pulse is 70/min. The patient appears cachectic. There is no palpable lymphadenopathy. Cardiac auscultation reveals normal rate and rhythm and no heart murmurs. Lung sounds are normal. The abdomen is nontender and nondistended. Which of the following is the most likely diagnosis?
A)Angiodysplasia
B)Cecal adenocarcinoma
C)Diverticular bleeding
D)Internal hemorrhoids
E)Sigmoid colon adenocarcinoma
A)Angiodysplasia
B)Cecal adenocarcinoma
C)Diverticular bleeding
D)Internal hemorrhoids
E)Sigmoid colon adenocarcinoma
E
Explanation:
This patient has clinical features suspicious for colon cancer. Adenocarcinoma of the colon often presents with fatigue, abdominal pain, and unexpected weight loss, but more specific symptoms are variable and can correlate to the site of the tumor:
Right-sided colon tumors: In the right colon, the lumen is wide, and stool is mostly liquid; obstructive symptoms are uncommon unless the tumor is very large and far advanced. Visible bleeding (ie, hematochezia) can occur but is atypical because blood is diluted by stool before it passes the anal verge. Therefore, adenocarcinoma in the cecum and ascending colon typically presents with occult bleeding and iron-deficiency anemia (Choice B).
Left-sided colon tumors: In the descending and sigmoid colon, tumors may obstruct the flow of stool, leading to crampy or colicky pain and/or a change in bowel habits (eg, constipation). Due to the proximity of these tumors to the anal verge, visible red/maroon hematochezia is common.
Rectal tumors: Bleeding is typically visible as hematochezia or frank red blood. Other symptoms include narrowed stools, tenesmus, and a sensation of a mass in the rectum.
(Choice A) Angiodysplasia is characterized by abnormal dilated and tortuous blood vessels in the intestines. It is most common at age >60 and can present with painless hematochezia or occult bleeding with iron deficiency anemia. This patient's crampy pain and unexpected weight loss are atypical for angiodysplasia.
(Choice C) Diverticular hemorrhage causes acute, self-limited hematochezia that generally lasts up to several days (not months). It is usually painless and does not cause weight loss.
(Choice D) Internal hemorrhoids present with anal pruritus and bright red rectal bleeding, typically on defecation. Crampy pain and weight loss would not be seen.
Educational objective:
Adenocarcinoma in the left side of the colon may obstruct the flow of stool, leading to altered bowel habits; visible hematochezia is common. In contrast, in the right side of the colon, obstructive symptoms are uncommon, and any associated bleeding can be diluted by stool and is less likely to be visible; therefore, right-sided colon cancer often presents with occult bleeding and iron-deficiency anemia.
References:
Clinical assessment to determine the risk of bowel cancer using symptoms, age, mass and iron deficiency anaemia (SAMI).
(http://www.ncbi.nlm.nih.gov/pubmed/28634990)
Explanation:
This patient has clinical features suspicious for colon cancer. Adenocarcinoma of the colon often presents with fatigue, abdominal pain, and unexpected weight loss, but more specific symptoms are variable and can correlate to the site of the tumor:
Right-sided colon tumors: In the right colon, the lumen is wide, and stool is mostly liquid; obstructive symptoms are uncommon unless the tumor is very large and far advanced. Visible bleeding (ie, hematochezia) can occur but is atypical because blood is diluted by stool before it passes the anal verge. Therefore, adenocarcinoma in the cecum and ascending colon typically presents with occult bleeding and iron-deficiency anemia (Choice B).
Left-sided colon tumors: In the descending and sigmoid colon, tumors may obstruct the flow of stool, leading to crampy or colicky pain and/or a change in bowel habits (eg, constipation). Due to the proximity of these tumors to the anal verge, visible red/maroon hematochezia is common.
Rectal tumors: Bleeding is typically visible as hematochezia or frank red blood. Other symptoms include narrowed stools, tenesmus, and a sensation of a mass in the rectum.
(Choice A) Angiodysplasia is characterized by abnormal dilated and tortuous blood vessels in the intestines. It is most common at age >60 and can present with painless hematochezia or occult bleeding with iron deficiency anemia. This patient's crampy pain and unexpected weight loss are atypical for angiodysplasia.
(Choice C) Diverticular hemorrhage causes acute, self-limited hematochezia that generally lasts up to several days (not months). It is usually painless and does not cause weight loss.
(Choice D) Internal hemorrhoids present with anal pruritus and bright red rectal bleeding, typically on defecation. Crampy pain and weight loss would not be seen.
Educational objective:
Adenocarcinoma in the left side of the colon may obstruct the flow of stool, leading to altered bowel habits; visible hematochezia is common. In contrast, in the right side of the colon, obstructive symptoms are uncommon, and any associated bleeding can be diluted by stool and is less likely to be visible; therefore, right-sided colon cancer often presents with occult bleeding and iron-deficiency anemia.
References:
Clinical assessment to determine the risk of bowel cancer using symptoms, age, mass and iron deficiency anaemia (SAMI).
(http://www.ncbi.nlm.nih.gov/pubmed/28634990)
2
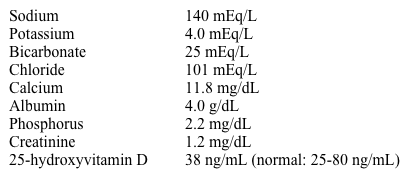
An imaging study detects an incidental 3.5-cm infrarenal abdominal aortic aneurysm in a 70-year-old man. He has no associated symptoms. Medical history is significant for hypertension, type 2 diabetes, and hypercholesterolemia. The patient is maintained on anticoagulation due to paroxysmal atrial fibrillation. He has smoked 1-2 packs of cigarettes a day for the past 40 years, and he drinks 1 or 2 glasses of wine daily. The patient is physically active, bikes regularly, and enjoys hiking. On physical examination, blood pressure is 150/78 mm Hg and pulse is 80/min. Heart sounds are normal, and the lungs are clear. Laboratory results are as follows:  Which of the following is most strongly associated with aneurysm progression in this patient?
Which of the following is most strongly associated with aneurysm progression in this patient?
A)Active smoking
B)Anticoagulation
C)Exercise activities
D)LDL >130 mg/dL
E)Systolic hypertension
F)Uncontrolled diabetes mellitus
 Which of the following is most strongly associated with aneurysm progression in this patient?
Which of the following is most strongly associated with aneurysm progression in this patient?A)Active smoking
B)Anticoagulation
C)Exercise activities
D)LDL >130 mg/dL
E)Systolic hypertension
F)Uncontrolled diabetes mellitus
A
Explanation:
 Abdominal aortic aneurysm (AAA) is generally defined as an enlargement of the abdominal aorta to a diameter ≥3 cm. It is often incidentally detected on imaging, as many patients have no symptoms unless and until rupture occurs. Rupture is more likely with large aneurysmal size (>5.5 cm) or rapid rate of expansion (eg, >1 cm/year), and preemptive surgical repair is the definitive treatment. However, surgery carries a relatively high risk of complication, with the risk of repair typically greater than the risk of rupture until the aneurysm reaches a large size. Therefore, management of small to moderately sized AAA involves surveillance with serial abdominal ultrasound and lifestyle modification to limit AAA progression.
Abdominal aortic aneurysm (AAA) is generally defined as an enlargement of the abdominal aorta to a diameter ≥3 cm. It is often incidentally detected on imaging, as many patients have no symptoms unless and until rupture occurs. Rupture is more likely with large aneurysmal size (>5.5 cm) or rapid rate of expansion (eg, >1 cm/year), and preemptive surgical repair is the definitive treatment. However, surgery carries a relatively high risk of complication, with the risk of repair typically greater than the risk of rupture until the aneurysm reaches a large size. Therefore, management of small to moderately sized AAA involves surveillance with serial abdominal ultrasound and lifestyle modification to limit AAA progression.
Risk factors for AAA include advanced age (eg, >60), smoking, male sex, family history, hypertension, and a history of atherosclerosis or underlying connective tissue disease. Of these, active smoking is the strongest modifiable influence for AAA development and progression. Smoking is believed to disrupt the arterial wall elastin matrix via stimulation of enhanced protease activity, chronic inflammation, and smooth muscle dysfunction, and smoking cessation is considered the best intervention to minimize AAA progression.
Because of the relationship between smoking and AAA, a one-time abdominal ultrasound is recommended to screen for AAA in men ages 65 to 75 with any smoking history.
(Choice B) Anticoagulation has not been shown to either slow or accelerate AAA progression. Patients with AAA who have an appropriate indication for anticoagulation (eg, atrial fibrillation) should remain on it.
(Choices C and D) AAA is considered a coronary artery disease equivalent; therefore, moderate exercise and enhanced lipid control are associated with overall improved cardiovascular outcomes in such patients. However, exercise and lipid control do not limit AAA progression to the same extent as smoking cessation.
(Choice E) AAA is more common in individuals with hypertension, indicating that hypertension may play a role in initial AAA development. However, hypertension, especially isolated systolic hypertension, has not been reliably correlated with AAA progression.
(Choice F) Diabetes is a strong risk factor for atherosclerosis and cardiovascular disease. However, the risk of AAA development and progression is lower in patients with diabetes compared to those without, for reasons that are unclear.
Educational objective:
The management of small to moderately sized (ie, 3 cm to 5.5 cm) abdominal aortic aneurysms (AAAs) involves lifestyle modification, with smoking cessation as the best intervention to minimize AAA progression.
References:
Abdominal aortic aneurysm expansion: risk factors and time intervals for surveillance.
(http://www.ncbi.nlm.nih.gov/pubmed/15210603)
The association between cigarette smoking and abdominal aortic aneurysms.
(http://www.ncbi.nlm.nih.gov/pubmed/10587395)
Association of hypertension with abdominal aortic aneurysm expansion.
(http://www.ncbi.nlm.nih.gov/pubmed/27521823)
Explanation:
 Abdominal aortic aneurysm (AAA) is generally defined as an enlargement of the abdominal aorta to a diameter ≥3 cm. It is often incidentally detected on imaging, as many patients have no symptoms unless and until rupture occurs. Rupture is more likely with large aneurysmal size (>5.5 cm) or rapid rate of expansion (eg, >1 cm/year), and preemptive surgical repair is the definitive treatment. However, surgery carries a relatively high risk of complication, with the risk of repair typically greater than the risk of rupture until the aneurysm reaches a large size. Therefore, management of small to moderately sized AAA involves surveillance with serial abdominal ultrasound and lifestyle modification to limit AAA progression.
Abdominal aortic aneurysm (AAA) is generally defined as an enlargement of the abdominal aorta to a diameter ≥3 cm. It is often incidentally detected on imaging, as many patients have no symptoms unless and until rupture occurs. Rupture is more likely with large aneurysmal size (>5.5 cm) or rapid rate of expansion (eg, >1 cm/year), and preemptive surgical repair is the definitive treatment. However, surgery carries a relatively high risk of complication, with the risk of repair typically greater than the risk of rupture until the aneurysm reaches a large size. Therefore, management of small to moderately sized AAA involves surveillance with serial abdominal ultrasound and lifestyle modification to limit AAA progression.Risk factors for AAA include advanced age (eg, >60), smoking, male sex, family history, hypertension, and a history of atherosclerosis or underlying connective tissue disease. Of these, active smoking is the strongest modifiable influence for AAA development and progression. Smoking is believed to disrupt the arterial wall elastin matrix via stimulation of enhanced protease activity, chronic inflammation, and smooth muscle dysfunction, and smoking cessation is considered the best intervention to minimize AAA progression.
Because of the relationship between smoking and AAA, a one-time abdominal ultrasound is recommended to screen for AAA in men ages 65 to 75 with any smoking history.
(Choice B) Anticoagulation has not been shown to either slow or accelerate AAA progression. Patients with AAA who have an appropriate indication for anticoagulation (eg, atrial fibrillation) should remain on it.
(Choices C and D) AAA is considered a coronary artery disease equivalent; therefore, moderate exercise and enhanced lipid control are associated with overall improved cardiovascular outcomes in such patients. However, exercise and lipid control do not limit AAA progression to the same extent as smoking cessation.
(Choice E) AAA is more common in individuals with hypertension, indicating that hypertension may play a role in initial AAA development. However, hypertension, especially isolated systolic hypertension, has not been reliably correlated with AAA progression.
(Choice F) Diabetes is a strong risk factor for atherosclerosis and cardiovascular disease. However, the risk of AAA development and progression is lower in patients with diabetes compared to those without, for reasons that are unclear.
Educational objective:
The management of small to moderately sized (ie, 3 cm to 5.5 cm) abdominal aortic aneurysms (AAAs) involves lifestyle modification, with smoking cessation as the best intervention to minimize AAA progression.
References:
Abdominal aortic aneurysm expansion: risk factors and time intervals for surveillance.
(http://www.ncbi.nlm.nih.gov/pubmed/15210603)
The association between cigarette smoking and abdominal aortic aneurysms.
(http://www.ncbi.nlm.nih.gov/pubmed/10587395)
Association of hypertension with abdominal aortic aneurysm expansion.
(http://www.ncbi.nlm.nih.gov/pubmed/27521823)
3
A 25-year-old man comes to the office for evaluation of a painless mass in his mouth. The patient has had the mass for many years and has had no growth or other changes in the mass over that time. He has had occasional sinus infections and was in a motor vehicle accident several years ago in which he sustained a concussion, but he is otherwise healthy. The patient smokes a pack of cigarettes a day and drinks 2 or 3 alcoholic beverages on the weekends. Vital signs are normal. Examination of the mass is seen below:  The mass is immobile, nontender, and has a hard consistency. The maxillary and frontal sinuses are nontender, and there is no cervical lymphadenopathy. Which of the following is the most likely cause of this patient's mass?
The mass is immobile, nontender, and has a hard consistency. The maxillary and frontal sinuses are nontender, and there is no cervical lymphadenopathy. Which of the following is the most likely cause of this patient's mass?
A)Congenital anomaly
B)Infectious sequelae
C)Malignant transformation
D)Palatal fracture
E)Vascular malformation
 The mass is immobile, nontender, and has a hard consistency. The maxillary and frontal sinuses are nontender, and there is no cervical lymphadenopathy. Which of the following is the most likely cause of this patient's mass?
The mass is immobile, nontender, and has a hard consistency. The maxillary and frontal sinuses are nontender, and there is no cervical lymphadenopathy. Which of the following is the most likely cause of this patient's mass?A)Congenital anomaly
B)Infectious sequelae
C)Malignant transformation
D)Palatal fracture
E)Vascular malformation
A
Explanation:
This patient has a chronic mass on his hard palate consistent with torus palatinus (TP), a benign bony growth (ie, exostosis) located at the midline suture of the hard palate. It is thought to be caused by both genetic and environmental factors and is more common in women and Asian individuals. TP can be congenital or develop later in life. Similar lesions at the lingual surface of the mandible are termed "tori mandibulari."
TPs are usually <2 cm in size but can gradually enlarge over time. They are typically asymptomatic and are frequently ignored by the patient but noted by clinicians (or family members) when examining the mouth for unrelated reasons. However, the thin epithelium overlying the bony growth may ulcerate with minor trauma of the oral cavity and heal slowly due to poor vascular supply. The diagnosis is usually obvious on clinical grounds. Surgery is indicated for patients in whom the mass becomes symptomatic, interferes with speech or eating, or causes problems with the fitting of dentures later in life.
(Choices B and C) Oral squamous cell carcinoma can be caused by smoking and excessive alcohol use; it can also be a late complication of human papillomavirus infection. However, oral cancer more commonly presents as a progressive ulcerating lesion located eccentrically on soft structures (eg, tongue, lips) rather than the center of the hard palate. Rarely, paranasal sinus infections with atypical organisms (eg, blastomycosis, mucormycosis) can erode into the palate, but this typically occurs in patients with immune suppression (eg, uncontrolled diabetes) and would present acutely.
(Choice D) Chronic complications of palatal fracture include dental malocclusion, temporomandibular joint dysfunction, and complicated wounds. However, palatal fractures are rare, are usually associated with other obvious skull fractures, and are not a major cause of TP.
(Choice E) Maxillofacial vascular malformations are congenital abnormalities that are present at birth. They present as soft, dusky lesions that grow with the patient and may bleed intermittently.
Educational objective:
Torus palatinus (TP) is a benign bony growth (exostosis) located on the midline suture of the hard palate. It can be congenital or develop later in life. TP is typically chronic and asymptomatic, and the diagnosis is usually clinically evident. Surgery is indicated if the mass becomes symptomatic, interferes with speech or eating, or causes problems with the fitting of dentures.
References:
Current status of the torus palatinus and mandibularis.
(http://www.ncbi.nlm.nih.gov/pubmed/19767716)
Explanation:
This patient has a chronic mass on his hard palate consistent with torus palatinus (TP), a benign bony growth (ie, exostosis) located at the midline suture of the hard palate. It is thought to be caused by both genetic and environmental factors and is more common in women and Asian individuals. TP can be congenital or develop later in life. Similar lesions at the lingual surface of the mandible are termed "tori mandibulari."
TPs are usually <2 cm in size but can gradually enlarge over time. They are typically asymptomatic and are frequently ignored by the patient but noted by clinicians (or family members) when examining the mouth for unrelated reasons. However, the thin epithelium overlying the bony growth may ulcerate with minor trauma of the oral cavity and heal slowly due to poor vascular supply. The diagnosis is usually obvious on clinical grounds. Surgery is indicated for patients in whom the mass becomes symptomatic, interferes with speech or eating, or causes problems with the fitting of dentures later in life.
(Choices B and C) Oral squamous cell carcinoma can be caused by smoking and excessive alcohol use; it can also be a late complication of human papillomavirus infection. However, oral cancer more commonly presents as a progressive ulcerating lesion located eccentrically on soft structures (eg, tongue, lips) rather than the center of the hard palate. Rarely, paranasal sinus infections with atypical organisms (eg, blastomycosis, mucormycosis) can erode into the palate, but this typically occurs in patients with immune suppression (eg, uncontrolled diabetes) and would present acutely.
(Choice D) Chronic complications of palatal fracture include dental malocclusion, temporomandibular joint dysfunction, and complicated wounds. However, palatal fractures are rare, are usually associated with other obvious skull fractures, and are not a major cause of TP.
(Choice E) Maxillofacial vascular malformations are congenital abnormalities that are present at birth. They present as soft, dusky lesions that grow with the patient and may bleed intermittently.
Educational objective:
Torus palatinus (TP) is a benign bony growth (exostosis) located on the midline suture of the hard palate. It can be congenital or develop later in life. TP is typically chronic and asymptomatic, and the diagnosis is usually clinically evident. Surgery is indicated if the mass becomes symptomatic, interferes with speech or eating, or causes problems with the fitting of dentures.
References:
Current status of the torus palatinus and mandibularis.
(http://www.ncbi.nlm.nih.gov/pubmed/19767716)
4
A 76-year-old man comes to the office due to constipation. He has infrequent bowel movements associated with straining during defecation. In addition, the patient has intermittent fecal leakage and hematochezia but no melena or unexpected weight loss. Medical history is notable for prostate cancer treated with external beam radiation and brachytherapy 18 months ago. Follow-up CT scans and prostate-specific antigen levels show no evidence of cancer recurrence. Temperature is 37.5 C (99.5 F), blood pressure is 132/80 mm Hg, pulse is 80/min, and respirations are 12/min. Conjunctival pallor is present. Cardiopulmonary examination is unremarkable. The abdomen is soft and nontender. Colonoscopy reveals rectal pallor with areas of mucosal hemorrhage and telangiectasias; the rest of the colon is unremarkable. Which of the following is most likely contributing to this patient's symptoms?
A)Chronic inflammation of the mucosa and submucosa
B)Electrolyte abnormalities
C)Parasympathetic nervous system dysregulation
D)Pelvic floor dyssynergia
E)Progressive rectal fibrosis
A)Chronic inflammation of the mucosa and submucosa
B)Electrolyte abnormalities
C)Parasympathetic nervous system dysregulation
D)Pelvic floor dyssynergia
E)Progressive rectal fibrosis

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
5
A 78-year-old man comes to the office due to lower extremity swelling. He has had progressive exertional dyspnea over the past 2 years. Over the past 2 months, the patient has noticed lower extremity swelling, decreased appetite, and increased abdominal girth. He has a history of poorly controlled hypertension but no known coronary artery disease. The patient is a lifetime nonsmoker. He has no history of prior surgeries. Blood pressure is 165/88 mm Hg and pulse is 72/min and regular. He is afebrile. On physical examination, the jugular veins are distended and there are prominent V waves. A holosystolic murmur is heard at the lower sternal border, and there is 3+ pitting edema of the lower extremities bilaterally. Which of the following best explains the physical examination findings in this patient?
A)Dilation of the pulmonary arteries
B)Dilation of the tricuspid valve annulus
C)Flailing of a tricuspid valve leaflet
D)Fusion of the tricuspid valve commissures
E)Increased intrapericardial pressure
A)Dilation of the pulmonary arteries
B)Dilation of the tricuspid valve annulus
C)Flailing of a tricuspid valve leaflet
D)Fusion of the tricuspid valve commissures
E)Increased intrapericardial pressure

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
6
A 42-year-old man comes to the office to discuss abnormal blood work results that were obtained at a local health fair. The patient currently feels well and reports no symptoms. Temperature is 37.6 C (99.7 F), blood pressure is 125/72 mm Hg, pulse is 82/min, and respirations are 13/min. Examination shows no scleral icterus. Heart and lung sounds are normal; skin and abdominal examination are normal. Laboratory results are as follows:  Right upper quadrant ultrasound is normal. The patient undergoes magnetic resonance cholangiopancreatography, which reveals luminal irregularities with mild focal dilatations within both intrahepatic and extrahepatic biliary ducts. Which of the following additional testing should be obtained from this patient?
Right upper quadrant ultrasound is normal. The patient undergoes magnetic resonance cholangiopancreatography, which reveals luminal irregularities with mild focal dilatations within both intrahepatic and extrahepatic biliary ducts. Which of the following additional testing should be obtained from this patient?
A)Colonoscopy
B)Echocardiogram
C)Ocular slit-lamp examination
D)Pulmonary function tests
E)Serum ferritin levels
 Right upper quadrant ultrasound is normal. The patient undergoes magnetic resonance cholangiopancreatography, which reveals luminal irregularities with mild focal dilatations within both intrahepatic and extrahepatic biliary ducts. Which of the following additional testing should be obtained from this patient?
Right upper quadrant ultrasound is normal. The patient undergoes magnetic resonance cholangiopancreatography, which reveals luminal irregularities with mild focal dilatations within both intrahepatic and extrahepatic biliary ducts. Which of the following additional testing should be obtained from this patient?A)Colonoscopy
B)Echocardiogram
C)Ocular slit-lamp examination
D)Pulmonary function tests
E)Serum ferritin levels

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
7
A 62-year-old man comes to the office due to anorexia, fatigue, and a 9 kg (20 lb) weight loss over the past 6 months. He rarely drinks alcohol and does not use illicit drugs, although he has smoked one pack of cigarettes daily for the past 40 years. The patient has previously been diagnosed with hypertension, diverticulosis, external hemorrhoids, and osteoarthritis. Current medications are atenolol and aspirin, and he has no known drug allergies. Temperature is 37 C (98.6 F), blood pressure is 132/88 mm Hg, pulse is 70/min, and respirations are 12/min. Physical examination reveals a soft abdomen that is mildly tender to deep palpation in the midepigastric region. The sclerae are icteric, and the skin is jaundiced. Laboratory results show:  Antimitochondrial antibodies are negative. Abdominal ultrasound demonstrates mild dilation of the common bile duct; there are no stones present in the gallbladder and no evidence of gallbladder wall thickening. Which of the following is the best next step in the management of this patient's condition?
Antimitochondrial antibodies are negative. Abdominal ultrasound demonstrates mild dilation of the common bile duct; there are no stones present in the gallbladder and no evidence of gallbladder wall thickening. Which of the following is the best next step in the management of this patient's condition?
A)Abdominal CT scan
B)Endoscopic retrograde pancreatography (ERCP)
C)Percutaneous transhepatic cholangiogram (PTC)
D)Serum amylase and lipase
E)Serum CA 19-9
 Antimitochondrial antibodies are negative. Abdominal ultrasound demonstrates mild dilation of the common bile duct; there are no stones present in the gallbladder and no evidence of gallbladder wall thickening. Which of the following is the best next step in the management of this patient's condition?
Antimitochondrial antibodies are negative. Abdominal ultrasound demonstrates mild dilation of the common bile duct; there are no stones present in the gallbladder and no evidence of gallbladder wall thickening. Which of the following is the best next step in the management of this patient's condition?A)Abdominal CT scan
B)Endoscopic retrograde pancreatography (ERCP)
C)Percutaneous transhepatic cholangiogram (PTC)
D)Serum amylase and lipase
E)Serum CA 19-9

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
8
A 61-year-old woman comes to the office due to 3 months of constipation and pain in the left lower abdomen. The pain is crampy, continuous, and nonradiating and is not affected by bowel movements or meals. The patient reports hard, pelletlike stools and early satiety but no vomiting, hematochezia, melena, or weight changes. The patient does not have a history of chronic constipation. She is postmenopausal and has not had a period in >5 years. Medical history is significant for hypertension. Family history is unremarkable, and the patient does not use tobacco or alcohol. Temperature is 37.5 C (99.5 F), blood pressure is 145/87 mm Hg, pulse is 80/min, and respirations are 12/min. No scleral icterus or palpable lymphadenopathy is present. Cardiopulmonary examination is unremarkable. The abdomen is mildly distended and tender to palpation in the left lower quadrant without rebound or guarding. Rectal examination is unremarkable and negative for fecal occult blood. Colonoscopy results are unremarkable. Which of the following is the best next step in management?
A)Abdominal x-ray
B)Barium enema
C)Biofeedback therapy
D)Fiber supplementation
E)Pelvic floor muscle exercises
F)Pelvic ultrasound
A)Abdominal x-ray
B)Barium enema
C)Biofeedback therapy
D)Fiber supplementation
E)Pelvic floor muscle exercises
F)Pelvic ultrasound

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
9
A 56-year-old man comes to the office for evaluation of a gradually enlarging, painless mass above the right angle of the jaw. He has also recently experienced right-sided facial weakness. When he was in his 20s, the patient had Hodgkin disease that was treated with radiation to the neck. Family history is significant for thyroid cancer in his mother. The patient does not use tobacco, alcohol, or illicit drugs. He had several male and female sexual partners in his 30s but has been sexually active with only one partner for the past 15 years. Vital signs are within normal limits. Physical examination shows a firm, nontender mass in the right parotid gland and weakness of all right-sided facial muscles. Which of the following is most concerning for malignancy in this patient?
A)Exposure to oncogenic virus
B)Family history of malignancy
C)Lack of salivary gland pain
D)Origin from parotid gland
E)Presence of facial droop
A)Exposure to oncogenic virus
B)Family history of malignancy
C)Lack of salivary gland pain
D)Origin from parotid gland
E)Presence of facial droop

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
10
A 55-year-old man comes to the office for follow-up due to recurrent episodes of jaw pain. The patient's most recent episode was a week ago. He had pain that worsened with eating, accompanied by a tender mass under the left jaw and fever. All symptoms resolved within a few days with oral antibiotic treatment. This was the third episode in the past year. Which of the following is the most likely underlying reason for this patient's recurrent episodes of jaw pain?
A)Giant cell arteritis
B)Sialolithiasis
C)Sjögren syndrome
D)Temporomandibular joint disease
E)Trigeminal neuralgia
A)Giant cell arteritis
B)Sialolithiasis
C)Sjögren syndrome
D)Temporomandibular joint disease
E)Trigeminal neuralgia

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
11
A 42-year-old man with a history of Crohn disease comes to the office for follow-up. He had a partial ileal resection due to a stricture and also had multiple surgeries to treat an enterocutaneous fistula. The patient has received parenteral nutrition for the past several weeks and recently restarted oral feeding. He reports nonbloody diarrhea but no fever or abdominal pain. The patient says that food does not taste the same as before. On examination, he has patchy alopecia and a pustular, crusting skin rash with scaling and erythema around the mouth and on the extremities. No abdominal tenderness is present and bowel sounds are normal. The jugular venous pulse is normal and there is no lower extremity edema. Which of the following is most likely to improve this patient's current condition?
A)Elemental copper
B)Gluten avoidance
C)Niacin therapy
D)Selenium supplement
E)Zinc supplement
A)Elemental copper
B)Gluten avoidance
C)Niacin therapy
D)Selenium supplement
E)Zinc supplement

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
12
A 56-year-old man comes to the office due to a right foot ulcer that is not healing. He first noticed a small wound on the right sole 2 weeks ago but does not remember any trauma. The patient applied over-the-counter antibiotic cream, but the wound gradually enlarged and began draining foul-smelling material. He has had no fever or significant pain. The patient has a history of hypertension and type 2 diabetes mellitus. Temperature is 37.2 C (99 F), blood pressure is 140/80 mm Hg, and pulse is 86/min. Right foot examination shows a 2×3 cm plantar ulcer under the first metatarsal head. There is purulent exudate and the bone can be palpated with a sterile metal probe. Distal pulses are present, but lower-extremity sensation to light touch and pain is decreased. A recent hemoglobin A1c level is 8.9%. Which of the following is the best next step in management of this patient's foot ulcer?
A)Amputation of the foot
B)Erythrocyte sedimentation rate
C)Fungal blood cultures
D)Metatarsal bone biopsy
E)Swab and culture from the wound base
A)Amputation of the foot
B)Erythrocyte sedimentation rate
C)Fungal blood cultures
D)Metatarsal bone biopsy
E)Swab and culture from the wound base

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
13
A 54-year-old woman comes to the emergency department due to bright red blood per rectum. She reports passing 3 large, bloody stools over the past 2 days, which have been associated with mild abdominal cramps. The patient has no melena, fever, vomiting, or unexpected weight changes. She underwent a radical hysterectomy and adjuvant radiation therapy for cervical cancer over 12 months ago. The patient has no other medical conditions and takes no medication. Temperature is 37.5 C (99.5 F), blood pressure is 140/80 mm Hg, pulse is 80/min, and respirations are 12/min. Cardiopulmonary examination is unremarkable. The abdomen is nontender and nondistended. Extremities are warm and well perfused. Laboratory results are as follows:  A colonoscopy is performed and shows mucosal pallor, friability, and multiple telangiectasias, all of which are confined within the rectum. Scattered diverticula are present but limited to the descending and transverse colon. Which of the following is the most likely diagnosis?
A colonoscopy is performed and shows mucosal pallor, friability, and multiple telangiectasias, all of which are confined within the rectum. Scattered diverticula are present but limited to the descending and transverse colon. Which of the following is the most likely diagnosis?
A)Angiodysplasia
B)Clostridioides difficile infection
C)Crohn disease
D)Diverticular colitis
E)Ischemic colitis
F)Radiation proctitis
 A colonoscopy is performed and shows mucosal pallor, friability, and multiple telangiectasias, all of which are confined within the rectum. Scattered diverticula are present but limited to the descending and transverse colon. Which of the following is the most likely diagnosis?
A colonoscopy is performed and shows mucosal pallor, friability, and multiple telangiectasias, all of which are confined within the rectum. Scattered diverticula are present but limited to the descending and transverse colon. Which of the following is the most likely diagnosis?A)Angiodysplasia
B)Clostridioides difficile infection
C)Crohn disease
D)Diverticular colitis
E)Ischemic colitis
F)Radiation proctitis

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
14
A 40-year-old man comes to the office for follow-up of hypertension. He was diagnosed with mild hypertension 6 months ago and has had good control with regular exercise and weight loss. The patient feels well and takes no medications. He does not smoke and drinks a few glasses of wine per week. The patient's medical history is otherwise unremarkable. His mother has osteoporosis that is treated with oral alendronate. On examination, inspection and palpation of the neck show no masses. Laboratory results are as follows: 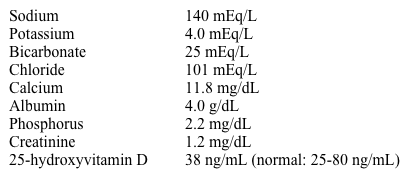 Serum parathyroid hormone level is 814 pg/mL. Further testing shows a high 24-hour urine calcium excretion of 325 mg. DXA scan reveals normal bone mineral density. Renal ultrasound shows multiple small (<5 mm) stones in both kidneys. Which of the following is the most appropriate next step in management of this patient?
Serum parathyroid hormone level is 814 pg/mL. Further testing shows a high 24-hour urine calcium excretion of 325 mg. DXA scan reveals normal bone mineral density. Renal ultrasound shows multiple small (<5 mm) stones in both kidneys. Which of the following is the most appropriate next step in management of this patient?
A)Initiate bisphosphonate therapy
B)Obtain CT scan of the chest, abdomen, and pelvis
C)Refer for parathyroid imaging and parathyroidectomy
D)Repeat serum calcium measurement in 3-6 months
E)Start vitamin D supplementation
 Serum parathyroid hormone level is 814 pg/mL. Further testing shows a high 24-hour urine calcium excretion of 325 mg. DXA scan reveals normal bone mineral density. Renal ultrasound shows multiple small (<5 mm) stones in both kidneys. Which of the following is the most appropriate next step in management of this patient?
Serum parathyroid hormone level is 814 pg/mL. Further testing shows a high 24-hour urine calcium excretion of 325 mg. DXA scan reveals normal bone mineral density. Renal ultrasound shows multiple small (<5 mm) stones in both kidneys. Which of the following is the most appropriate next step in management of this patient?A)Initiate bisphosphonate therapy
B)Obtain CT scan of the chest, abdomen, and pelvis
C)Refer for parathyroid imaging and parathyroidectomy
D)Repeat serum calcium measurement in 3-6 months
E)Start vitamin D supplementation

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
15
A 55-year-old man comes to the office due to progressive abdominal distension for the past 2 months. He reports that his abdomen has become so large that his clothes no longer fit. Temperature is 37.5 C (99.5 F), blood pressure is 152/87 mm Hg, pulse is 80/min, and respirations are 18/min. The abdomen is grossly enlarged and nontender. Shifting dullness is present. Trace pitting edema is identified in the bilateral lower extremities. Paracentesis reveals bloody ascitic fluid. Repeat paracentesis from another site yields similar bloody fluid. Which of the following is most likely responsible for this patient's presentation?
A)Hepatocellular carcinoma
B)Nephrotic syndrome
C)Portal vein thrombosis
D)Spontaneous bacterial peritonitis
E)Tuberculosis
A)Hepatocellular carcinoma
B)Nephrotic syndrome
C)Portal vein thrombosis
D)Spontaneous bacterial peritonitis
E)Tuberculosis

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
16
A 54-year-old man comes to the office after a year of progressive fatigue and frequent loose stools. He describes voluminous, foul-smelling stools that float and are difficult to flush. The patient has lost about 9 kg (20 lbs) in the past 6 months. He was hospitalized on multiple occasions several years ago for epigastric pain radiating to the back, nausea, and vomiting. Lately, the patient has had intermittent episodes of similar pain lasting for 15-30 minutes after meals. He has had no hematemesis, hematochezia, or melena. The patient stopped drinking alcohol several years ago and does not use tobacco or recreational drugs. Temperature is 37 C (98.6 F), blood pressure is 118/80 mm Hg, and pulse is 78/min. BMI is 19.5 kg/m2. Abdominal examination shows epigastric tenderness on deep palpation. Bowel sounds are normal. Which of the following is most likely to improve this patient's symptoms?
A)Antimicrobial therapy
B)Cholecystectomy and stone removal
C)Gluten-free diet
D)Helicobacter pylori eradication
E)Mesenteric angioplasty
F)Pancreatic enzyme supplementation
G)Restriction of dairy products
A)Antimicrobial therapy
B)Cholecystectomy and stone removal
C)Gluten-free diet
D)Helicobacter pylori eradication
E)Mesenteric angioplasty
F)Pancreatic enzyme supplementation
G)Restriction of dairy products

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
17
A 72-year-old man comes to the hospital due to several episodes of bright red blood per rectum. He also has dizziness and severe fatigue. The patient has never had prior episodes of gastrointestinal bleeding. He takes lisinopril and amlodipine for hypertension. The patient is a lifetime nonsmoker. Laboratory evaluation reveals decreased levels of von Willebrand factor multimers but a normal platelet count. Upper endoscopy and colonoscopy do not identify a source of bleeding. Which of the following is most likely associated with this patient's condition?
A)Calcific aortic stenosis
B)Chronic liver disease
C)Glucose intolerance
D)Uncontrolled hypertension
E)Vitamin B12 deficiency
A)Calcific aortic stenosis
B)Chronic liver disease
C)Glucose intolerance
D)Uncontrolled hypertension
E)Vitamin B12 deficiency

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
18
A 50-year-old man comes to the office due to a 4-month history of achy joint pain in the lower back, shoulders, hips, and knees. The pain increases with activity, and he has no morning stiffness. The patient also has excessive sweating, polyuria, and erectile dysfunction. Medical history is unremarkable. The patient has a 25-pack-year smoking history and drinks moderate amounts of alcohol on social occasions. Blood pressure is 150/90 mm Hg, pulse is 80/min, and respirations are 16/min. Examination shows crepitus on passive movement of the knee joints. There is increased interdental spacing and an enlarged tongue, and the remainder of the examination is normal. Plain radiography of the hand reveals widening of the joint spaces, osteophytes, and thickened soft tissues. Laboratory evaluation reveals low testosterone and hyperglycemia. What is the most likely diagnosis?
A)Acromegaly
B)Amyloidosis
C)Hemochromatosis
D)Paget disease of bone
E)Paraneoplastic syndrome
A)Acromegaly
B)Amyloidosis
C)Hemochromatosis
D)Paget disease of bone
E)Paraneoplastic syndrome

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
19
A 36-year-old woman comes to the office due to intermittent abdominal pain. She has had 5 episodes of pain over the past several weeks. The pain is dull, is located in the right upper quadrant and epigastrium, and often radiates to her back. The pain occurs only after eating and lasts 30-60 minutes. It is not relieved by antacids. The pain is occasionally associated with nausea and vomiting, but the patient has no hematemesis, melena, or weight loss. She does not use nonsteroidal anti-inflammatory drugs, tobacco, or alcohol. Her father died of pancreatic cancer at age 64. Temperature is 37.5 C (99.5 F), blood pressure is 142/89 mm Hg, pulse is 67/min, and respirations are 12/min. BMI is 32 kg/m2. The abdomen is tender to palpation in the right upper quadrant and epigastrium but is nondistended and without rebound or guarding. Laboratory results are as follows:  Which of the following is the best next step in management of this patient?
Which of the following is the best next step in management of this patient?
A)Abdominal ultrasound
B)Abdominal x-ray
C)CT scan of the abdomen
D)Helicobacter pylori stool antigen test
E)HIDA scan
F)Upper gastrointestinal endoscopy
 Which of the following is the best next step in management of this patient?
Which of the following is the best next step in management of this patient?A)Abdominal ultrasound
B)Abdominal x-ray
C)CT scan of the abdomen
D)Helicobacter pylori stool antigen test
E)HIDA scan
F)Upper gastrointestinal endoscopy

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
20
A 68-year-old woman comes to the office due to food getting "stuck" in her throat, which has worsened over the past 2 years. She occasionally has to get out of bed to vomit, although she does not vomit during the day. She has not changed her diet or lost weight. Medical history includes obesity, hypertension, and diabetes. A barium esophagogram is shown in the image below. Which of the following is the most appropriate next step in management of this patient? 
A)Cricopharyngeal myotomy
B)Esophageal balloon dilation
C)Ligamentum arteriosum ligation
D)Oral metoclopramide
E)Oral omeprazole
F)Swallowing rehabilitation

A)Cricopharyngeal myotomy
B)Esophageal balloon dilation
C)Ligamentum arteriosum ligation
D)Oral metoclopramide
E)Oral omeprazole
F)Swallowing rehabilitation

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
21
A 56-year-old woman comes to the office due to eye irritation, painful eye movements, and diplopia. Over the last few weeks, she has also experienced weight loss and fatigue. The patient smokes a pack of cigarettes a day and has a 25-pack-year history. Other medical problems include chronic obstructive pulmonary disease treated with an inhaled corticosteroid and bronchodilators. She also suffered a head injury in a motor vehicle accident 6 months ago. Blood pressure is 146/70 mm Hg, pulse is 110/min, and respirations are 18/min. On physical examination, the patient is unable to maintain eye convergence and experiences diplopia on upward gaze. Her eyes are shown in the image below.  Which of the following is the most likely cause of this patient's examination findings?
Which of the following is the most likely cause of this patient's examination findings?
A)Brain stem injury
B)Increased intracranial pressure
C)Increased intraocular pressure
D)Neuromuscular junction disorder
E)Orbital tissue expansion
F)Paraneoplastic syndrome
 Which of the following is the most likely cause of this patient's examination findings?
Which of the following is the most likely cause of this patient's examination findings?A)Brain stem injury
B)Increased intracranial pressure
C)Increased intraocular pressure
D)Neuromuscular junction disorder
E)Orbital tissue expansion
F)Paraneoplastic syndrome

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
22
A 67-year-old man was hospitalized yesterday following elective right knee arthroplasty for osteoarthritis. Medical history is notable for hypertension, type 2 diabetes, and coronary artery disease; the patient is receiving chronic antiplatelet therapy with clopidogrel, which was stopped 5 days prior to surgery. The procedure was performed under anesthesia via epidural and femoral nerve block, and no intraoperative complications were noted. Following surgery, patient-controlled analgesia was provided for pain control, and prophylactic enoxaparin was given beginning 12 hours after surgery completion. Today, the patient has had difficulty urinating after removal of the urinary catheter, as well as low back pain and numbness in the legs. Examination shows tenderness at the insertion site of the epidural catheter. The knee incision is clean with no bleeding or drainage. There is weakness of right plantar flexion and dorsiflexion. Sensation is decreased in the anterior thigh and leg bilaterally. Which of the following is the best next step in management of this patient?
A)Compartment pressure measurement
B)Discontinuation of opiate analgesics
C)MRI of the lumbosacral spine
D)Nerve conduction study
E)Reassurance and follow-up
A)Compartment pressure measurement
B)Discontinuation of opiate analgesics
C)MRI of the lumbosacral spine
D)Nerve conduction study
E)Reassurance and follow-up

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
23
A 78-year-old woman comes to the office due to worsening clumsiness and weakness of her hands for the past several months. The patient has had difficulty performing daily activities such as buttoning shirts or tightly holding garden tools. She also reports stiffness in her legs and neck. Medical history is significant for hypertension and osteoarthritis. Physical examination shows bony outgrowth at distal and proximal interphalangeal joints. There is wasting of the intrinsic hand muscles, and grip strength is decreased bilaterally. Neck flexion elicits an electric shock-like sensation down the patient's back. Ankle reflexes are 3+ bilaterally. Which of the following is the most likely diagnosis?
A)Amyotrophic lateral sclerosis
B)Inflammatory myopathy
C)Multiple sclerosis
D)Spinal cord compression
E)Ulnar neuropathy
A)Amyotrophic lateral sclerosis
B)Inflammatory myopathy
C)Multiple sclerosis
D)Spinal cord compression
E)Ulnar neuropathy

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
24
A 62-year-old woman is brought to the emergency department by her family due to dizziness. She was unable to get out of bed and go to the bathroom this morning and has had headache and nausea. The patient has a history of migraine headaches and hypertension. Six months ago, she had an episode of transient right-sided vision loss and was prescribed aspirin. Other medications include amlodipine and hydrochlorothiazide. Temperature is 36.7 C (98.1 F), blood pressure is 156/72 mm Hg, and pulse is 88/min. BMI is 33 kg/m2. On physical examination, the patient moves all extremities, and deep tendon reflexes are symmetric. CT scan of the head is shown in the image. The patient is admitted to the hospital. An hour after admission, she appears lethargic but follows simple commands. She had a single episode of vomiting in the emergency department. Which of the following is the best next step in management of this patient?
A)Anticoagulation
B)Intravenous corticosteroids
C)Loop diuretics
D)Lumbar puncture
E)Surgery
A)Anticoagulation
B)Intravenous corticosteroids
C)Loop diuretics
D)Lumbar puncture
E)Surgery

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
25
A 75-year-old man comes to the clinic due to a gradual onset of blurred vision in both eyes and difficulty reading over the past 2 months. He also has difficulty driving at night and reports seeing halos around bright lights. Medical history is notable for longstanding diabetes and hypertension. The patient has a 40 pack-year smoking history. Vital signs are normal. Corrected vision is OD (right eye) 20/80 and OS (left eye) 20/100 with normal findings on visual field testing. Which of the following is the most likely diagnosis in this patient?
A)Cataracts
B)Diabetic retinopathy
C)Hypertensive retinopathy
D)Macular degeneration
E)Open-angle glaucoma
A)Cataracts
B)Diabetic retinopathy
C)Hypertensive retinopathy
D)Macular degeneration
E)Open-angle glaucoma

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
26
A 5-year-old boy is brought to the emergency department due to right-sided hemiplegia. His parents say that he has been having increasing difficulty moving his right arm and leg over the past 3 hours. This morning, approximately 10 hours prior, the child tripped on a toy while brushing his teeth and fell forward with the toothbrush in his mouth. He cried immediately, but his parents did not note any oral bleeding. The boy did say, "My throat hurts" throughout the day but was able to eat his lunch. The child has a history of attention deficit hyperactivity disorder for which he takes methylphenidate. The boy's mother has a history of migraines, and his grandfather had a stroke at age 62. Neurologic examination shows right hemiplegia, right hemianesthesia, and mild motor aphasia. Which of the following is the most likely cause of this patient's condition?
A)Antithrombin III deficiency
B)Arteriovenous malformation
C)Carotid artery dissection
D)Congenital heart disease
E)Focal seizure
F)Hemiplegic migraine
G)Homocystinuria
H)Retropharyngeal abscess
A)Antithrombin III deficiency
B)Arteriovenous malformation
C)Carotid artery dissection
D)Congenital heart disease
E)Focal seizure
F)Hemiplegic migraine
G)Homocystinuria
H)Retropharyngeal abscess

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
27
A 46-year-old woman comes to the office due to tingling, numbness, and weakness of the left upper extremity. The patient experienced left shoulder and subscapular pain during a vacation 1 month ago, which she attributed to sleeping on a new bed. She saw a chiropractor upon returning and has taken ibuprofen as needed. Over the past 3 weeks, she has also experienced tingling and numbness in her left hand and has had mild left arm weakness. The patient spends prolonged time answering the phone at work and has noticed the symptoms worsen after cradling the phone between the head and the left shoulder. She has a history of hypothyroidism and takes levothyroxine. Vital signs are within normal limits. Physical examination shows loss of pinprick sensation in the left thumb and index finger. There is mild weakness of the elbow flexion and biceps reflex is decreased on the left side. Which of the following is the most likely cause of this patient's symptoms?
A)Median nerve compression
B)Peripheral nerve demyelination
C)Spinal cord demyelination
D)Spinal nerve root compression
E)Ulnar nerve compression
A)Median nerve compression
B)Peripheral nerve demyelination
C)Spinal cord demyelination
D)Spinal nerve root compression
E)Ulnar nerve compression

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
28
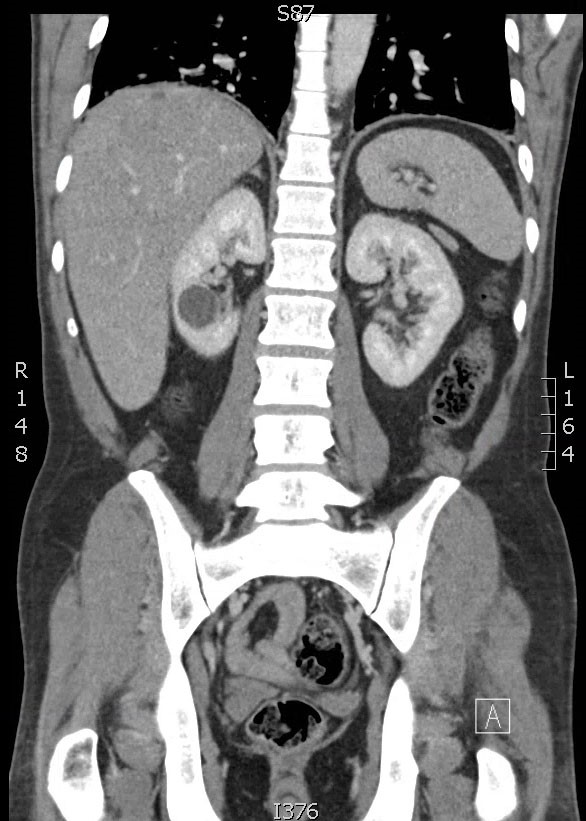
A 54-year-old man comes to the emergency department with cramping lower abdominal pain, mild nausea, and 2 episodes of watery diarrhea. The patient has no fever, vomiting, or urinary symptoms. His past medical history is unremarkable. The patient's father died at age 60 from abdominal aortic aneurysm rupture. He is a lifetime nonsmoker. His vital signs are normal. CT scan of the abdomen with contrast is shown in the image below: 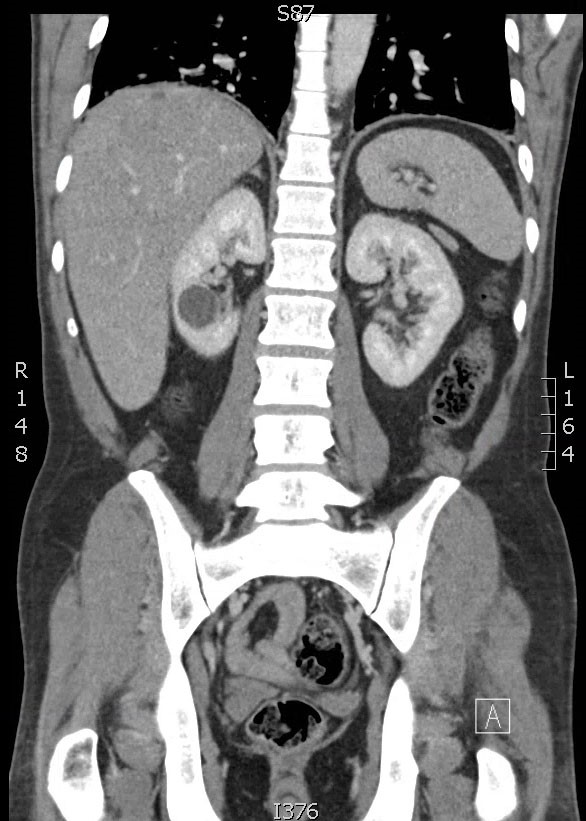 All gastrointestinal symptoms resolve in 2 hours without any intervention, and the patient wants to go home. Which of the following is the most appropriate management for the renal findings on the CT scan?
All gastrointestinal symptoms resolve in 2 hours without any intervention, and the patient wants to go home. Which of the following is the most appropriate management for the renal findings on the CT scan?
A)Antibiotics
B)Percutaneous aspiration
C)Reassurance only
D)Surgical excision
E)Ureteral stent placement
 All gastrointestinal symptoms resolve in 2 hours without any intervention, and the patient wants to go home. Which of the following is the most appropriate management for the renal findings on the CT scan?
All gastrointestinal symptoms resolve in 2 hours without any intervention, and the patient wants to go home. Which of the following is the most appropriate management for the renal findings on the CT scan?A)Antibiotics
B)Percutaneous aspiration
C)Reassurance only
D)Surgical excision
E)Ureteral stent placement

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
29
A 23-year-old man comes to the emergency department after injuring his right shoulder during a basketball game. He was trying to block a shot when his abducted and externally rotated arm was forced backward by an opposing player. The patient immediately felt excruciating pain and fell to the ground holding his right arm. He has no other medical conditions and has never had a similar injury. On examination, there is gross asymmetry of the right shoulder compared to the left, and the right arm is held in slight abduction and external rotation. Distal pulses are full. Plain film x-ray of the right shoulder is shown below. 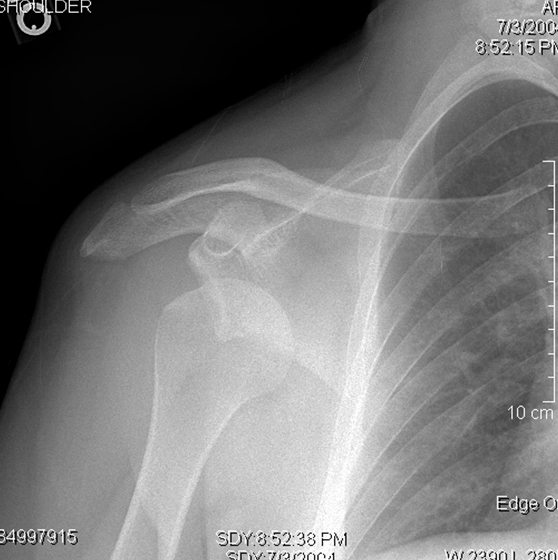 If left untreated, which of the following is the most likely complication of this patient's injury?
If left untreated, which of the following is the most likely complication of this patient's injury?
A)Inability to extend fingers
B)Loss of the biceps reflex
C)Numbness of the medial 2 fingers
D)Shoulder abduction weakness
E)Winging of the scapula
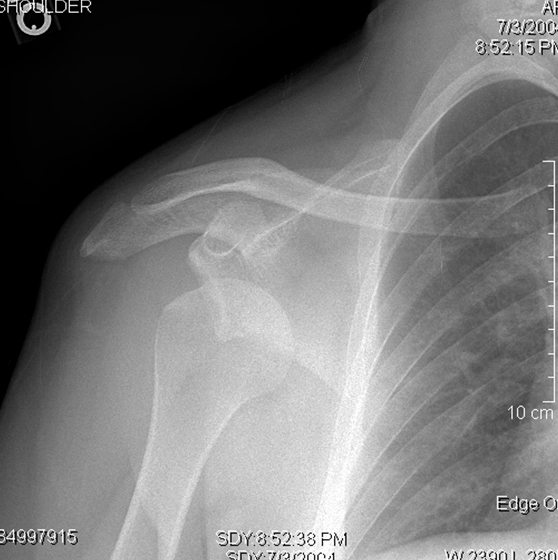 If left untreated, which of the following is the most likely complication of this patient's injury?
If left untreated, which of the following is the most likely complication of this patient's injury?A)Inability to extend fingers
B)Loss of the biceps reflex
C)Numbness of the medial 2 fingers
D)Shoulder abduction weakness
E)Winging of the scapula

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
30
A 46-year-old man is hospitalized after a motorcycle collision. The patient was thrown several feet and was found unconscious by the emergency medical team. On arrival at the emergency department, blood pressure is 160/100 mm Hg, pulse is 58/min, and respirations are 10/min and irregular. The patient does not answer questions or open his eyes to voice or touch. He withdraws all extremities to pain but has no purposeful movements. Pupils are symmetric and sluggish. Bilateral breath sounds are normal. There are abrasions on the face and extremities. Endotracheal intubation is performed for airway protection. Imaging of the head and cervical spine shows no intracranial hematomas, fractures, or dislocations, but diffuse cerebral edema is present. Which of the following is the best initial intervention for reducing intracranial pressure in this patient?
A)Glucocorticoid therapy
B)Hypertonic saline
C)Lumbar puncture
D)Nimodipine
A)Glucocorticoid therapy
B)Hypertonic saline
C)Lumbar puncture
D)Nimodipine

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
31
A 67-year-old man comes to the office due to slowly worsening fatigue and shortness of breath. The symptoms began after a chest cold 8 months ago. Medical history is significant for type 2 diabetes mellitus, for which the patient takes metformin. He has a 25-pack-year smoking history and quit 2 years ago. The patient is a retired attorney. He started taking trumpet lessons 3 months ago. Temperature is 36.6 C (97.9 F), blood pressure is 122/80 mm Hg, pulse is 70/min, and respirations are 16/min. Oxygen saturation is 96% on room air. Heart sounds are normal. Pulmonary examination demonstrates fine inspiratory crackles. Muscle strength is 5/5 throughout. The joints appear normal with full range of motion. Skin examination is normal. A high-resolution CT scan of the chest reveals lower lobe subpleural honeycombing and reticular markings greatest at the periphery. Pulmonary function tests demonstrate moderate restriction and reduced diffusion lung capacity for carbon monoxide. Hemoglobin A1c is 8.2%. All other laboratory test results are within normal limits. What is the most appropriate therapy for this patient?
A)Antifibrotic therapy
B)Corticosteroid-based immunosuppression
C)Exposure avoidance
D)Noncorticosteroid-based immunosuppression
E)Referral for hospice care
A)Antifibrotic therapy
B)Corticosteroid-based immunosuppression
C)Exposure avoidance
D)Noncorticosteroid-based immunosuppression
E)Referral for hospice care

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
32
A 74-year-old man is evaluated for acute agitation beginning 20 minutes after arrival to the post-anesthesia care unit (PACU) following abdominal surgery. He was admitted 5 days ago for a small bowel obstruction and failed nonoperative management. The patient received lorazepam for preoperative anxiety, and lysis of adhesions was performed under general anesthesia. His immediate postoperative course was uneventful, and he was responsive and following commands shortly after extubation and on arrival to the PACU. Medical history is significant for posttraumatic stress disorder. Temperature is 37.2 C (99 F), blood pressure is 142/86 mm Hg, pulse is 98/min, and respirations are 18/min. The patient is anxious, confused, and restless in bed. He now responds only to questions in Spanish despite being fluent in English minutes before. His muscles seem tense, but screening neurologic examination reveals no focal abnormalities. Arterial blood gas shows PaO2 of 86 mm Hg and PaCO2 of 38 mm Hg. Point-of-care electrolytes, glucose, and hematocrit are all normal. What is the most appropriate initial management of this patient?
A)Administer dantrolene
B)Administer lorazepam
C)Apply soft wrist restraints
D)Obtain CT scan of the head
E)Provide reassurance, reorientation, and observation
A)Administer dantrolene
B)Administer lorazepam
C)Apply soft wrist restraints
D)Obtain CT scan of the head
E)Provide reassurance, reorientation, and observation

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
33
A 58-year-old man comes to the office due to a hard mass on the posterior left elbow. The mass has been growing for the past 3 years. The patient has had no fever, pain, weight loss, or trauma. Medical history includes hypertension, chronic kidney disease, and gout. On examination, there is a 3 × 3 cm, nontender, hard mass just under the skin in the posterior left elbow. The elbow is not red, warm, or tender. Elbow imaging shows a 3-cm, soft tissue mass and bone erosions with overhanging edges of cortical bone at the olecranon process. Serum creatinine is 1.7 mg/dL. Which of the following conditions most likely explains this patient's findings?
A)Chronic kidney disease-mineral and bone disorder
B)Chronic olecranon bursitis
C)Osteoarthritis
D)Osteosarcoma
E)Tophaceous gout
A)Chronic kidney disease-mineral and bone disorder
B)Chronic olecranon bursitis
C)Osteoarthritis
D)Osteosarcoma
E)Tophaceous gout

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
34
A previously healthy 35-year-old man is evaluated in the hospital for new-onset fever. He was admitted 9 days ago following a motorcycle collision that resulted in severe traumatic brain injury and multiple extremity fractures. The patient initially required mechanical ventilation and multiple interventions to lower his intracranial pressure. He has since stabilized and underwent fracture fixation and tracheostomy, with subsequent weaning off of mechanical ventilation. Yesterday, while receiving a sponge bath, the patient was noted to be diaphoretic as well as hypertensive and tachycardic; his symptoms improved after morphine administration. Today, during routine repositioning and vital sign measurement, he again becomes diaphoretic. Temperature is 38.8 C (101.8 F), blood pressure is 194/110 mm Hg, pulse is 146/min, and respirations are 40/min. Oxygen saturation is 98% on room air. On examination, heart sounds and lung sounds are normal. Neurologic examination shows eye opening and withdrawal of all 4 extremities in response to painful stimuli, which is unchanged from previous examinations. Which of the following is the most likely cause of this patient's abnormal vital signs?
A)Alcohol withdrawal
B)Bacterial sepsis
C)Elevated intracranial pressure
D)Paroxysmal sympathetic hyperactivity
E)Pulmonary thromboembolism
F)Uncontrolled acute pain
A)Alcohol withdrawal
B)Bacterial sepsis
C)Elevated intracranial pressure
D)Paroxysmal sympathetic hyperactivity
E)Pulmonary thromboembolism
F)Uncontrolled acute pain

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
35
A 68-year-old man is evaluated in the cardiac care unit for confusion and agitation 3 days after coronary artery bypass grafting. Other than blood transfusion for perioperative bleeding, the surgery was uncomplicated. After initial difficulty weaning, the patient was successfully extubated on postoperative day 2. His pain has been well controlled with IV morphine, and he was calm throughout the day. This evening, the patient suddenly became anxious and started to pull his IV catheter. Medical history is significant for type 2 diabetes mellitus, dyslipidemia, and peripheral artery disease. He does not drink alcohol. Temperature is 37.1 C (98.8 F), blood pressure is 138/86 mm Hg, pulse is regular at 96/min, and respirations are 18/min. Pulse oximetry is 96% on room air. The patient is oriented to person but not place or time. During examination, he tries to grab the bed rails and sit up but calms down easily with reorientation. The patient states that he is frightened by small animals hopping around his bed. He has no apparent focal weakness. Laboratory studies are normal. What is the best initial intervention to help prevent self-harm in this patient?
A)Apply soft wrist restraints only at night
B)Discontinue all analgesics for pain
C)Employ a professional sitter at bedside
D)Restrict daytime interactions to maximize rest
E)Schedule nighttime lorazepam for sleep
A)Apply soft wrist restraints only at night
B)Discontinue all analgesics for pain
C)Employ a professional sitter at bedside
D)Restrict daytime interactions to maximize rest
E)Schedule nighttime lorazepam for sleep

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
36
A 75-year-old man comes to the office for evaluation of right hip pain. The patient first noticed the pain several months ago and it has become increasingly worse. He now has trouble putting on his shoes and socks. The patient used to walk his dog for 2 miles each night, but he now must use a cane and can only walk a half-mile. The patient has a history of hypertension. BMI is 32 kg/m2. X-ray of the right hip is shown below:  Which of the following is the most likely cause of this patient's hip pain?
Which of the following is the most likely cause of this patient's hip pain?
A)Avascular necrosis
B)Femur fracture
C)Greater trochanteric pain syndrome
D)Hip dislocation
E)Osteoarthritis
F)Osteosarcoma
 Which of the following is the most likely cause of this patient's hip pain?
Which of the following is the most likely cause of this patient's hip pain?A)Avascular necrosis
B)Femur fracture
C)Greater trochanteric pain syndrome
D)Hip dislocation
E)Osteoarthritis
F)Osteosarcoma

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
37
A 38-year-old construction worker is brought to the emergency department after falling from a 3.1 m (10 ft) height. Bystanders reported that the patient hit his head on the concrete and had jerking movements for 30 seconds. In the emergency department, blood pressure is 152/90 mm Hg, pulse is 92/min, and respirations are 16/min. On physical examination, the patient opens his eyes to verbal commands, makes incomprehensible sounds, and localizes pain. Glasgow coma scale score is 10. There is boggy swelling of the temporoparietal scalp. No major injuries of the chest, abdomen, or extremities are apparent. CT scan of the head shows linear fractures of the temporal and parietal bones, and multiple frontal, parietal, and temporal lobe contusions. There is no shift of midline structures. No cervical spine fracture or dislocation is present. Tranexamic acid is administered. Which of the following is the most likely mechanism of the beneficial effect of this drug?
A)Maintenance of normothermia
B)Reduction in brain edema
C)Reduction in cerebral metabolic demand
D)Prevention of intracranial hemorrhage
E)Prevention of seizures
A)Maintenance of normothermia
B)Reduction in brain edema
C)Reduction in cerebral metabolic demand
D)Prevention of intracranial hemorrhage
E)Prevention of seizures

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
38
A 40-year-old woman is brought to the emergency department following a low-speed motor vehicle accident. The patient was in the front passenger seat. During the accident, she hit her head against the windshield and hurt her right leg. She appears alert and oriented. Glasgow Coma Scale score is 15/15. Bilateral pupils are equal and reactive to light. There is a bruise over the right forehead, but no tenderness is present on palpation of the cranial bones. Examination of the right leg shows a hematoma over the thigh. Right knee extension and patellar reflex are markedly reduced compared to those on the left. There is decreased sensation to both sharp and dull stimuli over the anterior side of the right thigh and the medial side of the lower leg. All other dermatomes are intact. This patient most likely has an injury to which of the following nerves?
A)Common peroneal
B)Femoral
C)Ilioinguinal
D)Obturator
E)Tibial
A)Common peroneal
B)Femoral
C)Ilioinguinal
D)Obturator
E)Tibial

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
39
An 80-year-old Asian man comes to the office for evaluation of fatigue and 4.5 kg (10 lb) weight loss. Medical history is notable for benign prostatic hyperplasia (which is treated with tamsulosin), coronary artery disease, and hypertension. The patient does not use tobacco and drinks 2 shots of whiskey daily. He eats a vegetarian diet. Vital signs are normal. Physical examination shows a nodular prostate and inguinal lymphadenopathy. Serum prostate-specific antigen level is 25 ng/mL (normal: <4.5 ng/mL). Biopsy of the prostate reveals adenocarcinoma. Which of the following risk factors is most strongly associated with development of cancer in this patient?
A)Advanced age
B)Alcohol use
C)Benign prostatic hyperplasia
D)Ethnicity
E)Use of tamsulosin
F)Vegetarian diet
A)Advanced age
B)Alcohol use
C)Benign prostatic hyperplasia
D)Ethnicity
E)Use of tamsulosin
F)Vegetarian diet

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
40
A 34-year-old man is being discharged from the hospital after treatment for splenic rupture and intraabdominal bleeding following blunt abdominal trauma. His postoperative course was uncomplicated. The patient has no other chronic medical conditions and previously took no medications. He has no known drug allergies. Vital signs are normal. Abdominal examination shows a well healing incision. Appropriate vaccinations are planned for the first follow-up appointment in 2 weeks. Which of the following antibiotics should be prescribed for this patient to take immediately if he develops a fever?
A)Amoxicillin-clavulanate
B)Clindamycin
C)Metronidazole
D)Rifampin
E)Trimethoprim-sulfamethoxazole
A)Amoxicillin-clavulanate
B)Clindamycin
C)Metronidazole
D)Rifampin
E)Trimethoprim-sulfamethoxazole

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
41
A 22-year-old previously healthy man is brought to the emergency department by ambulance after a motor vehicle collision. The patient was unrestrained, and his vehicle sustained significant damage. The patient has anterior chest wall pain and painful respirations. Blood pressure is 110/70 mm Hg, pulse is 110/min, respirations are 18/min, and oxygen saturation is 98% on room air. He is alert and oriented to time, place, and person. Jugular venous pressure is normal. Anterior chest wall bruising is present. Bilateral breath sounds are normal and equal; heart sounds are normal. Examination of the abdomen and upper and lower extremities shows no abnormalities. Extended Focused Assessment with Sonography for Trauma (eFAST) reveals no pericardial or pleural effusion, or intrabdominal bleeding; chest x-ray and CT scan of the cervical spine are normal. The patient's pain improves with pain medication. Which of the following is the best next step in management of this patient?
A)Administer a beta blocker
B)Admit the patient and monitor serial cardiac enzymes
C)Discharge the patient home with analgesics
D)Obtain an electrocardiogram
E)Obtain a transesophageal echocardiogram
A)Administer a beta blocker
B)Admit the patient and monitor serial cardiac enzymes
C)Discharge the patient home with analgesics
D)Obtain an electrocardiogram
E)Obtain a transesophageal echocardiogram

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
42
A 42-year-old obese woman with a history of chronic alcoholism presents with right upper quadrant abdominal pain that began shortly after she had dinner at a local steakhouse. The pain is sharp, rated 7/10 in severity, and radiates to her right scapula. She also complains of nausea and vomiting. Her medical records indicate she has a history of asymptomatic gallstones. She drinks approximately 6 beers a day for the past 20 years but denies tobacco or illicit drug use. Her temperature is 38.5 C (101.3 F), blood pressure is 110/60 mm Hg, pulse is 96/min, and respirations are 16/min. On physical examination, there is right upper quadrant tenderness with deep inspiration. The rest of her examination is within normal limits. Laboratory studies are shown below.  Complete blood count shows leukocytosis with mild left shift. Which of the following is the most likely initial event leading to this patient's symptoms?
Complete blood count shows leukocytosis with mild left shift. Which of the following is the most likely initial event leading to this patient's symptoms?
A)Impaction of gallstone in cystic duct
B)Infection of gallbladder
C)Common bile duct obstruction with stone
D)Carcinoma of pancreatic head
E)Alcohol toxicity
 Complete blood count shows leukocytosis with mild left shift. Which of the following is the most likely initial event leading to this patient's symptoms?
Complete blood count shows leukocytosis with mild left shift. Which of the following is the most likely initial event leading to this patient's symptoms?A)Impaction of gallstone in cystic duct
B)Infection of gallbladder
C)Common bile duct obstruction with stone
D)Carcinoma of pancreatic head
E)Alcohol toxicity

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
43
A 63-year-old man comes to the emergency department due to left leg pain. The patient typically has pain in both legs after walking a couple of blocks, but several hours ago, severe left leg pain suddenly developed while he was resting. He reports numbness in the left leg, and he is also experiencing intermittent palpitations. Medical history includes hypertension and hyperlipidemia. The patient has smoked a pack of cigarettes daily for 45 years. Blood pressure is 130/80 mm Hg, and pulse is 116/min and irregular. On examination, hair is sparse on both legs. Distal pulses are absent on the left and diminished on the right. Sensation to light touch is decreased on the dorsum of the left foot and leg, and ankle dorsiflexion is weaker on the left. Which of the following is the best first step in management of this patient?
A)Ankle-brachial index
B)CT angiography of the lower extremities
C)Intravenous heparin infusion
D)Surgical bypass grafting
E)Transthoracic echocardiography
A)Ankle-brachial index
B)CT angiography of the lower extremities
C)Intravenous heparin infusion
D)Surgical bypass grafting
E)Transthoracic echocardiography

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
44
A 30-year-old man comes to the office for follow-up after traumatic injury to his left eye. Two months ago, there was an explosion at the factory where he worked. A large piece of shrapnel penetrated his left eye. Surgical removal of the shrapnel was performed, and vision in the left eye recovered to 20/200. Today, the patient reports that vision in his right eye is becoming blurry. On examination, there is bilateral conjunctival erythema. The right eye visual acuity is 20/160, which was normal 2 months ago. Which of the following is most likely involved in the pathogenesis of this patient's current ocular condition?
A)Hematogenous fungal spread
B)IgE-mediated hypersensitivity
C)Narrow anterior chamber angle
D)Precipitating immune complexes
E)T-cell sensitization to self-antigens
A)Hematogenous fungal spread
B)IgE-mediated hypersensitivity
C)Narrow anterior chamber angle
D)Precipitating immune complexes
E)T-cell sensitization to self-antigens

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
45
A 11-year-old girl is brought to the emergency department due to persistent vomiting. The first episode of emesis occurred 12 hours ago, and for the past 4 hours, the patient has been unable to keep any liquids down. She also has nausea and epigastric discomfort but no fever, abdominal distension, or diarrhea. The patient is a competitive gymnast. Yesterday, she fell and struck her abdomen hard on the balance beam during practice. Temperature is 36.7 C (98.1 F), blood pressure is 106/72 mm Hg, pulse is 110/min, and respirations are 18/min. On examination, mucous membranes are dry. Lung and heart sounds are normal. The abdomen is scaphoid with linear bruising across the epigastrium. On palpation, there is epigastric tenderness without guarding, rigidity, or rebound tenderness. Upright chest and abdominal x-rays are normal, with no free air under the diaphragm. Focused assessment with sonography for trauma reveals no intraperitoneal free fluid or air. Which of the following is the best next step in management of this patient?
A)Antiemetics and observation only
B)CT scan of the abdomen
C)Diagnostic peritoneal lavage
D)Exploratory laparotomy
E)Gallbladder ultrasonography
A)Antiemetics and observation only
B)CT scan of the abdomen
C)Diagnostic peritoneal lavage
D)Exploratory laparotomy
E)Gallbladder ultrasonography

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
46
A 43-year-old woman comes to the emergency department due to nausea, dizziness, and headache for a day. Her menses began 2 days ago. She has occasionally had fatigue and dizziness during her menstrual periods, but today's symptoms feel different. The patient has a history of von Willebrand disease, causing recurrent, heavy menstrual blood loss, and is scheduled for an endometrial ablation procedure. Her only medication is intranasal desmopressin taken on the first 3 days of her menstrual period. Temperature is 36.9 C (98.4 F), blood pressure is 120/80 mm Hg, pulse is 92/min and regular, and respirations are 18/min. The patient appears restless. Mucous membranes are moist. Deep tendon reflexes are 2+ throughout and Babinski sign is absent. Sensory examination shows no focal deficits. The chest is clear to auscultation. The abdomen is soft and nontender. There is no peripheral edema. The remainder of the examination is unremarkable. Which of the following is the most appropriate next step in management?
A)Arterial blood gas
B)Liver function studies
C)MRI of the brain
D)Plasma desmopressin level
E)Serum electrolytes
A)Arterial blood gas
B)Liver function studies
C)MRI of the brain
D)Plasma desmopressin level
E)Serum electrolytes

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
47
A 25-year-old man comes to the emergency department due to pain and swelling in his right ear. The patient sustained several blows to his ear during a wrestling match a few hours ago. He had no loss of consciousness and has no headache, neck pain, or hearing loss. Blood pressure is 110/55 mm Hg, pulse is 84/min, and respirations are 14/min. On examination, the right ear is red and swollen, and there is an auricular hematoma. The tympanic membrane is normal without hemotympanum. The auditory canal is within normal limits. There is no mastoid erythema or tenderness to palpation. There is no facial swelling or tenderness, and the neurologic examination is intact. Which of the following is the best next step in management of this patient?
A)Discharge with oral antibiotic
B)Evacuation of hematoma in the emergency department
C)No treatment is needed because this will resolve spontaneously
D)Pressure dressing and discharge with close follow-up
A)Discharge with oral antibiotic
B)Evacuation of hematoma in the emergency department
C)No treatment is needed because this will resolve spontaneously
D)Pressure dressing and discharge with close follow-up

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
48
A 40-year-old man comes to the office for evaluation of recurrent epistaxis. Every morning, the patient wakes up with significant nasal congestion; when he blows his nose, he often sees crusting and blood clots in the tissue. Afterward, his nose frequently (several times a week) starts bleeding. It stops with <5 minutes of pinching his nasal alae. Medical history includes obesity, hypertension, and obstructive sleep apnea treated with continuous positive airway pressure (CPAP). Vital signs are within normal limits. On examination, the nose has bilateral crusting with excoriations on both sides of the nasal septum, but there is no bleeding. Which of the following is the most appropriate step in management of this patient's condition?
A)Biopsy of the nasal septum
B)Complete blood count and coagulation panel
C)CPAP humidification
D)Nasal corticosteroid sprays
E)Oxymetazoline daily in the morning
A)Biopsy of the nasal septum
B)Complete blood count and coagulation panel
C)CPAP humidification
D)Nasal corticosteroid sprays
E)Oxymetazoline daily in the morning

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
49
A 64-year-old woman is brought to the emergency department due to fever, chills, flank pain, and lethargy for the past 2 days. Temperature is 38.9 C (102 F), blood pressure is 100/60 mm Hg, and pulse is 120/min. The patient has right costovertebral angle tenderness. Leukocytes are 16,000/mm3 and urinalysis shows pyuria, many bacteria, and positive nitrites. ECG shows sinus tachycardia. A central venous catheter placement is planned for intravenous therapy and hemodynamic monitoring. After the patient's chest is appropriately prepared and draped, a needle is inserted just lateral to the angle of the left clavicle and a triple lumen catheter is placed into the left subclavian vein. Each lumen is flushed with sterile saline after obtaining blood return. The catheter is sutured in place to the skin and a sterile dressing is applied. Which of the following is the best next step in management of this patient?
A)Antibiotic through the catheter
B)Bedside echocardiography
C)Fluid bolus through the catheter
D)Portable chest radiograph
E)Repeat ECG
A)Antibiotic through the catheter
B)Bedside echocardiography
C)Fluid bolus through the catheter
D)Portable chest radiograph
E)Repeat ECG

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
50
An 18-year-old football player is brought to the emergency department due to persistent pain following a hard tackle. The patient had just caught a pass when he was tackled from the front, with the opponent landing all his weight on the patient's abdomen. Immediately afterward, he began to experience abdominal discomfort and nausea. Blood pressure is 92/64 mm Hg, pulse is 118/min, and respirations are 24/min. The patient is alert but appears anxious. Bilateral breath sounds are clear and equal. Heart sounds are normal without murmur. The abdomen is mildly distended and tender to palpation diffusely. Chest x-ray and pelvic x-ray are normal. Focused Assessment with Sonography for Trauma reveals intraperitoneal free fluid. Further evaluation of this patient is most likely to reveal which of the following?
A)Abdominal aortic tear
B)Bladder rupture
C)Diaphragmatic tear
D)Duodenal hematoma
E)Pancreatic transection
F)Splenic laceration
A)Abdominal aortic tear
B)Bladder rupture
C)Diaphragmatic tear
D)Duodenal hematoma
E)Pancreatic transection
F)Splenic laceration

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
51
A 67-year-old man comes to the emergency department due to worsening left foot pain. The pain involves the entire left foot and is severe in the forefoot. The pain began a day prior while the patient was lying in bed watching television. He immediately sat up and dangled his foot over the side of the bed, but this did not improve the pain as it had during past episodes. Although the pain was initially mild, it progressively worsened over the course of the day. The patient tried heat packs and over-the-counter pain medication, which he takes intermittently for chronic low back pain, without relief. Medical history includes hypertension and hyperlipidemia. The patient smokes 1-2 packs of cigarettes daily. Temperature is 36.7 C (98 F), blood pressure is 146/90 mm Hg, and pulse is 92/min. On examination, the skin of both lower legs is shiny and hairless, and the left foot is mottled and cooler to the touch than the right foot. Pulses are not palpable in either foot but can be detected with doppler in the right foot. The left foot has capillary refill of 4-5 seconds. The patient has difficulty moving his left foot and toes. Which of the following is the most likely cause of the patient's new symptoms?
A)Atherosclerotic plaque disruption
B)Exaggerated cutaneous vasoreactivity
C)Increased compartmental pressure
D)Popliteal vein thrombosis
E)Tobacco-associated vasculitis
A)Atherosclerotic plaque disruption
B)Exaggerated cutaneous vasoreactivity
C)Increased compartmental pressure
D)Popliteal vein thrombosis
E)Tobacco-associated vasculitis

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
52
A 23-year-old man is brought to the emergency department after a motor vehicle collision. The patient was found unresponsive at the scene and intubated by the paramedics, who also administered 2 L of normal saline. He was the unrestrained driver. Upon arrival, blood pressure is 72/54 mm Hg, and pulse is 120/min. The patient responds to strong vocal and tactile stimuli by opening his eyes. Pupils are equal and reactive to light. Neck veins are distended. There are multiple bruises involving the anterior chest and upper abdomen. Chest x-ray reveals a small, left-sided pleural effusion and normal cardiac contours. Which of the following is the most likely diagnosis?
A)Aortic rupture
B)Bronchial rupture
C)Cardiac tamponade
D)Esophageal rupture
E)Lung contusion
A)Aortic rupture
B)Bronchial rupture
C)Cardiac tamponade
D)Esophageal rupture
E)Lung contusion

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
53
An 82-year-old man is brought to the emergency department due to fever and confusion. Yesterday, he experienced abdominal pain, nausea, vomiting, and rigors in the nursing home where he lives. Earlier today, he was found to be lethargic. Medical history includes hypercholesterolemia, type 2 diabetes mellitus, and Alzheimer dementia. The patient quit smoking 30 years ago and does not drink alcohol. Temperature is 39.1 C (102.4 F), blood pressure is 105/55 mm Hg, pulse is 110/min, and respirations are 20/min. He is lethargic but arousable to strong stimuli. On examination, the mucous membranes are dry. Scleral icterus is present. No cardiac murmurs are heard. The lungs are clear to auscultation. There is marked tenderness in the right upper quadrant and epigastrium but no distension, rebound, or guarding. Laboratory results are as follows: 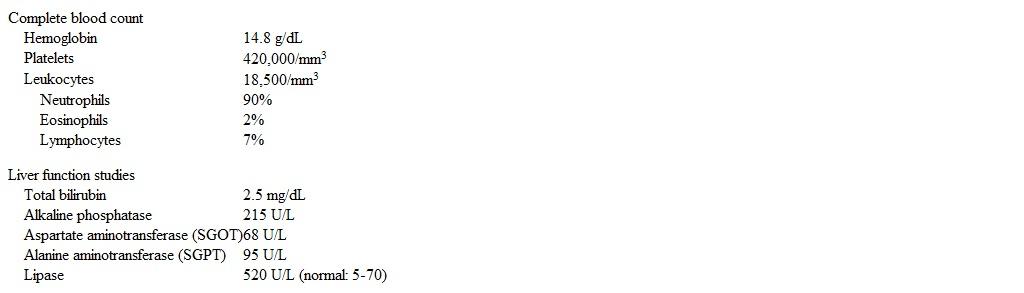 An abdominal ultrasound reveals multiple gallstones and a dilated common bile duct. The gallbladder wall is not thickened. In addition to aggressive intravenous hydration and antibiotics, which of the following is the best next step in management of this patient?
An abdominal ultrasound reveals multiple gallstones and a dilated common bile duct. The gallbladder wall is not thickened. In addition to aggressive intravenous hydration and antibiotics, which of the following is the best next step in management of this patient?
A)CT scan of the abdomen
B)Emergent cholecystectomy
C)Endoscopic retrograde cholangiopancreatography
D)HIDA scan
E)No additional intervention
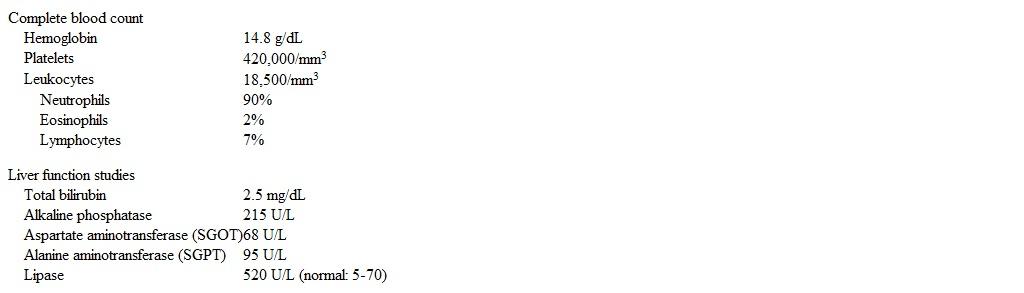 An abdominal ultrasound reveals multiple gallstones and a dilated common bile duct. The gallbladder wall is not thickened. In addition to aggressive intravenous hydration and antibiotics, which of the following is the best next step in management of this patient?
An abdominal ultrasound reveals multiple gallstones and a dilated common bile duct. The gallbladder wall is not thickened. In addition to aggressive intravenous hydration and antibiotics, which of the following is the best next step in management of this patient?A)CT scan of the abdomen
B)Emergent cholecystectomy
C)Endoscopic retrograde cholangiopancreatography
D)HIDA scan
E)No additional intervention

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
54
A 43-year-old construction worker is brought to the emergency department after falling 6.1 m (20 ft) from faulty scaffolding. The patient has severe chest pain and appears scared. Blood pressure is 136/92 mm Hg, and pulse is 120/min. Chest x-ray is shown below. 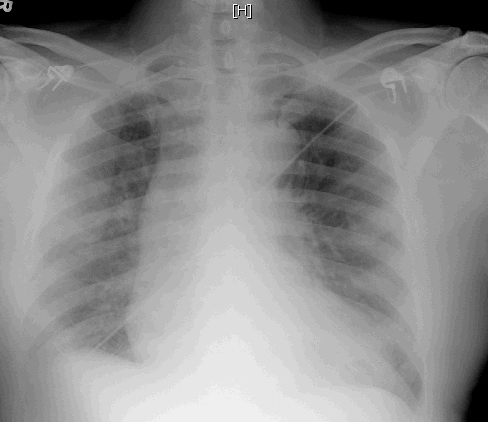 Which of the following is the most likely diagnosis in this patient?
Which of the following is the most likely diagnosis in this patient?
A)Blunt aortic injury
B)Diaphragmatic rupture
C)Left ventricular aneurysm
D)Myocardial contusion
E)Pulmonary contusion
F)Tracheobronchial disruption
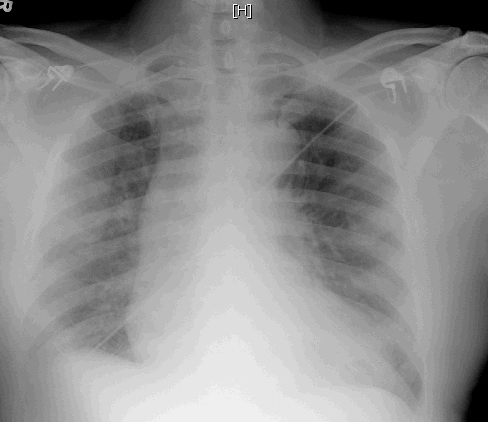 Which of the following is the most likely diagnosis in this patient?
Which of the following is the most likely diagnosis in this patient?A)Blunt aortic injury
B)Diaphragmatic rupture
C)Left ventricular aneurysm
D)Myocardial contusion
E)Pulmonary contusion
F)Tracheobronchial disruption

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
55
A previously healthy 19-year-old man comes to the emergency department (ED) due to persistent abdominal discomfort. The patient previously came to the ED 3 days ago after he fell while mountain biking. He did not lose consciousness and recalls hitting the handlebars prior to flipping and landing on his back. His trauma workup-which included CT scan of the chest, abdomen, and pelvis-was negative, and he was discharged. Since then, the patient has had persistent upper abdominal discomfort and nausea, along with an episode of nonbilious emesis. Temperature is 38.1 C (100.6 F), blood pressure is 104/62 mm Hg, and pulse is 108/min. The lungs are clear to auscultation, and heart sounds are normal. Ecchymosis is present across the upper abdomen, which is tender to palpation with voluntary guarding. Bowel sounds are decreased. Bedside ultrasonography reveals a large amount of free fluid in the upper abdomen. Which of the following is the most likely cause of this patient's condition?
A)Abdominal aortic tear
B)Diaphragmatic rupture
C)Hepatic laceration
D)Splenic rupture
E)Pancreatic duct injury
A)Abdominal aortic tear
B)Diaphragmatic rupture
C)Hepatic laceration
D)Splenic rupture
E)Pancreatic duct injury

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
56
A 29-year-old man comes to the emergency department with persistent vomiting and abdominal pain for the last 24 hours. The pain is crampy, diffuse, and getting worse. He had a normal bowel movement 3 days ago and has no diarrhea. The emesis appears green without blood or coffee grounds. The patient has not eaten since the onset of the pain due to nausea. His temperature is 36.8 C (98.2 F), pulse is 91/min, and blood pressure is 116/75 mm Hg while sitting and 94/65 mm Hg while standing. His abdomen is distended with hyperactive bowel sounds. Percussion reveals tympany, and the patient is diffusely tender to palpation. There is no rebound tenderness or guarding. Laboratory results are as follows: 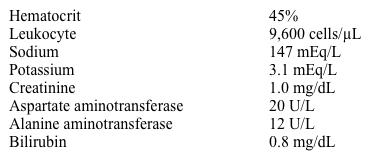 Which of the following historical findings would most likely be seen in this patient?
Which of the following historical findings would most likely be seen in this patient?
A)Appendectomy 6 months ago
B)Fatty food intolerance
C)High alcohol consumption
D)Occasional black or tarry stool
E)Recent fever and nonbloody diarrhea
F)Recent weight loss
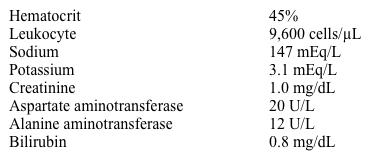 Which of the following historical findings would most likely be seen in this patient?
Which of the following historical findings would most likely be seen in this patient?A)Appendectomy 6 months ago
B)Fatty food intolerance
C)High alcohol consumption
D)Occasional black or tarry stool
E)Recent fever and nonbloody diarrhea
F)Recent weight loss

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
57
A 37-year-old woman is brought to the hospital with abdominal pain and confusion that began 24 hours ago. The patient describes the pain as stabbing and unremitting. It is worse in the upper abdomen and associated with nausea and frequent nonbloody emesis. Medical history is significant for type 1 diabetes mellitus and major depression. The patient has been hospitalized for diabetic ketoacidosis in the setting of insulin noncompliance as well as for a suicide attempt as a teenager. Temperature is 38.9 C (102 F), blood pressure is 90/60 mm Hg, pulse is 110/min, and respirations are 24/min. The patient is oriented to person but not to place or time. The mucous membranes are dry, and capillary refill is delayed. Heart and lung sounds are unremarkable. The abdomen is markedly tender in the right upper quadrant and epigastrium but with no rebound or guarding. Laboratory results are as follows: 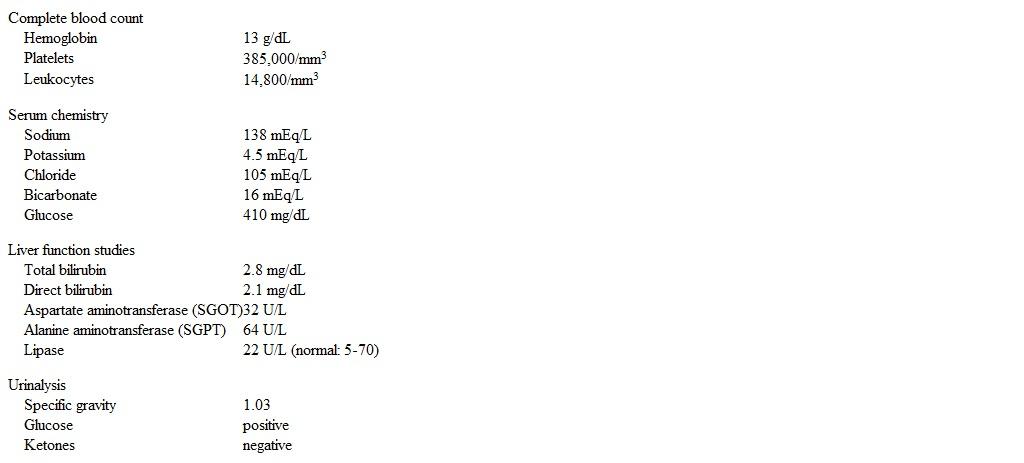 Which of the following is the most likely diagnosis?
Which of the following is the most likely diagnosis?
A)Acetaminophen overdose
B)Acute cholangitis
C)Acute viral hepatitis
D)Diabetic ketoacidosis
E)Ethanol overdose
F)Mesenteric arterial occlusion
G)Necrotizing pancreatitis
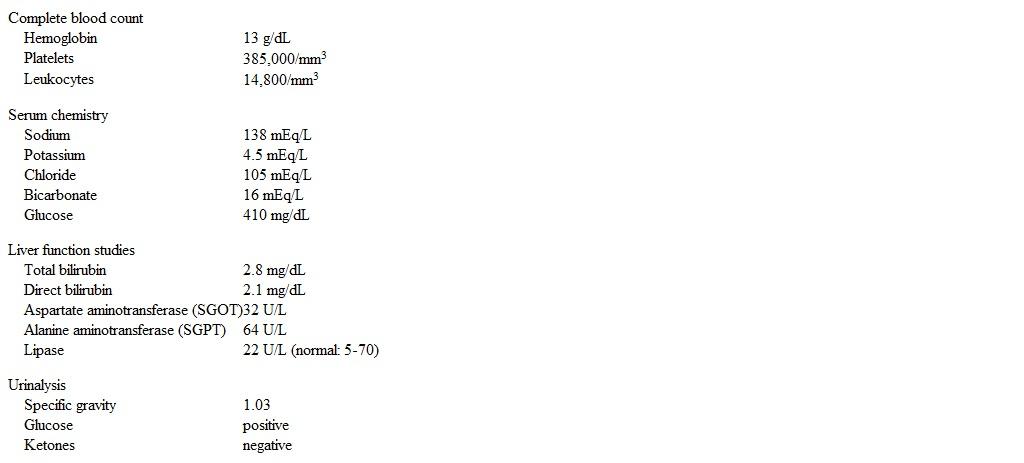 Which of the following is the most likely diagnosis?
Which of the following is the most likely diagnosis?A)Acetaminophen overdose
B)Acute cholangitis
C)Acute viral hepatitis
D)Diabetic ketoacidosis
E)Ethanol overdose
F)Mesenteric arterial occlusion
G)Necrotizing pancreatitis

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
58
A 21-year-old woman comes to the emergency department after she slipped and fell at work, landing on her mouth 30 minutes ago. She brought a tooth with her that got avulsed secondary to the injury. The patient did not lose consciousness and has no other injuries. Vital signs are within normal limits. On examination, the patient has an avulsed left central incisor with a small amount of dry blood in the socket. The remainder of the teeth are stable without fractures. There is no injury to the gum or palate. There is no mandibular or maxillary tenderness or instability, and neurologic examination is normal. The patient has the avulsed tooth with her in a tissue, and it appears intact. Which of the following is the best next step in management of this patient?
A)Dispose of the tooth; discharge with antibiotics and dental referral
B)Place the tooth in an ice-filled bag and advise follow-up with the dentist in 24-48 hours
C)Rinse the tooth and socket gently with hydrogen peroxide; reimplant and splint the tooth
D)Rinse the tooth and socket gently with normal saline; reimplant and splint the tooth
A)Dispose of the tooth; discharge with antibiotics and dental referral
B)Place the tooth in an ice-filled bag and advise follow-up with the dentist in 24-48 hours
C)Rinse the tooth and socket gently with hydrogen peroxide; reimplant and splint the tooth
D)Rinse the tooth and socket gently with normal saline; reimplant and splint the tooth

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
59
A 72-year-old man is brought to the emergency department by his daughter after she found him confused and febrile at home. Since the patient's wife died 6 months ago, he has insisted on continuing to live independently; however, he has taken worse care of his health, including refusing doctor's visits. Medical history includes type 2 diabetes, chronic kidney disease, and peripheral artery disease. Temperature is 38.3 C (101 F). Blood pressure is 98/54 mm Hg and pulse is 104/min. The patient is lethargic but opens his eyes when his name is called. He is not oriented to place, time, or situation. Both lower extremities are without palpable dorsalis pedis, posterior tibial, or popliteal pulses. The left foot is shown in the image below. In addition to obtaining blood cultures and administering antibiotics, which of the following is the best next step in management of this patient? 
A)Amputation of the foot
B)Hyperbaric oxygen therapy
C)Revascularization procedure
D)Sharp local wound debridement
E)Whirlpool therapy

A)Amputation of the foot
B)Hyperbaric oxygen therapy
C)Revascularization procedure
D)Sharp local wound debridement
E)Whirlpool therapy

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
60
A 34-year-old man is brought to the emergency department after being shot in the right thigh during an attempted robbery. The patient is awake, alert, and in moderate distress. Blood pressure is 101/49 mm Hg and pulse is 122/min. Records indicate that his last tetanus vaccine was a year ago. Physical examination shows a gunshot entry wound on the anteromedial upper right thigh with an exit wound on the lateral thigh. There is a hematoma at the entry site but no active bleeding from either wound. The right lower extremity is cool to the touch and distal pulses are feeble. Radiography of the lower extremity shows no fracture. Which of the following is the most appropriate next step in management of this patient?
A)Blood transfusion and close observation
B)Compression dressing and prophylactic antibiotics
C)CT angiography of the right lower extremity
D)Doppler ultrasonography of the lower limb vessels
E)Urgent surgical exploration of the wound
A)Blood transfusion and close observation
B)Compression dressing and prophylactic antibiotics
C)CT angiography of the right lower extremity
D)Doppler ultrasonography of the lower limb vessels
E)Urgent surgical exploration of the wound

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
61
A 59-year-old woman arrives at the emergency department due to right upper quadrant abdominal pain, nausea, vomiting, and fever since yesterday. She has no hematemesis, constipation, diarrhea, or shortness of breath. The patient's medical history is significant for hypertension, stable coronary artery disease, and type 2 diabetes mellitus. She does not use tobacco, alcohol, or illicit drugs. Temperature is 38.9 C (102 F), blood pressure is 112/76 mm Hg, pulse is 101/min, and respirations are 18/min. Oxygen saturation is 96% on room air. BMI is 34 kg/m2. Cardiopulmonary examination shows no abnormalities. There is marked tenderness and voluntary guarding to palpation in the right upper quadrant of the abdomen. Laboratory results are as follows. 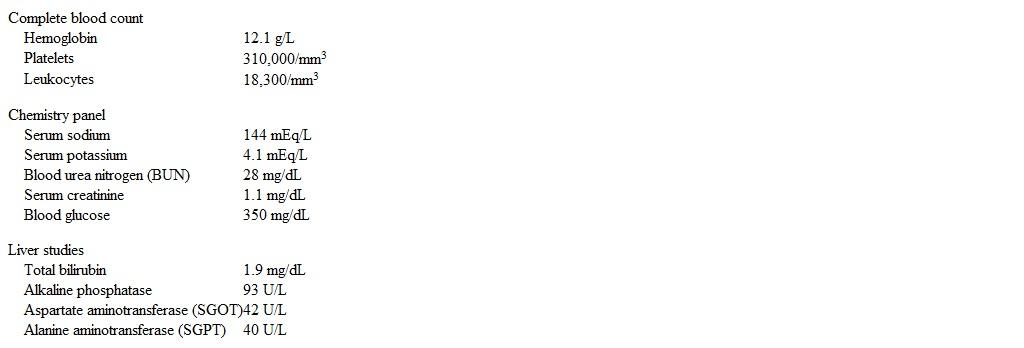 Abdominal imaging demonstrates a distended gallbladder with gas in the gallbladder wall and lumen. There is no gas in the biliary tree. What is the most likely diagnosis in this patient?
Abdominal imaging demonstrates a distended gallbladder with gas in the gallbladder wall and lumen. There is no gas in the biliary tree. What is the most likely diagnosis in this patient?
A)Acute cholangitis
B)Biliary-enteric fistula
C)Emphysematous cholecystitis
D)Gallstone ileus
E)Peptic ulcer perforation
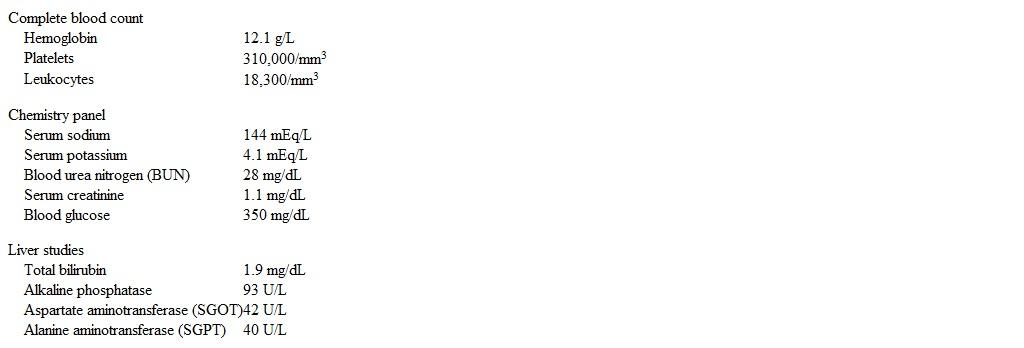 Abdominal imaging demonstrates a distended gallbladder with gas in the gallbladder wall and lumen. There is no gas in the biliary tree. What is the most likely diagnosis in this patient?
Abdominal imaging demonstrates a distended gallbladder with gas in the gallbladder wall and lumen. There is no gas in the biliary tree. What is the most likely diagnosis in this patient?A)Acute cholangitis
B)Biliary-enteric fistula
C)Emphysematous cholecystitis
D)Gallstone ileus
E)Peptic ulcer perforation

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
62
A 70-year-old male presents to the emergency room complaining of weakness, dizziness and back pain. He denies nausea, vomiting, diarrhea, chest pain, palpitations, shortness of breath, urinary symptoms, or black stools. His past medical history is significant for diabetes mellitus, diabetic nephropathy and retinopathy, hypertension, atrial fibrillation and chronic leg cellulitis. He takes warfarin for chronic anticoagulation. On physical examination, his blood pressure is 120/70 mmHg and his heart rate is 110 and irregular. His WBC count is 10,500/mm3, hemoglobin level is 7.0 g/dL and platelet count is 170,000/mm3. An abdominal CT image is shown on the slide below.  Which of the following is the most likely diagnosis?
Which of the following is the most likely diagnosis?
A)Renal cell carcinoma
B)Vertebral fracture
C)Retroperitoneal hematoma
D)Hydronephrosis
E)Mesenteric ischemia
 Which of the following is the most likely diagnosis?
Which of the following is the most likely diagnosis?A)Renal cell carcinoma
B)Vertebral fracture
C)Retroperitoneal hematoma
D)Hydronephrosis
E)Mesenteric ischemia

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
63
A 38-year-old woman comes to the emergency department complaining of severe pain and swelling in her left leg. She fell 2 days ago while playing recreation-league soccer and suffered a mildly painful abrasion to her posterior left thigh. The pain has worsened steadily since and is now unbearable. Initially only her left proximal thigh was painful and red, but now the pain has spread to her buttock and proximal calf. The patient also complains of fatigue and chills. Her temperature is 39.4 C (102.7 F), blood pressure is 82/60 mm Hg, pulse is 104/min, and respirations are 18/min. Physical examination shows a swollen left thigh with moderate erythema over the left proximal thigh and buttock. The buttock and distal thigh are markedly tender to palpation, and the patient has no sensation to light touch over the proximal thigh. Blood pressure improves with intravenous fluids. CT scan of the affected area is shown in the exhibit. 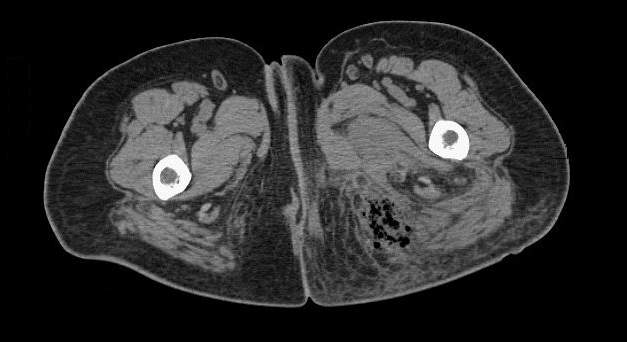 Which of the following is the most likely diagnosis in this patient?
Which of the following is the most likely diagnosis in this patient?
A)Abscess
B)Cellulitis
C)Hematoma
D)Necrotizing fasciitis
E)Pyomyositis
F)Thrombophlebitis
G)Toxic shock syndrome
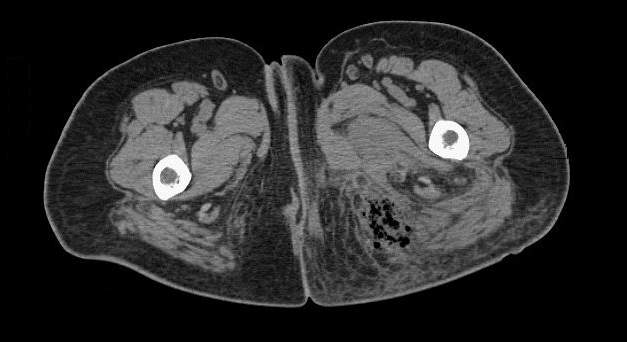 Which of the following is the most likely diagnosis in this patient?
Which of the following is the most likely diagnosis in this patient?A)Abscess
B)Cellulitis
C)Hematoma
D)Necrotizing fasciitis
E)Pyomyositis
F)Thrombophlebitis
G)Toxic shock syndrome

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
64
A 20-year-old man is brought to the emergency department after falling off a trampoline. He had been drinking alcohol with some friends and began jumping on a trampoline in his neighbor's backyard. The patient tried to do a backflip and landed on his head. Paramedics were called and found him confused but able to follow commands. However, he was unable to move his legs or his hands. The patient was placed in spine immobilization and transported to the emergency department. On arrival, his vital signs are within normal limits, but he has increasing shortness of breath and requests to sit up to help his breathing. Chest x-ray is normal, and ECG reveals sinus tachycardia. Over the next 30 minutes, his respirations become faster and shallower with more use of accessory muscles. The patient becomes sleepier and has difficulty responding to commands. Which of the following is the most appropriate next step in management?
A)Nasotracheal intubation
B)Needle cricothyroidotomy
C)Noninvasive positive pressure ventilation
D)Orotracheal intubation
E)Surgical tracheostomy
A)Nasotracheal intubation
B)Needle cricothyroidotomy
C)Noninvasive positive pressure ventilation
D)Orotracheal intubation
E)Surgical tracheostomy

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
65
A 75-year-old man is brought to the emergency department due to worsening generalized abdominal pain and nausea for the past 2 days. He has multiple chronic medical conditions and resides at a nursing facility. Temperature is 37.2 C (99 F), blood pressure is 128/74 mm Hg, and pulse is 94/min. Abdominal examination shows distension and diffuse tenderness without rigidity or rebound tenderness. Abdominal x-ray is shown in the image below:  Which of the following factors in this patient's history most likely increased the risk for developing this condition?
Which of the following factors in this patient's history most likely increased the risk for developing this condition?
A)Chronic constipation
B)Colonic hypermotility
C)Electrolyte abnormalities
D)Nonsteroidal anti-inflammatory drug use
E)Recent antibiotic therapy
 Which of the following factors in this patient's history most likely increased the risk for developing this condition?
Which of the following factors in this patient's history most likely increased the risk for developing this condition?A)Chronic constipation
B)Colonic hypermotility
C)Electrolyte abnormalities
D)Nonsteroidal anti-inflammatory drug use
E)Recent antibiotic therapy

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
66
A 32-year-old woman is brought to the emergency department an hour after developing acute-onset, right upper quadrant abdominal pain followed by syncope. The patient works at her family farm and felt well prior to the onset of these symptoms. She has no chronic medical conditions. She is sexually active and uses combined estrogen-progestin oral contraceptives. She does not use tobacco, alcohol, or illicit drugs. Temperature is 38.1 C (100.6 F), blood pressure is 80/50 mm Hg, pulse is 120/min, and respirations are 20/min. Oxygen saturation is 95% on room air. The patient appears anxious and pale. Examination shows abdominal distention, diffuse abdominal tenderness, and tender hepatomegaly. Bowel sounds are decreased. Extremities are cold, and capillary refill is delayed. Laboratory results are as follows:  Abdominal ultrasound of the right upper quadrant shows a solid liver mass and free fluid in the abdomen. Which of the following is the most likely diagnosis?
Abdominal ultrasound of the right upper quadrant shows a solid liver mass and free fluid in the abdomen. Which of the following is the most likely diagnosis?
A)Focal nodular hyperplasia
B)Hepatic abscess
C)Hepatic adenoma
D)Hepatic hemangioma
E)Hepatocellular carcinoma
F)Hydatid cyst
 Abdominal ultrasound of the right upper quadrant shows a solid liver mass and free fluid in the abdomen. Which of the following is the most likely diagnosis?
Abdominal ultrasound of the right upper quadrant shows a solid liver mass and free fluid in the abdomen. Which of the following is the most likely diagnosis?A)Focal nodular hyperplasia
B)Hepatic abscess
C)Hepatic adenoma
D)Hepatic hemangioma
E)Hepatocellular carcinoma
F)Hydatid cyst

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
67
A 36-year-old woman comes to the urgent care clinic due to worsening right lower extremity pain and swelling for the past several days. The patient has a history of injection drug use. She also exchanges sex for drugs and is inconsistent with condom use. Temperature is 37.1 C (98.8 F), blood pressure is 126/76 mm Hg, pulse is 86/min, and respirations are 13/min. Oxygen saturation is 98% on room air. On physical examination, edema, erythema, and warmth of the right leg are noted with increased calf and thigh diameters. There are injection marks in the right groin. Which of the following is the most likely diagnosis?
A)Acute lymphangitis
B)Deep venous thrombosis
C)Lymphatic filariasis
D)Lymphogranuloma venereum
E)Necrotizing myositis
A)Acute lymphangitis
B)Deep venous thrombosis
C)Lymphatic filariasis
D)Lymphogranuloma venereum
E)Necrotizing myositis

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
68
A 22-year-old man is brought to the emergency department by ambulance after sustaining a gunshot wound to the abdomen during a home invasion. The event occurred 45 minutes prior to arrival. Because of hypotension, paramedics administered 1 L of normal saline en route to the emergency department. On arrival, blood pressure is 98/62 mm Hg, pulse is 120/min, and respirations are 22/min. The patient is awake and moaning in pain. The lungs are clear to auscultation bilaterally, and heart sounds are normal. One bullet wound is noted in the left upper quadrant. The abdomen is tender and distended. The patient is moving all his extremities, but they are cool and clammy. Focused Assessment with Sonography for Trauma examination shows free fluid in the abdomen. Continuation of additional normal saline fluid boluses in this patient would likely result in which of the following?
A)Decreased risk for acute respiratory distress syndrome
B)Decreased risk for hypothermia
C)Increased risk for coagulopathy
D)Increased risk for metabolic alkalosis
A)Decreased risk for acute respiratory distress syndrome
B)Decreased risk for hypothermia
C)Increased risk for coagulopathy
D)Increased risk for metabolic alkalosis

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
69
A 26-year-old, previously healthy man is brought to the emergency department after a high-speed motor vehicle collision. He became obtunded in the field and required intubation by the paramedics. The patient also received 2 L of crystalloid on the way to the hospital. On arrival, blood pressure is 88/52 mm Hg and pulse is 128/min. Physical examination shows multiple contusions, including to the left side of the forehead, left arm, chest, abdomen, and pelvis, but there is no external hemorrhage. The trachea is midline. Breath sounds are present bilaterally and heart sounds are normal. The abdomen is nondistended and soft to palpation. Muscle tone is normal. Focused Assessment with Sonography for Trauma shows no pericardial or intraperitoneal free fluid. Which of the following is the most likely cause of this patient's hemodynamic instability?
A)Adrenal insufficiency
B)Intracranial hemorrhage
C)Pancreatic injury
D)Pelvic fracture
E)Spinal fracture
A)Adrenal insufficiency
B)Intracranial hemorrhage
C)Pancreatic injury
D)Pelvic fracture
E)Spinal fracture

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
70
A 16-year-old boy is brought to the emergency department by his mother due to a possible hand injury. She noticed that the patient's right hand was swollen and that he was not using it despite being right-handed. He has a history of oppositional defiant disorder and refuses to say how his hand was injured. Temperature is 38 C (100.4 F), blood pressure is 110/72 mm Hg, and pulse is 80/min. The dorsum of the right hand is swollen. There is erythema centered over the long finger metacarpophalangeal (MCP) joint, where there is a small, linear scab; the area is fluctuant on palpation, and passive movement of the joint elicits severe pain. Right hand x-ray reveals soft tissue swelling, no retained foreign body, and no underlying fractures or dislocations. Which of the following is the best next step in management of this patient?
A)Intraarticular glucocorticoid injection
B)Oral antibiotic therapy and outpatient follow-up
C)Oral nonsteroidal anti-inflammatory drugs and outpatient follow-up
D)Surgical irrigation and debridement of the MCP joint
A)Intraarticular glucocorticoid injection
B)Oral antibiotic therapy and outpatient follow-up
C)Oral nonsteroidal anti-inflammatory drugs and outpatient follow-up
D)Surgical irrigation and debridement of the MCP joint

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
71
A 34-year-old man is brought to the emergency department following a high-speed motor vehicle collision. He was found lying outside the car and was intubated by the paramedics. Upon arrival, the patient has absent breath sounds in the right chest, normal breath sounds in the left chest, and hypotension. A right-sided chest tube is placed, resulting in a loud rush of air. Physical examination reveals multiple bruises over the anterior chest wall, with crepitus on palpation. The patient is initially stabilized. Over the next hour, the patient's oxygen saturation progressively declines. Repeat chest x-ray reveals appropriate endotracheal and chest tube placement, reaccumulation of air in the right pleural space, pneumomediastinum, and increased subcutaneous emphysema. Which of the following is the most likely diagnosis?
A)Acute respiratory distress syndrome
B)Aspiration pneumonitis
C)Bronchial rupture
D)Diaphragmatic rupture
E)Esophageal rupture
F)Fat embolism
G)Hemothorax
A)Acute respiratory distress syndrome
B)Aspiration pneumonitis
C)Bronchial rupture
D)Diaphragmatic rupture
E)Esophageal rupture
F)Fat embolism
G)Hemothorax

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
72
A 26-year-old man is brought to the hospital after a motor vehicle collision. The patient was found unconscious at the scene and was intubated on the way to the hospital. Initial imaging showed left-sided epidural hematoma, multiple rib fractures, and a pelvic fracture. He was immediately taken to the operating room for epidural hematoma evacuation. During resuscitation and in the postoperative period, the patient received 4 L of intravenous fluids and 3 units of packed red blood cells. Although he was hemodynamically stable on day 1 of hospitalization, the nursing report on day 2 notes reduced urine output. In addition, there is persistent oozing from the patient's venipuncture sites and around the surgical wound. Which of the following is the most likely cause of this patient's bleeding?
A)ABO incompatibility
B)Acute liver failure
C)Complement-mediated microangiopathy
D)Consumptive coagulopathy
E)Drug-induced thrombocytopenia
F)Vitamin K deficiency
A)ABO incompatibility
B)Acute liver failure
C)Complement-mediated microangiopathy
D)Consumptive coagulopathy
E)Drug-induced thrombocytopenia
F)Vitamin K deficiency

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
73
A 65-year-old man has a cardiac arrest in a shopping mall. Resuscitation is initiated in the field, and the patient is successfully defibrillated. In the emergency department, he is found to have ST segment elevations in the inferior leads and then has an episode of sustained ventricular tachycardia that is treated with intravenous amiodarone. The patient is taken to the cardiac catheterization lab and is found to have a thrombotic occlusion of the right coronary artery, which is successfully treated with percutaneous coronary intervention. On the second day of hospitalization he demonstrates full neurologic recovery and is asymptomatic. Laboratory results are as follows:  The patient's laboratory results were within normal limits 1 week prior to admission. Which of the following is the most likely cause of the new findings?
The patient's laboratory results were within normal limits 1 week prior to admission. Which of the following is the most likely cause of the new findings?
A)Acalculous cholecystitis
B)Acute viral hepatitis
C)Hepatocyte ischemia
D)Medication-induced liver injury
E)Muscle injury
 The patient's laboratory results were within normal limits 1 week prior to admission. Which of the following is the most likely cause of the new findings?
The patient's laboratory results were within normal limits 1 week prior to admission. Which of the following is the most likely cause of the new findings?A)Acalculous cholecystitis
B)Acute viral hepatitis
C)Hepatocyte ischemia
D)Medication-induced liver injury
E)Muscle injury

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
74
A 78-year-old woman is brought from the nursing home to the emergency department due to worsening abdominal distension. Over the past 3 days, the patient has had decreased appetite and progressive abdominal distension that is now accompanied by diffuse abdominal discomfort. Her last bowel movement was 4 days ago. Medical history is significant for dementia, hypertension, osteoarthritis, osteoporosis, and chronic constipation. Surgical history includes open appendectomy and open cholecystectomy. Temperature is 37 C (98.6 F), blood pressure is 138/80 mm Hg, and pulse is 92/min. Physical examination shows a distended and tympanitic abdomen with diffuse tenderness to palpation but no rigidity or rebound tenderness. Blood counts and serum electrolytes are within normal limits. Abdominal x-ray is shown in the exhibit.  Which of the following is the best next step in management of this patient?
Which of the following is the best next step in management of this patient?
A)Emergency total abdominal colectomy
B)Manual disimpaction and laxative therapy
C)Nasogastric decompression and bowel rest only
D)Therapeutic flexible sigmoidoscopy
E)Upper gastrointestinal series with small-bowel follow-through
 Which of the following is the best next step in management of this patient?
Which of the following is the best next step in management of this patient?A)Emergency total abdominal colectomy
B)Manual disimpaction and laxative therapy
C)Nasogastric decompression and bowel rest only
D)Therapeutic flexible sigmoidoscopy
E)Upper gastrointestinal series with small-bowel follow-through

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
75
A 37-year-old man comes to the emergency department due to 2 days of progressive, colicky abdominal pain, abdominal distension, nausea, and vomiting. He had a similar episode 2 years ago that resolved spontaneously and did not require medical attention. He has no chronic medical conditions. Temperature is 36.8 C (98.2 F), blood pressure is 122/80 mm Hg, and pulse is 92/min. The abdomen is distended and tender without rigidity or guarding. Abdominal x-ray is shown in the image below: 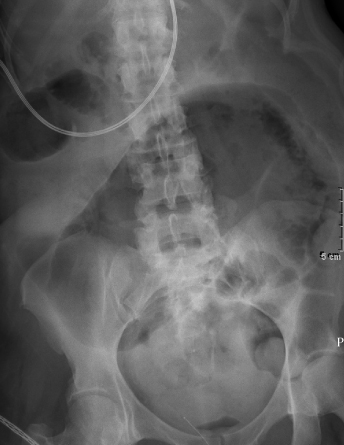 Which of the following is the most likely diagnosis?
Which of the following is the most likely diagnosis?
A)Cecal volvulus
B)Gastric outlet obstruction
C)Ileocolic intussusception
D)Paralytic ileus
E)Toxic megacolon
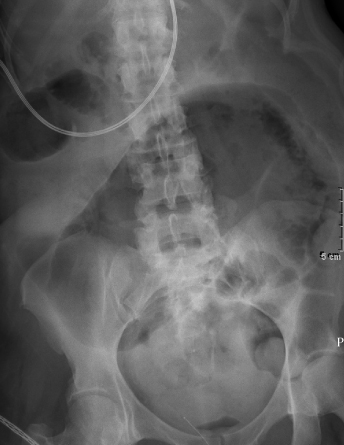 Which of the following is the most likely diagnosis?
Which of the following is the most likely diagnosis?A)Cecal volvulus
B)Gastric outlet obstruction
C)Ileocolic intussusception
D)Paralytic ileus
E)Toxic megacolon

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
76
A 52-year-old woman comes to the emergency department for rectal pain that started 2 hours ago. The pain is described as severe, burning, and exacerbated while sitting. Medical history is significant for chronic idiopathic constipation, for which she takes a fiber supplement. The patient has 4 children, all of whom were vaginally delivered. Family history is unremarkable. She does not use tobacco, alcohol, or illicit drugs. Temperature is 37.2 (99 F), blood pressure is 138/84 mm Hg, and pulse is 90/min. On physical examination, the patient appears in moderate distress due to pain. The abdomen is soft, nondistended, and nontender. Bowel sounds are normoactive. Anal examination reveals a small, exquisitely tender, bluish lesion at the anal verge. Which of the following is the most likely diagnosis?
A)Condyloma acuminata
B)Crohn disease
C)Perianal abscess
D)Prolapsed internal hemorrhoid
E)Rectal prolapse
F)Thrombosed external hemorrhoid
A)Condyloma acuminata
B)Crohn disease
C)Perianal abscess
D)Prolapsed internal hemorrhoid
E)Rectal prolapse
F)Thrombosed external hemorrhoid

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
77
A 55-year-old man comes to the emergency department due to rectal pain. The pain, which is described as excruciating and unrelenting, started abruptly 2 hours ago while the patient was having a bowel movement. He denies fevers, abdominal pain, hematochezia, or unexpected weight loss. Medical history is significant for chronic constipation. Temperature is 37.5 C (99.5 F), blood pressure is 125/75 mm Hg, pulse is 75/min, and respirations are 12/min. The abdomen is nontender and nondistended. Rectal examination reveals an exquisitely tender, purplish bulge just below the dentate line. Which of the following is the immediate next step in management?
A)Hemorrhoidectomy under local anesthesia
B)Infrared coagulation
C)Rubber band ligation
D)Stool softeners and antispasmodics alone
E)Stool softeners, antispasmodics, and antibiotics
A)Hemorrhoidectomy under local anesthesia
B)Infrared coagulation
C)Rubber band ligation
D)Stool softeners and antispasmodics alone
E)Stool softeners, antispasmodics, and antibiotics

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
78
A 24-year-old woman is brought to the emergency department (ED) after a motor vehicle collision. She was the passenger in a vehicle that collided with an 18-wheeler. Paramedics state that the patient was ejected from the vehicle and found on the side of the road. They placed 2 large-bore intravenous lines, infused 1 L of crystalloid, and transported her to the ED. Blood pressure is 80/50 mm Hg, pulse is 138/min, and respirations are 24/min. On examination, the eyes are closed, and the patient is moaning. Auscultation of the lungs reveals decreased breath sounds on the right. The abdomen is tender in the right and left upper quadrants. The patient has an obvious deformity of the left thigh. The extremities are cold and clammy. Chest x-ray reveals a right hemothorax. Focused assessment with sonography for trauma examination shows evidence of free fluid in the right and left upper quadrants. A right chest tube is placed, and 1.5 L of blood is returned. Which of the following is the best next step in management?
A)Administer an additional liter of crystalloid
B)Administer a vasopressor
C)Transfuse group O, Rh D-negative packed red blood cells
D)Transfuse group O, Rh D-positive packed red blood cells
E)Transfuse type-specific packed red blood cells after type and cross-matching
A)Administer an additional liter of crystalloid
B)Administer a vasopressor
C)Transfuse group O, Rh D-negative packed red blood cells
D)Transfuse group O, Rh D-positive packed red blood cells
E)Transfuse type-specific packed red blood cells after type and cross-matching

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
79
A 54-year-old man comes to the emergency department after 2 days of fever, chills, dysphagia, and drooling. The patient has been unable to eat or drink due to pain in his mouth and neck. He has a history of heavy alcohol use but does not use recreational drugs. Temperature is 38.8 C (101.8 F), blood pressure is 110/70 mm Hg, pulse is 108/min, and respirations are 22/min. The patient appears toxic with drooling and a muffled voice. The tongue is displaced posteriorly and superiorly due to a swollen area on the floor of the mouth. The bilateral submandibular area is tender, indurated, and nonfluctuant with palpable crepitus. Which of the following is the most likely source of infection in this patient?
A)Bloodstream
B)Epiglottis
C)Lymph nodes
D)Palatine tonsils
E)Parotid glands
F)Teeth roots
A)Bloodstream
B)Epiglottis
C)Lymph nodes
D)Palatine tonsils
E)Parotid glands
F)Teeth roots

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck
80
A 21-year-old man is brought to the emergency department after being stepped on by a bull approximately 30 minutes ago. The patient was bucked off of the bull, whose hind feet landed on his chest. On arrival, blood pressure is 75/50 mm Hg, pulse is 140/min, and respirations are 24/min. On examination, the patient moans in pain but does not answer questions. Two hoof prints are seen in the middle of the chest. He has decreased bilateral breath sounds, and crepitus is present over the anterior chest walls bilaterally. The abdomen is soft and nondistended. There is no obvious injury to the extremities, but they are cool, and capillary refill is decreased. Bilateral chest tubes are immediately placed, and 1.5 L of blood is returned from each side. Vital signs do not improve after placement of chest tubes. Four units of packed red blood cells are prepared for transfusion. What other blood products, if any, should also be administered at this time?
A)4 units of cryoprecipitate only
B)4 units of fresh frozen plasma and 4 units of platelets
C)4 units of fresh frozen plasma only
D)4 units of platelets only
E)No additional blood products
A)4 units of cryoprecipitate only
B)4 units of fresh frozen plasma and 4 units of platelets
C)4 units of fresh frozen plasma only
D)4 units of platelets only
E)No additional blood products

Unlock Deck
Unlock for access to all 563 flashcards in this deck.
Unlock Deck
k this deck



