Deck 13: Cardiovascular Diagnostic Procedures
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question
Question

Unlock Deck
Sign up to unlock the cards in this deck!
Unlock Deck
Unlock Deck
1/74
Play
Full screen (f)
Deck 13: Cardiovascular Diagnostic Procedures
1
What major clinical finding present in a patient with ventricular fibrillation (VF)?
A) Hypertension
B) Bradycardia
C) Diaphoresis
D) Pulselessness
A) Hypertension
B) Bradycardia
C) Diaphoresis
D) Pulselessness
Pulselessness
2
Which criteria are representative of the patient in normal sinus rhythm?
A) Heart rate, 64 beats/min; rhythm regular; PR interval, 0.10 second; QRS, 0.04 second
B) Heart rate, 88 beats/min; rhythm regular; PR interval, 0.18 second; QRS, 0.06 second
C) Heart rate, 54 beats/min; rhythm regular; PR interval, 0.16 second; QRS, 0.08 second
D) Heart rate, 92 beats/min; rhythm irregular; PR interval, 0.16 second; QRS, 0.04 second
A) Heart rate, 64 beats/min; rhythm regular; PR interval, 0.10 second; QRS, 0.04 second
B) Heart rate, 88 beats/min; rhythm regular; PR interval, 0.18 second; QRS, 0.06 second
C) Heart rate, 54 beats/min; rhythm regular; PR interval, 0.16 second; QRS, 0.08 second
D) Heart rate, 92 beats/min; rhythm irregular; PR interval, 0.16 second; QRS, 0.04 second
Heart rate, 88 beats/min; rhythm regular; PR interval, 0.18 second; QRS, 0.06 second
3
A patient reports that he has been having "indigestion" for the last few hours.Upon further review the nurse suspects the patient is having of chest pain.Cardiac biomarkers and a 12-lead electrocardiogram (ECG)are done.What finding is most significant in diagnosing an acute coronary syndrome (ACS)within the first 3 hours?
A) Inverted T waves
B) Elevated troponin I
C) Elevated B-type natriuretic peptide (BNP)
D) Indigestion and chest pain
A) Inverted T waves
B) Elevated troponin I
C) Elevated B-type natriuretic peptide (BNP)
D) Indigestion and chest pain
Elevated troponin I
4
Pulsus paradoxus may be noted on the bedside monitor when what is observed?
A) A decrease of more than 10 mm Hg in the arterial waveform during inhalation
B) A single, nonperfused beat on the electrocardiogram (ECG) waveform
C) Tall, tented T waves on the ECG waveform
D) An increase in pulse pressure greater than 20 mm Hg on exhalation
A) A decrease of more than 10 mm Hg in the arterial waveform during inhalation
B) A single, nonperfused beat on the electrocardiogram (ECG) waveform
C) Tall, tented T waves on the ECG waveform
D) An increase in pulse pressure greater than 20 mm Hg on exhalation

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
5
A patient with a serum potassium level of 6.8 mEq/L may exhibit what type of electrocardiographic changes?
A) A prominent U wave
B) Tall, peaked T waves
C) A narrowed QRS
D) Sudden ventricular dysrhythmias
A) A prominent U wave
B) Tall, peaked T waves
C) A narrowed QRS
D) Sudden ventricular dysrhythmias

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
6
ST segment monitoring for ischemia has gained increasing importance with the advent of thrombolytic therapy.What is the most accurate method for monitoring the existence of true ischemic changes?
A) Biomarkers
B) Echocardiogram
C) 5-lead ECG
D) 12-lead ECG
A) Biomarkers
B) Echocardiogram
C) 5-lead ECG
D) 12-lead ECG

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
7
Why is mixed venous oxygen saturation (SVO₂)monitoring helpful in the management of the critically ill patient?
A) It facilitates oxygen saturation monitoring at the capillary level.
B) It can detect an imbalance between oxygen supply and metabolic tissue demand.
C) It assesses the diffusion of gases at the alveolar capillary membrane.
D) It estimates myocardial workload during heart failure and acute pulmonary edema.
A) It facilitates oxygen saturation monitoring at the capillary level.
B) It can detect an imbalance between oxygen supply and metabolic tissue demand.
C) It assesses the diffusion of gases at the alveolar capillary membrane.
D) It estimates myocardial workload during heart failure and acute pulmonary edema.

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
8
What parameter is used to assess the contractility of the left side of the heart?
A) Pulmonary artery occlusion pressure
B) Left atrial pressure
C) Systemic vascular resistance
D) Left ventricular stroke work index
A) Pulmonary artery occlusion pressure
B) Left atrial pressure
C) Systemic vascular resistance
D) Left ventricular stroke work index

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
9
When assessing a patient with PVCs,the nurse knows that the ectopic beat is multifocal because it appears in what way?
A) In various shapes in the same lead
B) With increasing frequency
C) Wider than a normal QRS
D) On the T wave
A) In various shapes in the same lead
B) With increasing frequency
C) Wider than a normal QRS
D) On the T wave

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
10
What is the major factor influencing the patient's response to atrial flutter?
A) Atrial rate
B) Ventricular response rate
C) PR interval
D) QRS duration
A) Atrial rate
B) Ventricular response rate
C) PR interval
D) QRS duration

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
11
When assessing the pulmonary arterial waveform,the nurse notices dampening.After tightening the stopcocks and flushing the line,the nurse decides to calibrate the transducer.What are two essential components included in calibration?
A) Obtaining a baseline blood pressure and closing the transducer to air
B) Leveling the air-fluid interface to the phlebostatic axis and opening the transducer to air
C) Having the patient lay flat and closing the transducer to air
D) Obtaining blood return on line and closing all stopcocks
A) Obtaining a baseline blood pressure and closing the transducer to air
B) Leveling the air-fluid interface to the phlebostatic axis and opening the transducer to air
C) Having the patient lay flat and closing the transducer to air
D) Obtaining blood return on line and closing all stopcocks

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
12
A patient with heart failure may be at risk for hypomagnesemia as a result of which factor?
A) Pump failure
B) Diuretic use
C) Fluid overload
D) Hemodilution
A) Pump failure
B) Diuretic use
C) Fluid overload
D) Hemodilution

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
13
What is the formula for calculating mean arterial pressure (MAP)?
A) Averaging three of the patient's blood pressure readings over a 6-hour period
B) Dividing the systolic pressure by the diastolic pressure
C) Adding the systolic pressure and two diastolic pressures and then dividing by 3
D) Dividing the diastolic pressure by the pulse pressure
A) Averaging three of the patient's blood pressure readings over a 6-hour period
B) Dividing the systolic pressure by the diastolic pressure
C) Adding the systolic pressure and two diastolic pressures and then dividing by 3
D) Dividing the diastolic pressure by the pulse pressure

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
14
Which portion of the electrocardiogram (ECG)is most valuable in diagnosing atrioventricular (AV)conduction disturbances?
A) P wave
B) PR interval
C) QRS complex
D) QT interval
A) P wave
B) PR interval
C) QRS complex
D) QT interval

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
15
What is the rationale for giving the patient additional fluids after a cardiac catheterization?
A) Fluids help keep the femoral vein from clotting at the puncture site.
B) The patient had a nothing-by-mouth order before the procedure.
C) The radiopaque contrast acts as an osmotic diuretic.
D) Fluids increase cardiac output.
A) Fluids help keep the femoral vein from clotting at the puncture site.
B) The patient had a nothing-by-mouth order before the procedure.
C) The radiopaque contrast acts as an osmotic diuretic.
D) Fluids increase cardiac output.

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
16
Which findings would be reasons to abort an exercise stress test?
A) Ventricular axis of +90 degrees
B) Increase in blood pressure
C) Inverted U wave
D) ST segment depression or elevation
A) Ventricular axis of +90 degrees
B) Increase in blood pressure
C) Inverted U wave
D) ST segment depression or elevation

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
17
Which intervention should be strictly followed to ensure accurate cardiac output readings?
A) Inject 5 mL of iced injectate at the beginning of exhalation over 30 seconds.
B) Inject 10 mL of warmed injectate into the pulmonary artery port three times.
C) Ensure at least 5° C difference between injectate and the patient temperature.
D) Administer the injectate within 4 seconds during inspiration.
A) Inject 5 mL of iced injectate at the beginning of exhalation over 30 seconds.
B) Inject 10 mL of warmed injectate into the pulmonary artery port three times.
C) Ensure at least 5° C difference between injectate and the patient temperature.
D) Administer the injectate within 4 seconds during inspiration.

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
18
What is the physiologic effect of left ventricular afterload reduction?
A) Decreased left atrial tension
B) Decreased systemic vascular resistance
C) Increased filling pressures
D) Decreased cardiac output
A) Decreased left atrial tension
B) Decreased systemic vascular resistance
C) Increased filling pressures
D) Decreased cardiac output

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
19
What characteristic is associated with junctional escape rhythms?
A) Irregular rhythm
B) Rate greater than 100 beats/min
C) P wave may be present or absent
D) QRS greater than 0.10 seconds
A) Irregular rhythm
B) Rate greater than 100 beats/min
C) P wave may be present or absent
D) QRS greater than 0.10 seconds

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
20
Which diagnostic test is most effective for measuring overall heart size?
A) 12-lead electrocardiography
B) Echocardiography
C) Chest radiography
D) Vectorcardiography
A) 12-lead electrocardiography
B) Echocardiography
C) Chest radiography
D) Vectorcardiography

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
21
A patient returns from the cardiac catheterization laboratory after angioplasty and stent placement (ECG changes had indicated an inferior wall myocardial infarction in progress).Which lead would best monitor this patient?
A) Varies based on the patient's clinical condition and recent clinical history
B) Lead V3
C) Lead V1
D) Lead II
A) Varies based on the patient's clinical condition and recent clinical history
B) Lead V3
C) Lead V1
D) Lead II

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
22
Which lead is best to monitor a patient?
A) Varies based on the patient's clinical condition and recent clinical history
B) Lead aVF
C) Lead V1
D) Lead II
A) Varies based on the patient's clinical condition and recent clinical history
B) Lead aVF
C) Lead V1
D) Lead II

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
23
The physician is going to place a central venous catheter.Which anatomic site is associated with a lower risk of infection?
A) Subclavian vein
B) External jugular vein
C) Internal jugular vein
D) Femoral vein
A) Subclavian vein
B) External jugular vein
C) Internal jugular vein
D) Femoral vein

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
24
A patient's bedside electrocardiogram (ECG)strips show the following changes: increased PR interval; increased QRS width; and tall,peaked T waves.Vital signs are temperature 98.2° F; heart rate 118 beats/min; blood pressure 146/90 mm Hg; and respiratory rate 18 breaths/min.The patient is receiving the following medications: digoxin 0.125 mg PO every day; D₅1/2 normal saline with 40 mEq potassium chloride at 125 mL/hr; Cardizem at 30 mg PO q8h; and aldosterone at 300 mg PO q12h.The practitioner is notified of the ECG changes.What orders should the nurse expect to receive?
A) Change IV fluid to D51/2 normal saline and draw blood chemistry.
B) Give normal saline with 40 mEq of potassium chloride over a 6-hour period.
C) Hold digoxin and draw serum digoxin level.
D) Hold Cardizem and give 500 mL normal saline fluid challenge over a 2-hour period.
A) Change IV fluid to D51/2 normal saline and draw blood chemistry.
B) Give normal saline with 40 mEq of potassium chloride over a 6-hour period.
C) Hold digoxin and draw serum digoxin level.
D) Hold Cardizem and give 500 mL normal saline fluid challenge over a 2-hour period.

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
25
Most chest radiographs of critically ill patients are obtained using a portable chest radiograph machine.What is the difference between a chest radiograph taken in the radiology department and one taken in the critical care unit?
A) Portable chest radiographs are usually clearer.
B) Only posterior views can be obtained in the critical care unit.
C) The sharpness of the structures is decreased with a portable chest radiograph.
D) Chest radiographs taken in radiology enlarge some thoracic structures.
A) Portable chest radiographs are usually clearer.
B) Only posterior views can be obtained in the critical care unit.
C) The sharpness of the structures is decreased with a portable chest radiograph.
D) Chest radiographs taken in radiology enlarge some thoracic structures.

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
26
Which of the electrocardiogram (ECG)findings would be positive for an inferior wall myocardial infarction (MI)?
A) ST segment depression in leads I, aVL, and V2 to V4
B) Q waves in leads V1 to V2
C) Q waves in leads II, III, and aVF
D) T-wave inversion in leads V4 to V6, I, and aVL
A) ST segment depression in leads I, aVL, and V2 to V4
B) Q waves in leads V1 to V2
C) Q waves in leads II, III, and aVF
D) T-wave inversion in leads V4 to V6, I, and aVL

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
27
Why is the measurement of the QT interval important?
A) It facilitates rhythm identification and is best assessed in Lead II.
B) It helps differentiate myocardial ischemia from infarction.
C) An increasing QT interval increases the risk of torsades de pointes.
D) A decreasing QT interval increases the risk of torsades de pointes.
A) It facilitates rhythm identification and is best assessed in Lead II.
B) It helps differentiate myocardial ischemia from infarction.
C) An increasing QT interval increases the risk of torsades de pointes.
D) A decreasing QT interval increases the risk of torsades de pointes.

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
28
What does the P wave component of the electrocardiographic waveform represent?
A) Atrial contraction
B) Atrial depolarization
C) Sinus node discharge
D) Ventricular contraction
A) Atrial contraction
B) Atrial depolarization
C) Sinus node discharge
D) Ventricular contraction

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
29
To accurately measure the heart rate of a patient in normal sinus rhythm,which technique would be the most accurate?
A) The number of R waves in a 6-second strip
B) The number of large boxes in a 6-second strip
C) The number of small boxes between QRS complexes divided into 1500
D) The number of large boxes between consecutive R waves divided into 300
A) The number of R waves in a 6-second strip
B) The number of large boxes in a 6-second strip
C) The number of small boxes between QRS complexes divided into 1500
D) The number of large boxes between consecutive R waves divided into 300

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
30
A patient with a potassium level of 2.8 mEq/L is given 60 mEq over a 12-hour period.A repeat potassium level is obtained,and the current potassium level is 3.2 mEq/L.In addition to administering additional potassium supplements,what intervention should now be considered?
A) Discontinue spironolactone
B) Drawing a serum magnesium level
C) Rechecking the potassium level
D) Monitoring the patient's urinary output
A) Discontinue spironolactone
B) Drawing a serum magnesium level
C) Rechecking the potassium level
D) Monitoring the patient's urinary output

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
31
When performing a 12-lead electrocardiogram (ECG),how many wires are connected to the patient?
A) 3
B) 5
C) 10
D) 12
A) 3
B) 5
C) 10
D) 12

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
32
The patient's admitting 12-lead ECG shows tall,peaked P waves.What diagnosis could be responsible for this finding?
A) Mitral stenosis
B) Pulmonary edema
C) Ischemia
D) Pericarditis
A) Mitral stenosis
B) Pulmonary edema
C) Ischemia
D) Pericarditis

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
33
A physician orders removal of the central venous catheter (CVC)line.The patient has a diagnosis of heart failure with chronic obstructive pulmonary disease.The nurse would place the patient in what position for this procedure?
A) Supine in bed
B) Supine in a chair
C) Flat in bed
D) Reverse Trendelenburg position
A) Supine in bed
B) Supine in a chair
C) Flat in bed
D) Reverse Trendelenburg position

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
34
Which serum lipid value is a significant predictor of future acute myocardial infarction (MI)in persons with established coronary artery atherosclerosis?
A) High-density lipoprotein (HDL)
B) Low-density lipoprotein (LDL)
C) Triglycerides
D) Very-low-density lipoprotein
A) High-density lipoprotein (HDL)
B) Low-density lipoprotein (LDL)
C) Triglycerides
D) Very-low-density lipoprotein

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
35
A new-onset myocardial infarction (MI)can be recognized by what electrocardiogram (ECG)change?
A) Q waves
B) Smaller R waves
C) Widened QRS
D) ST segment elevation
A) Q waves
B) Smaller R waves
C) Widened QRS
D) ST segment elevation

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
36
What is the most common complication of a central venous catheter (CVC)?
A) Air embolus
B) Infection
C) Thrombus formation
D) Pneumothorax
A) Air embolus
B) Infection
C) Thrombus formation
D) Pneumothorax

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
37
Mechanical contraction of the heart occurs during which phase of the cardiac cycle?
A) Phase 0
B) Phase 2
C) Phase 3
D) Phase 4
A) Phase 0
B) Phase 2
C) Phase 3
D) Phase 4

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
38
Which cardiac biomarker is elevated in decompensated heart failure?
A) Triglycerides
B) Troponin I
C) Troponin T
D) B-type natriuretic peptide (BNP)
A) Triglycerides
B) Troponin I
C) Troponin T
D) B-type natriuretic peptide (BNP)

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
39
A patient asks why he had to take a deep breath when the radiology technician took his chest radiograph.Which statement is the best response?
A) "Deep breaths get the chest wall closer to the machine."
B) "When the lungs are filled with air, you get a clearer picture."
C) "Taking a deep breath decreases the error caused by motion."
D) "Holding your breath makes the heart appear larger."
A) "Deep breaths get the chest wall closer to the machine."
B) "When the lungs are filled with air, you get a clearer picture."
C) "Taking a deep breath decreases the error caused by motion."
D) "Holding your breath makes the heart appear larger."

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
40
A nurse is obtaining the history of a patient who reveals that he had an myocardial infarction (MI)5 years ago.When the admission 12-lead electrocardiogram (ECG)is reviewed,Q waves are noted in leads V3 and V4 only.Which conclusion is most consistent with this situation?
A) The patient may have had a posterior wall MI.
B) The patient must have had a right ventricular MI.
C) The admission 12-lead ECG was done incorrectly.
D) The patient may have had an anterior MI.
A) The patient may have had a posterior wall MI.
B) The patient must have had a right ventricular MI.
C) The admission 12-lead ECG was done incorrectly.
D) The patient may have had an anterior MI.

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
41
What is the initial intervention in a patient with sinus tachycardia with the following vital signs: heart rate,136 beats/min; blood pressure,102/60 mm Hg; respiratory rate,24 breaths/min; temperature,99.2° F; SpO₂,94% on oxygen 2 L/min by nasal cannula?
A) Administer adenosine IV push.
B) Identify the cause.
C) Administer nitroglycerine 0.4 mg sublingual.
D) Administer lidocaine 75 mg IV push.
A) Administer adenosine IV push.
B) Identify the cause.
C) Administer nitroglycerine 0.4 mg sublingual.
D) Administer lidocaine 75 mg IV push.

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
42
Zeroing the pressure transducer on hemodynamic monitoring equipment occurs when the displays reads which number?
A) 0
B) 250
C) 600
D) 760
A) 0
B) 250
C) 600
D) 760

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
43
After a myocardial infarction,a patient presents with an increasing frequency of premature ventricular contractions (PVCs).The patient's heart rate is 110 beats/min,and electrocardiogram (ECG)indicates a sinus rhythm with up to five unifocal PVCs per minute.The patient is alert and responsive and denies any chest pain or dyspnea.What action should the nurse take next?
A) Administer lidocaine 100 mg bolus IV push stat.
B) Administer Cardizem 20 mg IV push stat.
C) Notify the physician and monitor the patient closely.
D) Nothing; PVCs are expected in this patient.
A) Administer lidocaine 100 mg bolus IV push stat.
B) Administer Cardizem 20 mg IV push stat.
C) Notify the physician and monitor the patient closely.
D) Nothing; PVCs are expected in this patient.

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
44
Which blood test standardizes prothrombin time (PT)results among worldwide clinical laboratories?
A) aPTT
B) ACT
C) HDL
D) INR
A) aPTT
B) ACT
C) HDL
D) INR

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
45
A positive signal-averaged electrocardiogram (ECG)indicates that a patient is at risk for what problem?
A) Myocardial infarction
B) Sudden cardiac death
C) Coronary artery disease
D) Stroke
A) Myocardial infarction
B) Sudden cardiac death
C) Coronary artery disease
D) Stroke

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
46
What effect does ventricular tachycardia have on cardiac output?
A) Increases cardiac output due to an increase in ventricular filling time
B) Decreases cardiac output due to a decrease in stroke volume
C) Increases cardiac output due to an increase in preload
D) Decreases cardiac output due to a decrease in afterload
A) Increases cardiac output due to an increase in ventricular filling time
B) Decreases cardiac output due to a decrease in stroke volume
C) Increases cardiac output due to an increase in preload
D) Decreases cardiac output due to a decrease in afterload

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
47
What is the target range for an international normalized ratio (INR)?
A) 1.0 to 2.0
B) 1.5 to 3.0
C) 1.5 to 2.5
D) 2.0 to 3.0
A) 1.0 to 2.0
B) 1.5 to 3.0
C) 1.5 to 2.5
D) 2.0 to 3.0

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
48
Which electrocardiographic (ECG)abnormality is most often found in ventricular dysrhythmias?
A) Retrograde P waves
B) Wide QRS complexes
C) No P waves
D) An inverted T wave
A) Retrograde P waves
B) Wide QRS complexes
C) No P waves
D) An inverted T wave

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
49
The patient has a heart rate (HR)of 84 beats/min and a stroke volume (SV)of 65 mL.Calculate the cardiac output (CO).
A) 149 mL
B) 500 mL
C) 4650 mL
D) 5460 mL
A) 149 mL
B) 500 mL
C) 4650 mL
D) 5460 mL

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
50
Which statement made by a patient would indicate the need for further education before an electrophysiology procedure?
A) "I need to take all my heart medications the morning of the procedure."
B) "The doctor is going to make my heart beat wrong on purpose."
C) "I will be awake but relaxed during the procedure."
D) "I will be x-rayed during the procedure."
A) "I need to take all my heart medications the morning of the procedure."
B) "The doctor is going to make my heart beat wrong on purpose."
C) "I will be awake but relaxed during the procedure."
D) "I will be x-rayed during the procedure."

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
51
A patient becomes unresponsive.The patient's heart rate is 32 beats/min in an idioventricular rhythm; blood pressure is 60/32 mm Hg; SpO₂ is 90%; and respiratory rate is 14 breaths/min.Which intervention would the nurse do first?
A) Notify the physician and hang normal saline wide open.
B) Notify the physician and obtain the defibrillator.
C) Notify the physician and obtain a temporary pacemaker.
D) Notify the physician and obtain a 12-lead ECG.
A) Notify the physician and hang normal saline wide open.
B) Notify the physician and obtain the defibrillator.
C) Notify the physician and obtain a temporary pacemaker.
D) Notify the physician and obtain a 12-lead ECG.

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
52
The patient is admitted with a diagnosis of cardiogenic shock.The patient's heart rate (HR)is 135 beats/min with weak peripheral pulses.The patient has bilaterally crackles in the bases of the lungs.O₂ saturation is 90% on 4L/NC.The practitioner orders diuretics and vasodilators.What response should the nurse expect after starting the medications?
A) Decreased preload and afterload
B) Increased preload and afterload
C) Decreased preload and increased afterload
D) Increased preload and decreased afterload
A) Decreased preload and afterload
B) Increased preload and afterload
C) Decreased preload and increased afterload
D) Increased preload and decreased afterload

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
53
On returning from the cardiac catheterization laboratory,the patient asks if he can get up in the chair.What should the nurse tell the patient?
A) "You cannot get up because you may pass out."
B) "You cannot get up because you may start bleeding."
C) "You cannot get up because you may fall."
D) "You cannot get up until you urinate."
A) "You cannot get up because you may pass out."
B) "You cannot get up because you may start bleeding."
C) "You cannot get up because you may fall."
D) "You cannot get up until you urinate."

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
54
Which diagnostic tool can be used to detect structural heart abnormalities?
A) Echocardiogram
B) Electrocardiogram (ECG)
C) Exercise stress test
D) 24-hour Holter monitor
A) Echocardiogram
B) Electrocardiogram (ECG)
C) Exercise stress test
D) 24-hour Holter monitor

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
55
What type of atrioventricular (AV)block can be described as a gradually lengthening PR interval until ultimately the final P wave in the group fails to conduct?
A) First-degree AV block
B) Second-degree AV block, type I
C) Second-degree AV block, type II
D) Third-degree AV block
A) First-degree AV block
B) Second-degree AV block, type I
C) Second-degree AV block, type II
D) Third-degree AV block

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
56
Why is a new-onset of atrial fibrillation serious?
A) It increases the patient's risk for a stroke.
B) It increases the patient's risk for a deep venous thrombosis.
C) It may increase cardiac output to dangerous levels.
D) It indicates the patient is about to have a myocardial infarction.
A) It increases the patient's risk for a stroke.
B) It increases the patient's risk for a deep venous thrombosis.
C) It may increase cardiac output to dangerous levels.
D) It indicates the patient is about to have a myocardial infarction.

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
57
A patient presents with atrial flutter with an atrial rate of 280 beats/min and a ventricular rate of 70 beats/min.Which statement best explains this discrepancy in rates?
A) The ventricles are too tired to respond to all the atrial signals.
B) The atrioventricular (AV) node does not conduct all the atrial signals to the ventricles.
C) Some of the atrial beats are blocked before reaching the AV node.
D) The ventricles are responding to a ventricular ectopic pacemaker.
A) The ventricles are too tired to respond to all the atrial signals.
B) The atrioventricular (AV) node does not conduct all the atrial signals to the ventricles.
C) Some of the atrial beats are blocked before reaching the AV node.
D) The ventricles are responding to a ventricular ectopic pacemaker.

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
58
Why is the Allen test performed before placement of a radial arterial line placement?
A) To evaluate collateral circulation to the hand
B) To estimate patency of the radial artery
C) To appraise the neurologic function of the hand
D) To assess the sensitivity of the insertion point
A) To evaluate collateral circulation to the hand
B) To estimate patency of the radial artery
C) To appraise the neurologic function of the hand
D) To assess the sensitivity of the insertion point

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
59
A patient's central venous pressure (CVP)reading suddenly increased from 10 to 48 mm Hg.His lungs are clear except for fine rales at the bases.What should the nurse do next?
A) Nothing as this reading is still within normal limits.
B) Place a STAT call into the physician.
C) Administer ordered prn Lasix.
D) Check the level of the transducer.
A) Nothing as this reading is still within normal limits.
B) Place a STAT call into the physician.
C) Administer ordered prn Lasix.
D) Check the level of the transducer.

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
60
Which statement expresses the correct order when working with an invasive pressure monitor?
A) Level the transducer, locate the phlebostatic axis, zero the transducer, and take the reading.
B) Locate the phlebostatic axis, level the transducer, zero the transducer, and take the reading.
C) Take the reading, level the transducer, locate the phlebostatic axis, and zero the transducer.
D) Locate the phlebostatic axis, zero the transducer, level the transducer, and take the reading.
A) Level the transducer, locate the phlebostatic axis, zero the transducer, and take the reading.
B) Locate the phlebostatic axis, level the transducer, zero the transducer, and take the reading.
C) Take the reading, level the transducer, locate the phlebostatic axis, and zero the transducer.
D) Locate the phlebostatic axis, zero the transducer, level the transducer, and take the reading.

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
61
The patient's admitting 12-lead ECG shows wide,M-shaped P waves.What diagnosis could be responsible for this finding?
A) Mitral stenosis
B) Chronic pulmonary disease
C) Hypotension
D) Pericarditis
A) Mitral stenosis
B) Chronic pulmonary disease
C) Hypotension
D) Pericarditis

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
62
What is the effect of preload on cardiac output?
A) As preload increases, cardiac output increases.
B) As preload increases, cardiac output decreases.
C) As preload increases, cardiac output increases until it overstretches the ventricle and cardiac output decreases.
D) Increased preload has no effect on cardiac output.
A) As preload increases, cardiac output increases.
B) As preload increases, cardiac output decreases.
C) As preload increases, cardiac output increases until it overstretches the ventricle and cardiac output decreases.
D) Increased preload has no effect on cardiac output.

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
63
Which statement regarding the use of cuff blood pressures is true?
A) Cuff pressures may be unreliable when a patient is in shock.
B) Cuff pressures are more accurate than arterial line pressures.
C) Cuff pressures and arterial line pressures should be nearly identical.
D) Cuff pressures should not be compared to arterial line pressures.
A) Cuff pressures may be unreliable when a patient is in shock.
B) Cuff pressures are more accurate than arterial line pressures.
C) Cuff pressures and arterial line pressures should be nearly identical.
D) Cuff pressures should not be compared to arterial line pressures.

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
64
Identify the rhythm. 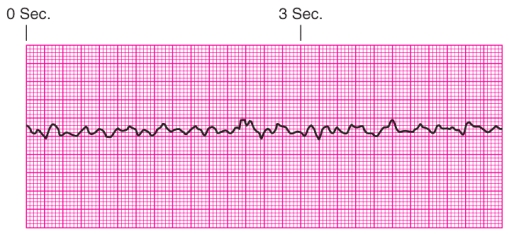
A) Ventricular tachycardia
B) Ventricular fibrillation
C) Supraventricular tachycardia
D) Torsades de pointes
A) Ventricular tachycardia
B) Ventricular fibrillation
C) Supraventricular tachycardia
D) Torsades de pointes

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
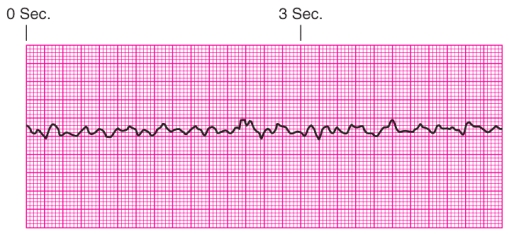
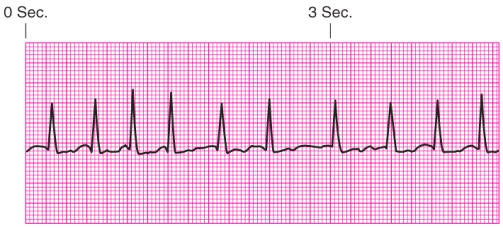
65
Identify the rhythm. 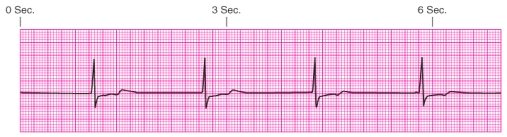
A) Junctional escape rhythm
B) Atrial fibrillation
C) Unifocal premature ventricular contractions
D) Ventricular tachycardia
A) Junctional escape rhythm
B) Atrial fibrillation
C) Unifocal premature ventricular contractions
D) Ventricular tachycardia

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
66
A patient's arterial line waveform has become damped.What action should the nurse take to correct the situation?
A) Check for kinks, blood, and air bubbles in the pressure tubing.
B) Prepare for a normal saline fluid challenge for hypotension.
C) Discontinue the arterial line as it has become nonfunctional.
D) Check the patient's lung sounds for a change in patient condition.
A) Check for kinks, blood, and air bubbles in the pressure tubing.
B) Prepare for a normal saline fluid challenge for hypotension.
C) Discontinue the arterial line as it has become nonfunctional.
D) Check the patient's lung sounds for a change in patient condition.

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
67
Which noninvasive imaging technique is useful in diagnosing complications of a myocardial infarction (MI)?
A) 12-lead ECG
B) CT
C) MRI
D) Echocardiography
A) 12-lead ECG
B) CT
C) MRI
D) Echocardiography

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
68
Which condition can cause an artificial increase in the pulmonary artery occlusion pressure (PAOP)?
A) Aortic regurgitation
B) Aortic stenosis
C) Mitral stenosis
D) Mitral regurgitation
A) Aortic regurgitation
B) Aortic stenosis
C) Mitral stenosis
D) Mitral regurgitation

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
69
Identify the rhythm. 
A) Junctional escape rhythm
B) Atrial fibrillation
C) Unifocal premature ventricular contractions
D) Ventricular tachycardia

A) Junctional escape rhythm
B) Atrial fibrillation
C) Unifocal premature ventricular contractions
D) Ventricular tachycardia

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
70
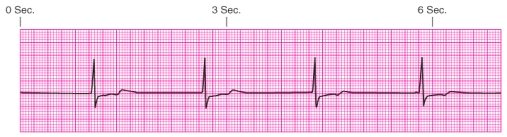
Identify the rhythm. 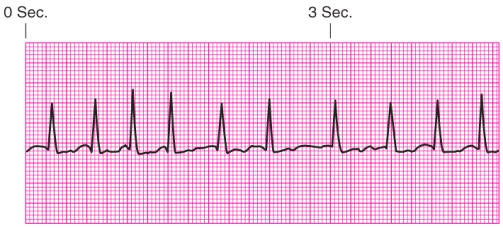
A) Junctional escape rhythm
B) Atrial fibrillation
C) Unifocal premature ventricular contractions
D) Ventricular tachycardia
A) Junctional escape rhythm
B) Atrial fibrillation
C) Unifocal premature ventricular contractions
D) Ventricular tachycardia

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
71
Identify the rhythm. 
A) Junctional escape rhythm
B) Atrial fibrillation
C) Unifocal premature ventricular contractions
D) Ventricular tachycardia

A) Junctional escape rhythm
B) Atrial fibrillation
C) Unifocal premature ventricular contractions
D) Ventricular tachycardia

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
72
Which of the following is most indicative of decreased left ventricular preload?
A) Increased pulmonary artery occlusion pressure (PAOP)
B) Decreased pulmonary artery occlusion pressure (PAOP)
C) Increased central venous pressure (CVP)
D) Decreased central venous pressure (CVP)
A) Increased pulmonary artery occlusion pressure (PAOP)
B) Decreased pulmonary artery occlusion pressure (PAOP)
C) Increased central venous pressure (CVP)
D) Decreased central venous pressure (CVP)

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
73
Patient education for a patient with a Holter monitor should include which instruction?
A) Keep a diary of activities, symptoms, and any medications that are taken.
B) Do not drink coffee while the recorder is on.
C) Do not take a bath but a shower is alright.
D) Carry the monitor in a purse or backpack.
A) Keep a diary of activities, symptoms, and any medications that are taken.
B) Do not drink coffee while the recorder is on.
C) Do not take a bath but a shower is alright.
D) Carry the monitor in a purse or backpack.

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck
74
A 55-year-old patient is scheduled for a stress test.What is the estimation of the patient's maximal predicted heart rate?
A) 65 beats/min
B) 155 beats/min
C) 165 beats/min
D) 265 beats/min
A) 65 beats/min
B) 155 beats/min
C) 165 beats/min
D) 265 beats/min

Unlock Deck
Unlock for access to all 74 flashcards in this deck.
Unlock Deck
k this deck



