A 72-year-old man is brought to the emergency department due to severe, tearing pain in the anterior and posterior areas of his chest for the last 2 hours. The pain is accompanied by diaphoresis and mild shortness of breath. The patient has never experienced similar pain. Stress testing 6 months ago showed mild ischemia in the inferior wall, which was treated medically. Other medical problems include hypertension, hyperlipidemia, gout, and chronic constipation. The patient is a lifelong nonsmoker.
Blood pressure is 80/60 mm Hg in the right arm and 76/47 mm Hg in the left arm, and pulse is 102/min. The jugular veins are distended when the patient is sitting. Heart sounds are distant and no murmurs are heard on cardiac auscultation. The lungs are clear to auscultation. There is no peripheral edema. The extremities are cold, and peripheral pulses are markedly diminished.
ECG performed in the emergency department is shown in the exhibit.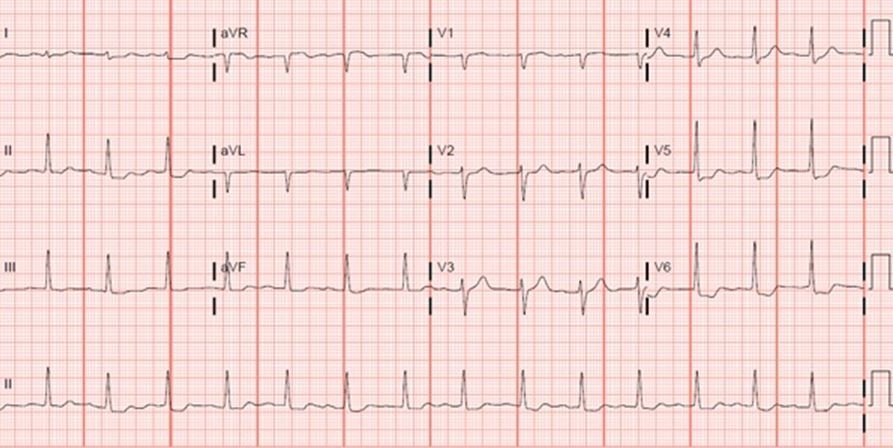
Which of the following is the best next step in management of this patient?
A) Bedside transthoracic echocardiography followed by pericardiocentesis
B) Bedside transthoracic echocardiography followed by transfer to the operating room
C) Cardiac catheterization
D) Conscious sedation followed by transesophageal echocardiography
E) CT scan of the chest with contrast
Correct Answer:
Verified
Q1: A 72-year-old man is seen in the
Q3: A 34-year-old man with history of type
Q4: A 60-year-old woman is brought to the
Q5: A 56-year-old man comes to the physician
Q6: A 62-year-old man comes to the emergency
Q7: A 47-year-old man is brought to the
Q8: A 56-year-old woman comes to the emergency
Q9: A 32-year-old woman, gravida 1 para 0,
Q10: A 34-year-old man is brought to the
Q11: A 66-year-old retired police officer is brought
Unlock this Answer For Free Now!
View this answer and more for free by performing one of the following actions

Scan the QR code to install the App and get 2 free unlocks

Unlock quizzes for free by uploading documents