A 72-year-old woman with diet-controlled type 2 diabetes mellitus is brought to the emergency department for chest pain and shortness of breath. Her initial blood pressure is 132/72 mm Hg and pulse is 102/min. ECG shows sinus tachycardia and a 2 mm horizontal ST segment depression in the anterior precordial leads. A chest x-ray shows bilateral patchy opacities most consistent with congestive heart failure.
She is treated with aspirin, clopidogrel, furosemide, nitroglycerin infusion, and heparin infusion. Non-invasive positive pressure ventilation is initiated. She is taken to the cardiac catheterization lab, and coronary angiography is performed which shows extensive triple vessel coronary artery disease. Pulmonary artery catheter is placed and no coronary artery intervention is performed.
The patient is transferred to the cardiac care unit. Four hours later, her blood pressure is 84/46 mm Hg and pulse is 116/min. Hemodynamic readings from the pulmonary artery catheter are shown below.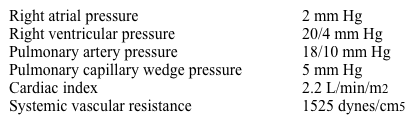
Which of the following is the most likely cause of this patient's hypotension?
A) Cardiogenic Shock
B) Early sepsis
C) Pericardial tamponade
D) Pulmonary embolism
E) Volume depletion
Correct Answer:
Verified
Q9: A 32-year-old woman, gravida 1 para 0,
Q10: A 34-year-old man is brought to the
Q11: A 66-year-old retired police officer is brought
Q12: A 36-year-old man comes to the emergency
Q13: A 78-year-old man is brought to the
Q15: A 52-year-old construction worker is brought to
Q16: A 72-year-old man comes to the emergency
Q17: A 39-year-old woman comes to the emergency
Q18: A 68-year-old man comes to the emergency
Q19: A 73-year-old woman comes to the emergency
Unlock this Answer For Free Now!
View this answer and more for free by performing one of the following actions

Scan the QR code to install the App and get 2 free unlocks

Unlock quizzes for free by uploading documents