A 24-year-old man with sickle cell disease (hemoglobin SS) comes to the emergency department with chest pain and shortness of breath. He has felt unwell for the last several days with increasing extremity, abdominal, and chest pain. The patient took extra doses of oral morphine with little relief. He stopped taking hydroxyurea 4 months ago due to stomach upset.
His blood pressure is 122/72 mm Hg, pulse is 108/min, respirations are 22/min, and oxygen saturation is 84% on room air. Bilateral crackles are heard on chest auscultation. A 2/6 midsystolic murmur is heard at the left upper sternal border. The abdomen is diffusely tender without rebound. There is no swelling of the extremities.
Laboratory results are as follows: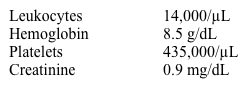
Chest x-ray reveals bilateral dense infiltrates involving both upper and lower right lung fields and the lower left lung field. Intravenous fluids, supplemental oxygen, and antibiotics are initiated.
Which of the following is the best next step in management of this patient?
A) Exchange transfusion
B) Glucocorticoid therapy
C) Hydroxyurea
D) Naloxone
E) Noninvasive ventilation
Correct Answer:
Verified
Q90: A 36-year-old woman comes to the emergency
Q91: A 19-year-old man from Arizona is brought
Q92: A 31-year-old man comes to the emergency
Q93: A 37-year-old woman comes to the emergency
Q94: A 27-year-old woman comes to the emergency
Q96: A 60-year-old woman comes to the emergency
Q97: A 61-year-old woman comes to the emergency
Q98: A 67-year-old man comes to the emergency
Q99: A 62-year-old man is brought to the
Q100: A 50-year-old man is brought to the
Unlock this Answer For Free Now!
View this answer and more for free by performing one of the following actions

Scan the QR code to install the App and get 2 free unlocks

Unlock quizzes for free by uploading documents