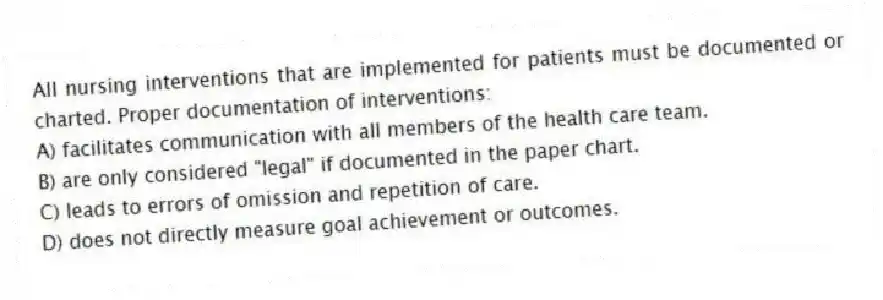
All nursing interventions that are implemented for patients must be documented or charted. Proper documentation of interventions:
A) facilitates communication with all members of the health care team.
B) are only considered "legal" if documented in the paper chart.
C) leads to errors of omission and repetition of care.
D) does not directly measure goal achievement or outcomes.
Correct Answer:
Verified
Q3: The nurse is assisting a patient to
Q10: A patient with a congenital heart defect
Q12: The charge nurse is discussing a patient's
Q13: The nurse writes a short-term goal for
Q15: The nurse is caring for a patient
Q16: The nursing process is cyclic rather than
Q18: The nursing student is caring for a
Q19: The nurse makes the following entry on
Q21: The nurse develops a list of nursing
Q22: Establishing short- and long-term goals to address
Unlock this Answer For Free Now!
View this answer and more for free by performing one of the following actions

Scan the QR code to install the App and get 2 free unlocks

Unlock quizzes for free by uploading documents