A 72-year-old woman is found to be severely short of breath at her skilled nursing facility. The patient was recently hospitalized for vertebral osteomyelitis and discharged 2 weeks ago to complete a 6-week course of piperacillin-tazobactam via a peripherally inserted central venous catheter. Her dyspnea began only with exertion but is now also present at rest. Medical history includes coronary artery disease with ischemic cardiomyopathy, chronic obstructive pulmonary disease, and chronic kidney disease. She has had 2 hospitalizations for heart failure over the last year; noninvasive positive-pressure ventilation was required. Paramedics observe the patient to be obtunded with agonal respirations and rales throughout the bilateral lung fields. Oxygen saturation is 72% on room air. She is intubated and transferred to the emergency department. On arrival, the patient is minimally responsive to stimuli. Temperature is 36.7 C (98 F) , blood pressure is 115/65 mm Hg, and pulse is 110/min and regular. The patient's oxygen saturation is 88% on 100% inspired oxygen. BMI is 19 kg/m2. The trachea is midline. On physical examination, rales are heard on the right side and markedly decreased breath sounds on the left side of the chest. S3 is heard. There is 2+ bilateral peripheral edema. A chest x-ray reveals the following: 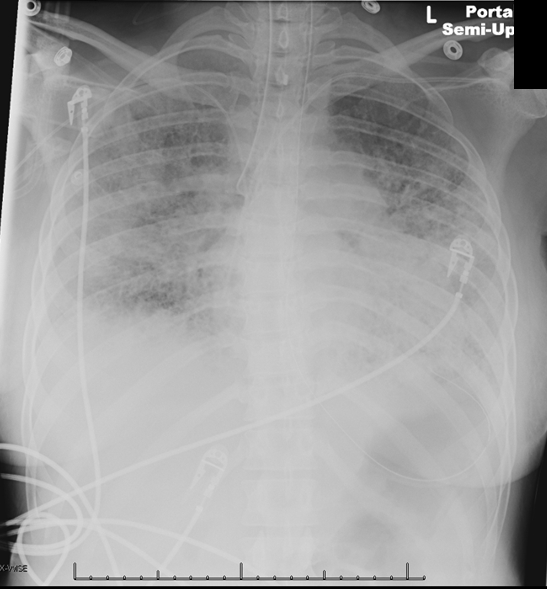 After the intervention is performed, the patient's oxygenation improves. She is transferred to the medical intensive care unit and treated with diuretics and bronchodilators. Two days later, her ventilation requirements have improved to 50% inspired oxygen and 5 cm of positive end-expiratory pressure. The patient's respirations suddenly become dys-synchronous with the ventilator, and her oxygen saturation drops to 85%. Tidal volume spontaneously decreases from 350 to 200 mL. Temperature is 37.2 C (99 F) , blood pressure is 125/60 mm Hg, pulse is 110/min, and respirations are 25/min. Physical examination shows that the trachea is midline and the endotracheal tube is in place. No jugular venous distension is present. Breath sounds are markedly decreased on the right side. A portable chest x-ray reveals the following:
After the intervention is performed, the patient's oxygenation improves. She is transferred to the medical intensive care unit and treated with diuretics and bronchodilators. Two days later, her ventilation requirements have improved to 50% inspired oxygen and 5 cm of positive end-expiratory pressure. The patient's respirations suddenly become dys-synchronous with the ventilator, and her oxygen saturation drops to 85%. Tidal volume spontaneously decreases from 350 to 200 mL. Temperature is 37.2 C (99 F) , blood pressure is 125/60 mm Hg, pulse is 110/min, and respirations are 25/min. Physical examination shows that the trachea is midline and the endotracheal tube is in place. No jugular venous distension is present. Breath sounds are markedly decreased on the right side. A portable chest x-ray reveals the following: Which of the following is the best next step in management of this patient?
Which of the following is the best next step in management of this patient?
A) Decrease the level of sedation
B) Disconnect the ventilator from the endotracheal tube and provide bag ventilation
C) Increase the level of positive end-expiratory pressure
D) Perform needle decompression on the right side of the chest
E) Prepare to insert a chest tube on the right
Correct Answer:
Verified
Q936: A 72-year-old man is evaluated in his
Q937: A 16-year-old boy comes to the office
Q938: A 68-year-old man with chronic obstructive pulmonary
Q939: A 6-month-old boy is brought to the
Q940: A 55-year-old man comes to the emergency
Q942: A 60-year-old man with a history of
Q943: A 40-year-old woman is brought to the
Q944: A 40-year-old woman is brought to the
Q945: A 61-year-old Caucasian female presents to her
Q946: A 59-year-old man comes to the office
Unlock this Answer For Free Now!
View this answer and more for free by performing one of the following actions

Scan the QR code to install the App and get 2 free unlocks

Unlock quizzes for free by uploading documents