A 42-year-old woman comes to the emergency department due to shortness of breath. Approximately 2 weeks ago, the patient developed shortness of breath on exertion that has become progressively worse. She also reports mild chest pain with deep inspiration. She has had no weight loss, fever, cough, or sputum production. Medical history includes diet-controlled type 2 diabetes mellitus and locally advanced infiltrating ductal carcinoma of the left breast, for which she underwent neoadjuvant chemotherapy followed by surgical resection and radiation approximately 2 years ago. The patient is a lifetime nonsmoker and has no significant second-hand tobacco exposure. She lives with her family and works as a teacher. Family history is notable for colon cancer in her father.
Temperature is 37.6 C (99.7 F) , blood pressure is 122/78 mm Hg, pulse is 92/min, and respirations are 20/min. Oxygen saturation is 92% on ambient air. Physical examination shows moist mucous membranes with no jugular venous distension or lymphadenopathy. Heart rate is regular with no murmurs or gallops. Auscultation reveals decreased breath sounds over the right lower lung with dullness to percussion. Extremities have no edema. The remainder of the examination is normal. Upright chest x-ray reveals the following: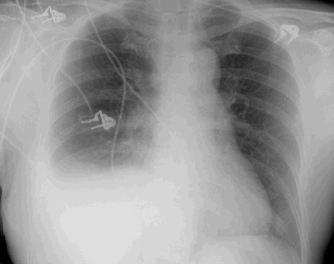
The patient undergoes thoracentesis. Pleural fluid analysis shows 3,500/mm3 nucleated cells, predominantly lymphocytes. Additional pleural fluid analysis results are as follows: Gram stain and culture of the pleural fluid are negative. What is the most appropriate next step in management of this patient?
Gram stain and culture of the pleural fluid are negative. What is the most appropriate next step in management of this patient?
A) Bronchoscopy with bronchoalveolar lavage
B) CT scan of the chest with contrast
C) Nonsteroidal anti-inflammatory agent and clinical follow-up
D) Oral antibiotic and clinical follow-up
E) Thorascopic pleural biopsy
Correct Answer:
Verified
Q77: A 72-year-old man is brought to the
Q78: A 36-year-old woman comes to the emergency
Q79: A 20-year-old African American woman with sickle
Q80: A 19-year-old man comes to the emergency
Q81: A 67-year-old man is brought to the
Q83: An 82-year-old nursing home resident with a
Q84: A 23-year-old woman with known sickle cell
Q85: A 22-year-old woman comes to the emergency
Q86: A 54-year-old woman who recently received a
Q87: A 28-year-old man comes to the emergency
Unlock this Answer For Free Now!
View this answer and more for free by performing one of the following actions

Scan the QR code to install the App and get 2 free unlocks

Unlock quizzes for free by uploading documents