A 68-year-old man comes to the emergency department with a 3-week history of progressive dyspnea, orthopnea, and lower extremity edema. His past medical history is significant for hypertension, type 2 diabetes mellitus, myocardial infarction 8 years ago, and congestive heart failure. Current medications include metoprolol, digoxin, enalapril, furosemide, spironolactone, and aspirin. His blood pressure is 135/80 mm Hg, and pulse is 75/min and regular. Symmetric 2+ pitting edema of the lower extremities is present. Point of maximal impulse is displaced to the left and a soft holosystolic murmur is heard at the apex. Bilateral crackles are present over the lower lobes. Laboratory results are as follows: 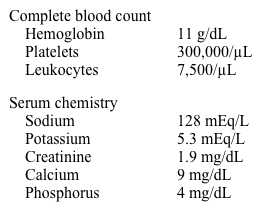 Electrocardiogram shows normal sinus rhythm and no acute ischemic changes. Which of the following is most likely accurate regarding this patient's condition?
Electrocardiogram shows normal sinus rhythm and no acute ischemic changes. Which of the following is most likely accurate regarding this patient's condition?
A) Hyponatremia indicates severe heart failure
B) Increasing sodium intake will help to control the electrolyte abnormalities
C) Increasing the dose of digoxin may be indicated
D) Serum norepinephrine level is low
E) The combination of furosemide and enalapril is the cause of hyperkalemia
Correct Answer:
Verified
Q824: A study was conducted to assess the
Q825: A 54-year-old male with a past medical
Q826: An 80-year-old woman comes to the office
Q827: A 69-year-old man is brought to the
Q828: A 32-year-old woman comes to the emergency
Q830: A prospective cohort study was conducted to
Q831: A 45-year-old mildly overweight man recovering from
Q832: A 52-year-old man comes to the emergency
Q833: A study was conducted to establish the
Q834: A 56-year-old man comes to the emergency
Unlock this Answer For Free Now!
View this answer and more for free by performing one of the following actions

Scan the QR code to install the App and get 2 free unlocks

Unlock quizzes for free by uploading documents