Passage
Myalgic encephalopathy (ME) , or chronic fatigue syndrome (CFS) , is a physiological disease that affects 0.15% of the human population. Compared with healthy individuals, persons with ME experience reduced phospholipid levels, muscular degeneration, urinary urgency, and other symptoms that contribute to a lower quality of life. Studies in resting subjects have yielded inconsistent data and failed to identify a unique metabolic defect in patients with ME.Analyzing the blood plasma of male and female patients with ME, physicians have observed that male patients display elevated levels of 3-methylhistidine, a marker of protein catabolism. Researchers expanded this finding by measuring the serum concentration of amino acids in blood samples obtained from nonfasting ME patients and healthy controls. Amino acids were classified into separate categories according to their metabolic intermediates.Table 1 Classification of Amino Acids in Blood Plasma
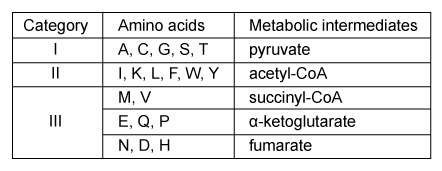
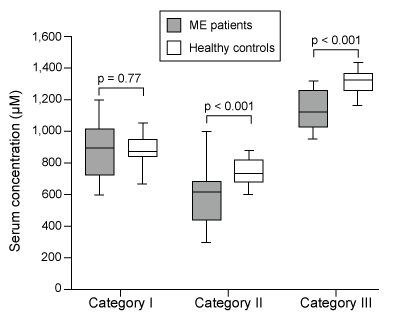 Figure 1 Serum concentrations of amino acids in patients with ME and healthy controls (HC) Next, researchers hypothesized that the inhibition of pyruvate dehydrogenase (PDH) and impairment of fatty acid oxidation were responsible for the fluctuations in amino acid levels. PDH function and lipid metabolism were studied in peripheral blood mononuclear cells (PBMCs) by measuring the gene expression of proteins within regulatory pathways. Researchers monitored the mRNA levels of the inhibitor pyruvate dehydrogenase kinase 1 (PDK1) and of sirtuin 4 (SIRT4) , which removes lipoic acid groups from the PDH complex. They also examined lipid metabolism by measuring the mRNA levels of peroxisome proliferator-activated receptor-α (PPARα) , a transcription factor that upregulates the uptake of fatty acids. The mRNA level of each protein in PBMCs of patients with ME was evaluated against healthy controls, as shown in Figure 2.
Figure 1 Serum concentrations of amino acids in patients with ME and healthy controls (HC) Next, researchers hypothesized that the inhibition of pyruvate dehydrogenase (PDH) and impairment of fatty acid oxidation were responsible for the fluctuations in amino acid levels. PDH function and lipid metabolism were studied in peripheral blood mononuclear cells (PBMCs) by measuring the gene expression of proteins within regulatory pathways. Researchers monitored the mRNA levels of the inhibitor pyruvate dehydrogenase kinase 1 (PDK1) and of sirtuin 4 (SIRT4) , which removes lipoic acid groups from the PDH complex. They also examined lipid metabolism by measuring the mRNA levels of peroxisome proliferator-activated receptor-α (PPARα) , a transcription factor that upregulates the uptake of fatty acids. The mRNA level of each protein in PBMCs of patients with ME was evaluated against healthy controls, as shown in Figure 2.
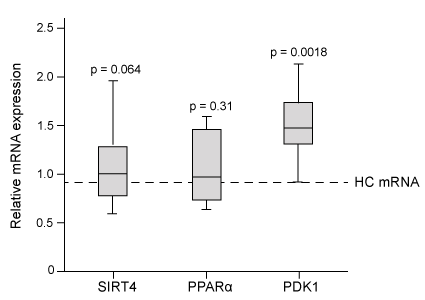 Figure 2 Gene expression of PDK1, SIRT4, and PPARα in PBMCs
Figure 2 Gene expression of PDK1, SIRT4, and PPARα in PBMCs
Adapted from Fluge Ø, Mella O, Bruland O, et al.. JCI Insight. 2016;1(21) :e89376.
-Lipids serve as energy stores for healthy patients and patients with ME. If both groups were fed the same diet, would the rate of lipid synthesis after a meal be faster in healthy individuals or in patients with ME?
A) Patients with ME, because the release of glucagon activates acetyl-CoA carboxylase in the liver
B) Patients with ME, because more chylomicrons are broken down in the bloodstream
C) Healthy individuals, because insulin stimulates the transport of acetyl-CoA to the cytosol
D) Healthy individuals, because fewer fatty acids are being generated by hormone-sensitive lipase
Correct Answer:
Verified
Q81: Passage
Ribulose-1,5-bisphosphate carboxylase/oxygenase (rubisco) is one of the
Q82: Passage
Myalgic encephalopathy (ME), or chronic fatigue syndrome
Q83: Passage
Synthesis of coenzyme A (CoA) requires vitamin
Q84: Passage
Ribulose-1,5-bisphosphate carboxylase/oxygenase (rubisco) is one of the
Q85: If a frameshift mutation changes the number
Q87: Passage
Ribulose-1,5-bisphosphate carboxylase/oxygenase (rubisco) is one of the
Q88: Passage
Synthesis of coenzyme A (CoA) requires vitamin
Q89: Passage
Myalgic encephalopathy (ME), or chronic fatigue syndrome
Q90: Passage
Synthesis of coenzyme A (CoA) requires vitamin
Q91: Two possible mechanisms, shown below, were designed
Unlock this Answer For Free Now!
View this answer and more for free by performing one of the following actions

Scan the QR code to install the App and get 2 free unlocks

Unlock quizzes for free by uploading documents