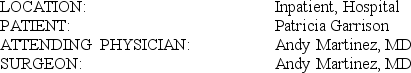
T11-1B OPERATIVE REPORT, CESAREAN SECTION
 PREOPERATIVE DIAGNOSES:
PREOPERATIVE DIAGNOSES:
1. Twin intrauterine pregnancy at 36 weeks 4 days.
2. Vertex/breech combination.
POSTOPERATIVE DIAGNOSES:
1. Twin intrauterine pregnancy at 36 weeks 4 days.
2. Vertex/breech combination.
PROCEDURE PERFORMED: Primary low transverse cesarean section
ANESTHESIA: Spinal
SURGICAL INDICATIONS: The patient is a 26-year-old gravida 2, para (to bring forth) 1, at 36 weeks 4 days who presented in active labor with vertex/breech combination. After counseling with the patient, the decision was made to proceed with delivery by C-section.
OPERATIVE FINDINGS: The first twin weighed 2794 g (gram) and was a male infant, with Apgar scores of 6 at 1 minute and 8 at 5 minutes. The second child was a male weighing 3203 g, with Apgar of 6 at 1 minute and 9 at 5 minutes. There were two separate sacs with fused placenta. The amniotic fluid was clear on both twins. Tubes and ovaries were normal. The appendix was retrocecal.
OPERATIVE DESCRIPTION: After induction of subarachnoid anesthesia, Foley catheter was placed as well as Venodynes, and the patient was then prepped and draped. The abdomen was opened through a Pfannenstiel incision. The bladder flap was opened transversely with scissors and the bladder dissected down bluntly with the hand. A small incision was made in the myometrium of the lower uterine segment, and then entry into the uterus was accomplished bluntly with a Kelly clamp. A finger was introduced into the uterus to guide a bandage scissors for a low transverse incision. The first infant was then delivered without difficulty, and the mouth and nose were suctioned with bulb syringe, cord was clamped and cut, and infant handed to ICN (intensive care; neonatal) staff. The second sac was then ruptured with Allis clamp, and the infant was delivered breech without difficulty. This infant was then suctioned and handed off. The placenta was delivered manually. The cords were tagged appropriately for pathology. Uterus was closed in two layers, first with a running locked 0 Vicryl followed by a running horizontal Lembert 0 Vicryl. The pelvis was irrigated with saline. The uterine incision was reinspected and was felt to be dry. With sponge and needle counts correct, attention was directed toward the closure. The peritoneum was loosely approximated in the midline with three mattress sutures of 2-0 Vicryl. The fascia was then closed with running 0 Vicryl using two strands, one from either side to the middle and tied independently. The skin was closed with staples, and a sterile dressing was applied. Blood loss estimation was difficult due to the large amount of amniotic fluid, but we estimated approximately 1200 cc. Specimen to pathology: Placenta. Final sponge and needle counts were correct.
PATHOLOGY REPORT LATER INDICATED: Benign tissue
T11-1B:
SERVICE CODE(S): ___________________________________________________
ICD-10-CM DX CODE(S): ______________________________________________
Correct Answer:
Verified
Q2: T11-1A OBSTETRICAL ULTRASOUND Q3: T11-2A OPERATIVE REPORT, CESAREAN SECTION Q4: AUDIT REPORT T11.2 DISCHARGE SUMMARY Q5: T11-2B OPERATIVE REPORT, AMNIOCENTESIS Q6: AUDIT REPORT T11.1 OPERATIVE REPORT, CESAREAN
![]()


![]()
SECTION
Unlock this Answer For Free Now!
View this answer and more for free by performing one of the following actions

Scan the QR code to install the App and get 2 free unlocks

Unlock quizzes for free by uploading documents