A 34-year-old woman is brought to the emergency department with acute onset of severe headache followed by generalized tonic-clonic seizures. The patient was feeling well until 6 hours ago, when she developed a 10/10 throbbing bilateral headache associated with blurry vision. Her headache is not exacerbated by change in head position, and nothing seems to improve the pain. She denies any nausea, vomiting, photophobia, vertigo, fever, or neck pain. She also denies any recent head or neck trauma. She has had upper respiratory tract symptoms for the last couple of days.
Her other medical problems include chronic migraines and non-essential hypertension related to renal artery stenosis from fibromuscular dysplasia. Her medications include topiramate and multiple anti-hypertensive agents including amlodipine, hydrochlorothiazide, lisinopril, and metoprolol. She also takes birth control pills and vitamins. She has never had a seizure before and has no family history of epilepsy. She works as a secretary and has smoked 2 packs of cigarettes daily for 10 years.
Her temperature is 37 C (98.6 F) , blood pressure is 210/140 mm Hg, pulse is 80/min and regular, and respirations are 18/min with normal oxygen saturation. The general physical examination is unremarkable, except for an abdominal bruit. Neurological examination reveals that she is awake and alert, but is only oriented to person and place. Funduscopic examination reveals copper and silver wiring in the retina without papilledema. Pupils are equal, round, and reactive to light. Visual acuity is 20/200 bilaterally with intact visual fields to confrontation. There is no nystagmus and extra-ocular movements are full. The remainder of the neurological examination is unremarkable.
A non-contrast head CT showed hypodense regions with loss of grey-white matter differentiation in the posterior occipital-parietal lobes. An MRI of the brain without gadolinium (shown below) showed a symmetrical, increased T2/FLAIR signal abnormality in the subcortical white matter of the posterior occipital-parietal lobes.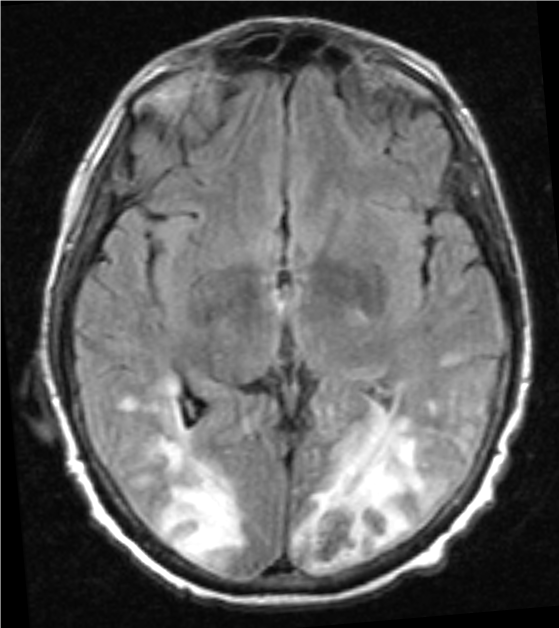
Which of the following is the most likely diagnosis?
A) Aneurysmal subarachnoid hemorrhage
B) Herpes simplex encephalitis
C) Idiopathic intracranial hypertension
D) Migraine headache
E) Posterior reversible encephalopathy syndrome
Correct Answer:
Verified
Q117: A 23-year-old woman is brought to the
Q118: A previously healthy 24-year-old woman comes to
Q119: A 43-year-old man with a history of
Q120: A 68-year-old man is brought to the
Q121: A 45-year-old woman is brought to the
Q123: A 40-year-old man comes to the emergency
Q124: A 21-year-old woman comes to the emergency
Q125: A 65-year-old man comes to the emergency
Q126: A 65-year-old man is brought to the
Q127: A 65-year-old man is brought to the
Unlock this Answer For Free Now!
View this answer and more for free by performing one of the following actions

Scan the QR code to install the App and get 2 free unlocks

Unlock quizzes for free by uploading documents