A 65-year-old woman comes to the office reporting progressively increasing orthopnea, daytime fatigue, and morning headache for the last month. She has had no chest pain or problems with swallowing or speech. Medical conditions include myocardial infarction, type 2 diabetes, hypertension, and amyotrophic lateral sclerosis. Temperature is 37 C (98.6 F) , blood pressure is 130/70 mm Hg, pulse is 88/min, and respirations are 16/min. Pulse oximetry shows 95% on room air. BMI is 24 kg/m2. Examination shows normal jugular venous pressure, clear lungs, and normal heart sounds. There is no peripheral edema. Neurologic examination shows 3/5 power in right lower extremity and 4/5 power in left lower extremity and muscle atrophy, unchanged from her last examination 2 months ago. Laboratory results are as follows: 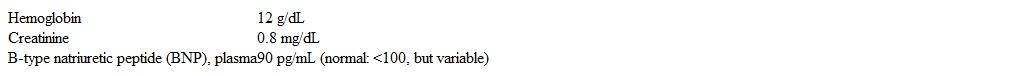 Which of the following is the most appropriate next step in management?
Which of the following is the most appropriate next step in management?
A) Furosemide
B) Home oxygen therapy
C) Modafinil
D) Noninvasive positive-pressure ventilation
E) Tiotropium
F) Tracheostomy
Correct Answer:
Verified
Q1680: A 75-year-old woman is evaluated for agitation
Q1681: A 75-year-old man comes to the office
Q1682: A 23-year-old woman with a history of
Q1683: A 33-year-old woman comes to the office
Q1684: A 32-year-old woman is brought to the
Q1686: A 52-year-old man comes to the office
Q1687: A 27-year-old woman comes to the office
Q1688: A 35-year-old woman is evaluated due to
Q1689: A 34-year-old man comes to the office
Q1690: A 42-year-old man with HIV infection who
Unlock this Answer For Free Now!
View this answer and more for free by performing one of the following actions

Scan the QR code to install the App and get 2 free unlocks

Unlock quizzes for free by uploading documents