A 76-year old man is admitted because of cough, fever, and shortness of breath. His medical problems include type 2 diabetes mellitus and hypertension.
His blood pressure is 105/60 mm Hg, pulse is 110/min and regular, and respirations are 30/min. His oxygen saturation is 85% on room air. On examination, he had crackles at the right lower lung base. Chest x-ray showed a dense right lower lobe infiltrate. He was started on antibiotics.
Over the following 24 hours, he developed progressive respiratory failure requiring endotracheal intubation and mechanical ventilation. His antibiotic coverage was broadened. Bilateral crackles are heard on chest examination. Extremities are warm with bounding pulses.
Chest x-ray shows bilateral infiltrates involving both the upper and lower lungs. The current ventilator settings are as follows: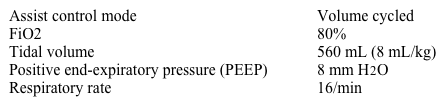
Arterial blood gas analysis shows pH 7.30, pCO2 49 mm Hg, and pO2 48 mm Hg.
Which of the following is the best next step in managing this patient?
A) Increase FiO2
B) Increase positive end-expiratory pressure
C) Increase respiratory rate
D) Increase tidal volume
E) Switch to a pressure cycled ventilation mode
Correct Answer:
Verified
Q78: A 55-year-old man comes to the physician
Q79: A 53-year-old woman is brought to the
Q80: A 35-year-old woman comes to the emergency
Q81: A 63-year-old hospitalized woman develops severe shortness
Q82: A 52-year-old man with alcoholic cirrhosis is
Q84: An 89-year-old man is hospitalized because of
Q85: A 73-year-old smoker is brought to the
Q86: A 63-year-old man is hospitalized with dyspnea
Q87: A 55-year-old man is evaluated for acute
Q88: A 74-year-old woman is brought to the
Unlock this Answer For Free Now!
View this answer and more for free by performing one of the following actions

Scan the QR code to install the App and get 2 free unlocks

Unlock quizzes for free by uploading documents