A 76-year-old man comes to the physician due to a several-week history of fatigue and lethargy. He lives in an assisted living facility and takes naps during the day but still feels exhausted in the evening. The patient does not use tobacco or alcohol. His medical problems include hypertension, type 2 diabetes mellitus, coronary artery disease, and ischemic cardiomyopathy. He also underwent coronary artery bypass grafting 5 years ago.
The patient was hospitalized 4 months ago with dizziness, palpitations, and near-syncope and was diagnosed with monomorphic ventricular tachycardia. He underwent electrical cardioversion and was started on amiodarone and high-dose metoprolol. Laboratory workup during that time was unremarkable, and his echocardiogram showed a left ventricular ejection fraction of 25%. An automated implantable cardioverter-defibrillator (AICD) was implanted before discharge. The last device interrogation 4 weeks ago showed multiple episodes of non-sustained ventricular tachycardia but no defibrillator shocks.
His blood pressure is now 140/90 mm Hg and pulse is 62/min and regular. The patient has normal jugular venous pressure. There is no thyromegaly. Lung fields are clear to auscultation. A faint mid-systolic murmur is heard at the left sternal border. There is 1+ peripheral edema bilaterally and his skin is dry. Deep tendon reflexes are diminished bilaterally. Laboratory studies are shown below: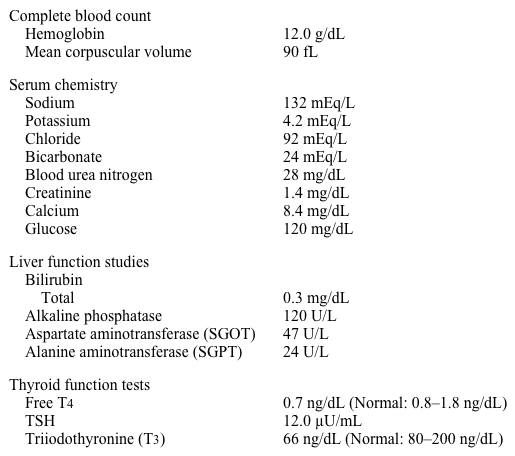
Which of the following is the best next step in managing this patient?
A) Check anti-thyroid peroxidase (anti-TPO) antibodies
B) Continue amiodarone and start levothyroxine
C) Discontinue amiodarone and repeat thyroid function tests in a few weeks
D) Discontinue amiodarone and start levothyroxine
E) Order thyroid ultrasound
Correct Answer:
Verified
Q212: A 30-year-old woman comes to the office
Q213: A 35-year-old man comes to the office
Q214: A 45-year-old man comes to the office
Q215: A 27-year-old woman comes to the physician
Q216: A 45-year-old woman comes to the physician
Q218: A 29-year-old woman comes to the physician
Q219: A 46-year-old man comes to the office
Q220: A 42-year-old man comes to the physician
Q221: A 49-year-old woman comes to the clinic
Q222: A 72-year-old man with a seven-year history
Unlock this Answer For Free Now!
View this answer and more for free by performing one of the following actions

Scan the QR code to install the App and get 2 free unlocks

Unlock quizzes for free by uploading documents