A 62-year-old hospitalized man is evaluated for new-onset, right lower extremity pain. The patient underwent bypass surgery for 3-vessel coronary artery disease 2 months ago. He arrived at the emergency department 2 nights ago due to recurrent chest pains. At that time, ECG showed sinus rhythm with no ST-segment changes, but cardiac troponin I levels were elevated. The patient was initiated on unfractionated heparin, antiplatelet agents, a beta blocker, and a nitrate. A coronary angiogram was performed via the radial artery; it revealed graft insertion site stenosis and was treated with stenting. Postintervention echocardiography revealed left ventricular ejection fraction of 50% with no regional wall motion abnormalities. This morning, the patient had new, sudden-onset, right lower extremity pain. He has never had pain in that extremity before. The patient has a history of hypertension, hyperlipidemia, and type 2 diabetes mellitus. Current medications include aspirin, clopidogrel, rosuvastatin, metoprolol, losartan, isosorbide mononitrate, basal-bolus insulins, and subcutaneous heparin at a prophylactic dose. The patient is a former smoker with a 30-pack-year history. Temperature is 37.6 C (99.7 F) , blood pressure is 138/84 mm Hg, pulse is 96/min, and respirations are 18/min. Physical examination reveals normal jugular venous pressure, clear lungs, no heart murmurs, and a soft, nontender abdomen. The right leg is tender and cool to the touch when compared to the left leg. Right lower extremity distal pulses are diminished, but capillary refill is intact. Left leg examination is normal with the exception of healed scars from previous saphenous vein harvesting. Neurological examination is normal. Laboratory results are as follows: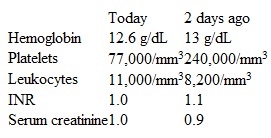
Which of the following is the most likely cause of this patient's leg pain?
A) Acute ulceration and thrombosis of a peripheral artery atheroma
B) Arterial embolization of a left ventricular thrombus
C) Autoantibodies directed against heparin-platelet factor 4 complexes
D) Embolization of cholesterol crystals from an atherosclerotic plaque
E) Uncontrolled activation of coagulation and fibrinolytic cascades
Correct Answer:
Verified
Q436: A 33-year-old woman comes to the office
Q437: A 16-year-old boy is brought to the
Q438: A 35-year-old Caucasian man is seen in
Q439: A 54-year-old man comes to the emergency
Q440: A 65-year-old man is brought to the
Q442: A 54-year old Caucasian man comes to
Q443: A 68-year-old woman comes to the office
Q444: A 67-year-old man comes to the physician
Q445: A 62-year-old hospitalized man is evaluated for
Q446: Imaging studies show the presence of colonic
Unlock this Answer For Free Now!
View this answer and more for free by performing one of the following actions

Scan the QR code to install the App and get 2 free unlocks

Unlock quizzes for free by uploading documents