A 67-year-old woman comes to the emergency department due to increased dyspnea on exertion. Her chronic medical problems include obesity, obstructive sleep apnea, moderate chronic obstructive pulmonary disease, coronary artery disease, congestive heart failure, hypertension, hyperlipidemia, rheumatoid arthritis, and hypothyroidism. She was treated with antibiotics and a steroid taper for a "lung infection" 1 month ago. Her cough productive of thick yellowish sputum improved, but she has been feeling increasingly dyspneic when walking up stairs and doing her grocery shopping over the past week. She took some extra doses of furosemide with minimal relief.
The patient denies increased orthopnea but says, "I always sleep on 3 pillows so I can avoid using that PAP mask." She has no fever, chills, or night sweats. She smokes half a pack of cigarettes a day. Surgical history is significant for a 3-vessel coronary artery bypass graft 5 years ago.
Her blood pressure is 160/96 mm Hg, pulse is 78/min, and respirations are 20/min. Pulse oximetry shows 96% on room air. Her BMI is 36 kg/m2. Physical examination shows mild respiratory distress. Lung examination reveals decreased breath sounds on the right with dullness to percussion almost halfway up. There is 1+ pitting edema up to the knees bilaterally.
Laboratory results are as follows: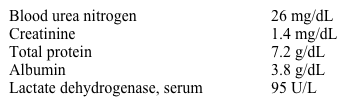
Chest x-ray reveals blunting of the costophrenic angle on the left and a moderate right-sided pleural effusion. Thoracentesis is performed on the right and 750 mL of serous fluid is removed. The results of pleural fluid analysis are as follows: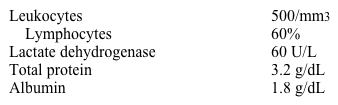
Which of the following is the most likely cause of her pleural effusion?
A) Congestive heart failure
B) Malignant pleural effusion
C) Parapneumonic effusion
D) Pulmonary embolism
E) Rheumatoid pleurisy
Correct Answer:
Verified
Q180: A 54-year-old man with a history of
Q181: An 85-year-old nursing home resident is brought
Q182: A 72-year-old man with metastatic prostate cancer
Q183: A 67-year-old man with chronic obstructive pulmonary
Q184: A 75-year-old man with moderate chronic obstructive
Q186: A 62-year-old woman comes to the emergency
Q187: A 46-year-old woman comes to the emergency
Q188: A 28-year-old woman comes to the emergency
Q189: A 62-year-old man comes to the emergency
Q190: A 53-year-old man comes to the emergency
Unlock this Answer For Free Now!
View this answer and more for free by performing one of the following actions

Scan the QR code to install the App and get 2 free unlocks

Unlock quizzes for free by uploading documents