A 60-year-old woman is brought to the hospital for fever, chills, productive cough, and worsening shortness of breath. These symptoms began 3 days ago but have worsened over the last 24 hours. Her other medical problems include type 2 diabetes, hypertension, and psoriatic arthritis. Her medications include methotrexate, metformin, glyburide, lisinopril, and hydrochlorothiazide. She has a 20-pack-year smoking history.
The patient's temperature is 39.3 C (102.7 F) , blood pressure is 110/70 mm Hg, pulse is 112/min, and respirations are 22/min. Oxygen saturation is 90% on room air. Examination shows mild respiratory discomfort with crackles over the right lower lung field. The remainder of the examination shows no significant abnormalities.
The patient is admitted to the hospital and started on intravenous antibiotics and normal saline at 150 mL/hr. Over the next 12 hours, she develops worsening shortness of breath and hypotension requiring transfer to the intensive care unit. Her blood pressure is 80/50 mm Hg, respirations are 36/min, and oxygen saturation is 82% on 100% oxygen. She is intubated emergently. Repeat chest x-ray, in the image below, shows diffuse bilateral airspace disease. Laboratory results are as follows: pH 7.38, PaCO2 39 mm Hg, and PaO2 61 mm Hg on FIO2 of 100%.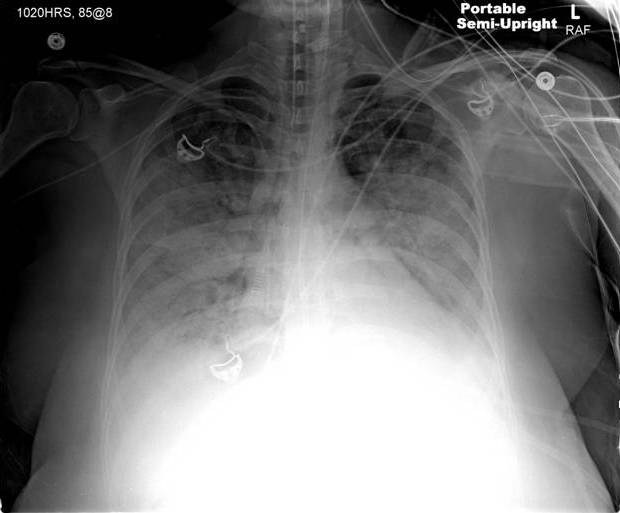
Which of the following is most likely to improve this patient's prognosis?
A) High-frequency ventilation
B) Low positive end-expiratory pressure
C) Low tidal volume ventilation
D) Maintenance of low PaCO2
E) Use of inotropic agents with invasive cardiac output monitoring
Correct Answer:
Verified
Q95: A 43-year-old man with alcoholic pancreatitis is
Q96: A 36-year-old woman comes to the emergency
Q97: A 65-year-old woman with a history of
Q98: A 63-year-old man with chronic obstructive pulmonary
Q99: A 65-year-old woman with a history of
Q101: A 64-year-old woman was found poorly responsive
Q102: A 48-year-old man comes to the emergency
Q103: A 48-year-old man is admitted to the
Q104: A 25-year-old woman being treated for infective
Q105: A 47-year-old man is hospitalized due to
Unlock this Answer For Free Now!
View this answer and more for free by performing one of the following actions

Scan the QR code to install the App and get 2 free unlocks

Unlock quizzes for free by uploading documents